Bone health tumbles with hip fractures rising
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

If you’re over 65, you’re probably worried about having a heart attack, or being diagnosed with breast or prostate cancer. But you’re actually much more likely to have osteoporosis, a
disease that weakens bone and increases the risk of fracture. In fact, about 10 percent of Americans age 50 and older have osteoporosis and another 43 percent have osteopenia, or low bone
density_._ And with osteoporosis, you’re much more at risk of suffering a hip fracture, which can prevent you from living independently and may sometimes even be deadly. Now, new research
suggests that hip fracture rates in older women are on the rise. In a study published this month in _Osteoporosis International_, researchers looked at Medicare claims of women age 65 and
older from 2002 to 2015. They found that rates declined until 2012. In 2013 hip fracture rates were higher than had been expected, a concern since they are expensive and associated with a
loss of independence and even death. “As a result, we ended up with over 11,000 additional hip fractures from 2013 to 2015,” says study author E. Michael Lewiecki, M.D., director of the New
Mexico Clinical Research & Osteoporosis Center in Albuquerque. There are several reasons for the uptick in fractures, he says. Since Medicare reimbursement rates for bone density testing
have gone down over the last several years, some screening facilities have actually closed down, leading to fewer people getting checked. But the main — and more concerning — reason is many
people have stopped taking bone density medications. In fact, use of these drugs dropped from 15 percent in 2004 to just 3 percent in 2013. “It’s a real crisis point in osteoporosis
treatment,” says Sundeep Khosla, M.D., an osteoporosis specialist at the Mayo Clinic in Minnesota. “Many people have been scared away from taking these drugs after reports of very rare side
effects, including thigh fractures and breakdown of bone in the jaw. As a result, many who should be on them aren’t — and we’re seeing rising fracture rates as a result.” Here are the four
things osteoporosis experts say you need to do to help keep your bones strong and reduce your risk of fracture, either now or later. GET SCREENED You know your blood pressure and cholesterol
numbers, and you should know your bone density, too. Every woman should have a baseline screening at age 65, and men should have one at age 70, says Khosla. But you may need to have one
earlier if you have risk factors such as a strong family history of osteoporosis, rheumatoid arthritis and are on certain medications such as steroids, and if you smoke or consume more than
three alcoholic drinks a day. Having suffered a past low impact fracture such as falling and breaking your wrist also puts you at greater risk. You should also discuss possible earlier
screening with your physician if you regularly take a type of anti-depressant known as selective serotonin reuptake inhibitors (SSRIs), such as sertraline (Zoloft and generic), or a type of
anti-anxiety medication known as benzodiazepines, such as diazepam (Valium and generic). Both appear to significantly increase risk of having an osteoporotic fracture, according to a study
published recently in _JAMA Psychiatry_. If you don’t have any risk factors, it’s fine to wait until age 65, says Khosla. If your bone density is found to be normal (defined as a T-score -1
or better), you don’t have to have another test for a decade. If you have osteopenia, or low bone density (defined as a T-score between -1 and -2.5), you should have a follow-up scan
sometime between three and five years, and if you have osteoporosis (with a T-score -2.5 and below), you’ll need repeat testing every two years. Try to have follow-up scans done at the same
facility, as bone density measurements are easier to compare if they have been taken on the same model. EAT THE RIGHT FOODS Women over age 50 and men over age 70 need about 1200 mg of
calcium a day, ideally from food, according to the National Osteoporosis Foundation. A cup of milk has 300 mg, while a 6-ounce serving of low fat yogurt has about 260 mg; 3 ounces of canned
salmon has around 180 mg, and a cup of cooked broccoli has 60 mg. “It’s still essential to get this total amount, since we lose calcium every day in urine and in our intestines and need to
replace it,” explains Lewiecki. Vitamin D is also important, since it helps your body absorb calcium. While the NOF recommends men and women over age 50 get 800-1000 IU worth, “it’s a good
idea to have your doctor check your Vitamin D levels," says Ethel Siris, M.D., director of the Toni Stabile Osteoporosis Center at the Columbia University Medical Center. If you’re low
— under 30 ng/mL — you may want to talk to your doctor about supplementing to obtain a higher level, she says. (Vitamin D is only found in a few foods, like fortified milk or orange juice or
fatty fish like salmon.) And bone up on as many fresh fruits and veggies as you can; these foods are rich in potassium and magnesium, both of which have been linked to better bone mass in
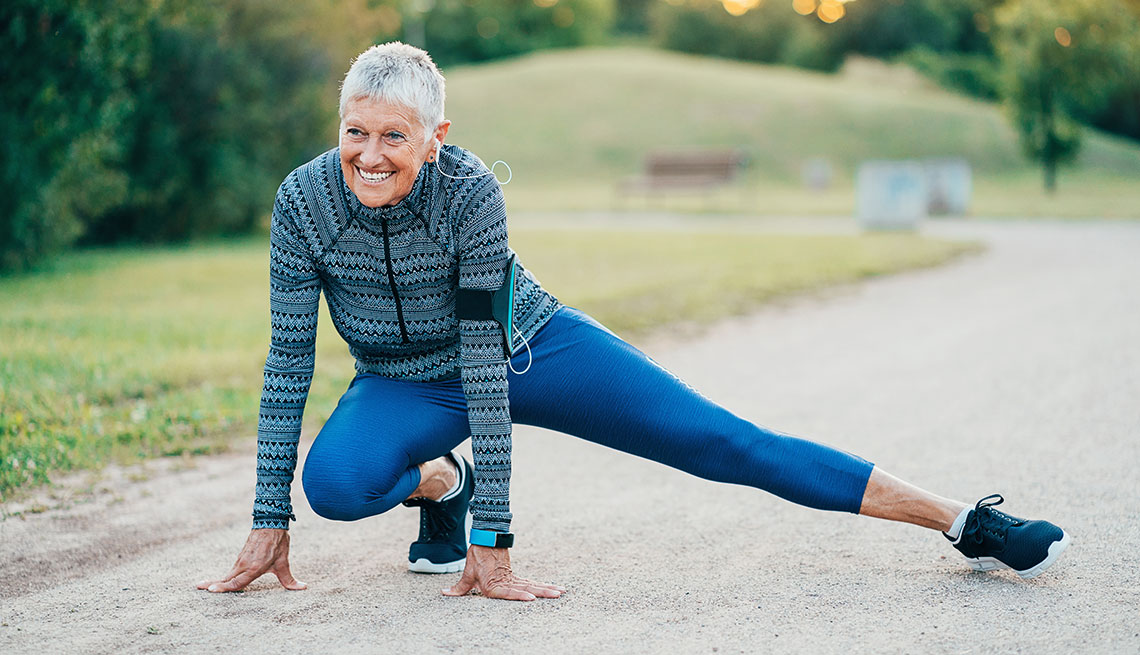
people. AMP UP YOUR EXERCISE
