Relationship between refraction and allergic conjunctivitis
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT PURPOSE External allergens are the main causative factor in the pathogenesis of allergic diseases; however, little is known about internal factors such as the biometrical structure
of the eye. We investigated the relationship between refractive error and allergic conjunctivitis in order to reveal possible insights into the pathogenesis in 1015 subjects. METHODS The
patients were divided into four groups: contact lens wearers with allergic conjunctivitis (_n_=73), contact lens wearers without allergic conjunctivitis (_n_=59), non-contact lens wearers
with allergic conjunctivitis (_n_=224), and non-contact lens wearers without allergic conjunctivitis (_n_=659). The spherical power, cylindrical power, corneal radius, and minimum and
maximum corneal refractive powers were measured in all subjects. RESULTS In the non-contact lens wearers, the spherical equivalent and spherical power were significantly lower in patients
with allergic conjunctivitis than in patients without allergic conjunctivitis (−3.01±3.83 D _vs_−1.36±3.08 D, _P_<0.0001, and −2.64±3.63 D _vs_−1.05±2.88 D, _P_<0.0001, respectively),
while there was no significant difference in any of the parameters between the contact lens wearers with and without allergic conjunctivitis. CONCLUSION Refractive error may be a risk factor
for allergic conjunctivitis. SIMILAR CONTENT BEING VIEWED BY OTHERS INCREASED RISK OF CATARACT SURGERY IN PATIENTS WITH ALLERGIC DISEASE: A POPULATION BASED COHORT STUDY Article Open access
08 December 2022 EVALUATION ON THE CLINICAL FINDINGS AND ALLERGOLOGICAL FACTORS OF LOCAL ALLERGIC CONJUNCTIVITIS AND NON-LOCAL ALLERGIC CONJUNCTIVITIS Article Open access 12 April 2025
ATOPIC DISEASE AND ASTIGMATISM: A POPULATION-BASED STUDY Article Open access 28 February 2025 INTRODUCTION In recent years, the increasing number of cases of allergic diseases has resulted
in a growing social concern. A prevalent idea is that hypersensitivity responses to external allergens such as pollen and house dust are the main causative factors in the development of
allergic diseases.1, 2 However, little attention has been given to the internal factors such as the biometrical structure of the eye. This paper introduces the novel concept that refractive
error could be responsible for allergic conjunctivitis. MATERIALS AND METHODS SUBJECT This study was performed in accordance with the Helsinki's Declaration of 1975 and its 1983
revision. Institutional Review Board approval and a written informed consent were obtained from each subject. The consecutive patients visiting our outpatient clinic between September 2003
and August 2004 were selected for this study. The subjects were classified into four groups: contact lens wearers with seasonal allergic conjunctivitis (SAC) (73 eyes of 73 patients),
contact lens wearers without SAC (59 eyes of 59 patients), non-contact lens wearers with SAC (224 eyes of 224 patients), and non-contact lens wearers without SAC (659 eyes of 659 patients).
We excluded participants with a previous history of cataract surgery, corneal refractive surgery, and vernal keratoconjunctivitis. Thus, 1015 patients were included in the present study.
AUTOREFRACTIVE MEASURES As part of our standardized examination, an automated objective refraction test was performed on each participant with an autokeratorefractometer (KR 3000, TOPCON,
Yamagata, Japan). The spherical power, cylindrical power, corneal radius, and minimum and maximum corneal refractive power were measured. The spherical equivalent (sphere+1/2 cylinder) was
used to calculate the refractive error. Both the right and left eyes were measured; however, only the right eye was used for analysis purposes. DEFINITION OF SEASONAL ALLERGIC CONJUNCTIVITIS
Seasonal allergic conjunctivitis was diagnosed by slit-lamp examination by identification of clinical symptoms such as conjunctival follicle, papillae, and redness, and seasonal symptoms
such as ocular itching and tearing without proliferative lesions according to the guidelines of diagnosis and treatment of conjunctivitis.3 STATISTICAL ANALYSIS Unpaired Student's
_t_-tests were used to compare the mean values. _χ_2 tests were used to compare the difference in proportions between the two groups. The level of significance was set at _P_<0.05. The
calculations were carried out using the Stat View statistical software package (Abacus Concepts, Berkeley, CA, USA). RESULTS The characteristics of the study population are presented in
Table 1. The proportion of contact lens wearers was higher in patients with SAC than in patients without SAC (24.6 _vs_ 8.2%, _χ_2=49.71, _P_<0.0001). The mean spherical equivalent of the
refractive error and spherical power were significantly lower in patients with SAC than in patients without SAC (−3.62±3.76 D _vs_ −1.69±3.25 D, _P_<0.0001, −3.23±3.56 D _vs_ −1.37±3.06
D, _P_<0.0001, respectively, unpaired _t_-test). In the non-contact lens wearers, significant differences were found in spherical equivalent (−3.01±3.83 D _vs_ −1.36±3.08 D,
_P_<0.0001) and spherical power (−2.64±3.63 D _vs_ −1.05±2.88 D, _P_<0.0001) between patients with and without SAC. On the contrary, no significant difference was found in cylindrical
power, corneal radius, and minimum and maximum corneal refractive power between patients with and without SAC (Table 1). In the contact lens wearers, no statistically significant differences
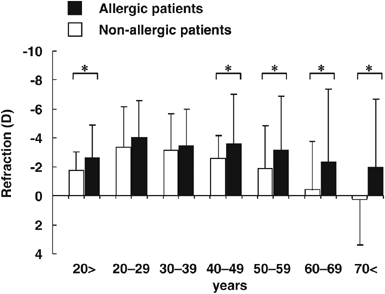
were noted in any of the parameters between patients with and without SAC (Table 1). In the non-contact lens wearers, the mean spherical equivalent refraction, shown in Figure 1, was lower
in patients with SAC than in patients without SAC (_P_<0.05), except for the group aged between 20 and 39 years. In all patients including contact wearers, similar results were obtained
(Figure 2). DISCUSSION The relationship between eye shape and allergic conjunctivitis has not been studied so far. Initial studies were conducted to compare the prevalence of allergic
conjunctivitis between the contact and non-contact lens wearers. The prevalence of allergic conjunctivitis was higher in the contact lens wearers than in the non-contact lens wearers. This
result suggests that allergic conjunctivitis occurs more frequently in the contact lens wearers, as reported previously.4 Next, we attempted to investigate the relationship between the
refraction of the eye and allergic conjunctivitis in the non-contact lens wearers to minimize the influence of contact lens-associated conjunctivitis. In the non-contact lens wearers, the
mean spherical equivalent and spherical power were significantly lower in patients with SAC than in patients without SAC. In addition, our refraction data pertaining to the non-contact lens
wearers without SAC were in excellent agreement with the refraction data of the healthy Asian population.5 These results suggest that with respect to the non-contact lens wearers, patients
with SAC are more myopic than healthy individuals. Therefore, the myopia may be relevant in SAC. A possible drawback of this study is that myopic patients with allergic conjunctivitis are
less likely to tolerate contact lens wear and the selective analysis of the non-contact lens wearers is likely to include a significant proportion of myopic allergic patients. Therefore,
future study should be designed to overcome this bias induced by contact lens wearer. However, most contact lens wearers were 20–40 years old in the current study; and contrary to
expectation, there was no significant difference in refractive error between patients with and without allergic conjunctivitis in the non-contact lens wearers aged between 20 and 39 years.
Furthermore, as shown Figure 1, each age group except for the group aged 20–39, showed significant differences in refractive error between patients with and without allergic conjunctivitis,
suggesting that allergic conjunctivitis may be associated with refractive error at least in the younger group under 19 years and older group over 40 years. The first possibility is to assume
that the configuration of the corneal surface leads to allergic conjunctivitis. Recent investigations have demonstrated that vernal conjunctivitis, classified under the term allergic
conjunctivitis, is related to the abnormal pattern of the corneal surface.6 The abnormal ocular surface deteriorates the capacity of the fluid reservoir over the ocular surface. Tear film
anomalies capture allergens in the conjunctival SAC and cause the conjunctival immune-based inflammation by inducing T-cell activation. Thus, refractive error may be a possible risk factor
for the direct progression to allergic conjunctivitis. Second, myopic eyes, which have a longer axial eye length and wider palpebral fissures, may be liable to mediate intimate attachment of
allergens by the close interaction between bulbar and palpebral conjunctiva. Third, myopia may be indirectly relevant to SAC. Myopia is associated with education levels and socioeconomic
factors.5 Moreover, educational level appears to be associated with the risk of allergic sensitization,7 and higher socioeconomic status is associated with high multiple allergen
concentrations in house dust.8, 9 High humidity and warm temperature in high-income homes are optimal conditions for mite growth. House dust mites, in particular, multiply in the bed,
bedroom carpets, and upholstered furniture under hot and humid atmospheric conditions. Therefore, myopic people with a high-socioeconomic status may be exposed to a high level of allergens.
Myopic patients may be prone to suffer from allergic conjunctivitis on account of these factors. However, we cannot comment on the role of myopia due to the limitations of our study. The
question of how refraction and allergic conjunctivitis are actually correlated with each other is still open. Additionally, as compared with the Asian population, our findings may not be
applicable to Western populations with a lower prevalence of refractive errors.10 Thus, these considerations invite further empirical investigation concerning the interaction between
refraction and allergic conjunctivitis. REFERENCES * Mimura T, Yamagami S, Amano S, Funatsu H, Arimoto A, Usui T _et al_. Allergens in Japanese patients with allergic conjunctivitis in
autumn. _Eye_ 2005; 19: 995–999. Article CAS Google Scholar * Mimura T, Amano S, Funatsu H, Yamagami S, Araie M, Kaji Y _et al_. Correlations between allergen-specific IgE serum levels in
patients with allergic conjunctivitis in Spring. _Ocul Immunol Inflamm_ 2004; 12: 45–51. Article Google Scholar * Ben Ezra D . Guidelines on the diagnosis and treatment of conjunctivitis.
_Ocul Immunol Inflamm_ 1994; 2(Suppl): 17–26. Google Scholar * Suchecki JK, Donshik P, Ehlers WH . Contact lens complications. _Ophthalmol Clin North Am_ 2003; 16: 471–484. Article Google
Scholar * Shimizu N, Nomura H, Ando F, Niino N, Miyake Y, Shimokata H . Refractive errors and factors associated with myopia in an adult Japanese population. _Jpn J Ophthalmol_ 2003; 47:
6–12. Article Google Scholar * Totan Y, Hepşen IF, Cekiç O, Gündüz A, Aydin E . Incidence of keratoconus in subjects with vernal keratoconjunctivitis: a videokeratographic study.
_Ophthalmology_ 2001; 108: 824–827. Article CAS Google Scholar * Porsbjerg C, Linstow ML, Nepper-Christensen SC, Rasmussen A, Korsgaard J, Nolte H, Greenlandic Population Study Group _et
al_. Allergen sensitization and allergen exposure in Greenlander Inuit residing in Denmark and Greenland. _Respir Med_ 2002; 96: 736–744. Article CAS Google Scholar * Rosenstreich DL,
Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P _et al_. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. _N
Engl J Med_ 1997; 336: 1356–1363. Article CAS Google Scholar * Kitch BT, Chew G, Burge HA, Muilenberg ML, Weiss ST, Platts-Mills TA _et al_. Socioeconomic predictors of high allergen
levels in homes in the greater Boston area. _Environ Health Perspect_ 2000; 108: 301–307. Article CAS Google Scholar * Saw SM, Katz J, Schein OD, Chew SJ, Chan TK . Epidemiology of
myopia. _Epidemiol Rev_ 1996; 18: 175–187. Article CAS Google Scholar Download references ACKNOWLEDGEMENTS The authors have no commercial or proprietary interest in the product or company
described in the current article. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Ophthalmology, University of Tokyo Graduate School of Medicine, Tokyo, Japan T Mimura, Y
Mimura, A Arimoto, S Amano, S Yamagami, T Usui & N Honda * Okamoto Eye Clinic, Yamato, Japan T Mimura, A Arimoto & S Okamoto * Department of Ophthalmology, Yachiyo Medical Center,
Tokyo Women's Medical University, Chiba, Japan H Funatsu & H Noma Authors * T Mimura View author publications You can also search for this author inPubMed Google Scholar * Y Mimura
View author publications You can also search for this author inPubMed Google Scholar * A Arimoto View author publications You can also search for this author inPubMed Google Scholar * S
Amano View author publications You can also search for this author inPubMed Google Scholar * S Yamagami View author publications You can also search for this author inPubMed Google Scholar *
H Funatsu View author publications You can also search for this author inPubMed Google Scholar * T Usui View author publications You can also search for this author inPubMed Google Scholar
* H Noma View author publications You can also search for this author inPubMed Google Scholar * N Honda View author publications You can also search for this author inPubMed Google Scholar *
S Okamoto View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to T Mimura. RIGHTS AND PERMISSIONS Reprints and
permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Mimura, T., Mimura, Y., Arimoto, A. _et al._ Relationship between refraction and allergic conjunctivitis. _Eye_ 23, 63–66 (2009).
https://doi.org/10.1038/sj.eye.6702999 Download citation * Received: 11 June 2007 * Accepted: 10 September 2007 * Published: 12 October 2007 * Issue Date: January 2009 * DOI:
https://doi.org/10.1038/sj.eye.6702999 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * allergic conjunctivitis * refraction * myopia
