Functional mitral regurgitation and left ventricular systolic dysfunction in the recent era of cardiovascular clinical practice, an observational cohort study
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT Functional mitral regurgitation (MR) is frequently associated with left ventricular systolic dysfunction (LVSD). Ventricular volume overload that occurs in patients with MR may lead
to a progression of myocardial dysfunction. However, the prevalence and clinical outcomes of functional MR in Japanese patients with LVSD remain unclear. The aim of the present study is to
clarify the prevalence and prognosis of functional MR in Japanese LVSD patients in the contemporary era. We followed patients with LVSD (LV ejection fraction (LVEF) ⩽40%) who were listed
within a single, hospital-based cohort in the Shinken Database from 2004 to 2011, which was composed of all new patients (_n_=17 517) who visited the Cardiovascular Institute. A total of 506
patients were included: 86 FMR (moderate-to-severe functional MR) patients and 420 non-FMR (none or mild functional MR) patients. FMR patients were older, had lower rates of hypertension
and ischemic heart disease but had higher rates of chronic kidney disease, dilated cardiomyopathy and New York Heart Association III/IV classification. FMR patients had higher brain
natriuretic peptide levels and lower LVEF. The Kaplan–Meier curves revealed that the incidence of all-cause death, cardiovascular death and heart failure (HF) admission was significantly
higher in FMR patients. The presence of FMR was independently associated with a significantly higher risk of composite end point, including all-cause death and/or HF admission (hazard ratio
1.551, 95% confidence interval 1.045–2.303, _P_=0.029). FMR was common in Japanese patients with LVSD and was associated with adverse long-term outcomes. Future study is warranted to
establish the optimal therapeutic strategy for FMR and LVSD. SIMILAR CONTENT BEING VIEWED BY OTHERS PROGNOSIS AND DIASTOLIC DYSFUNCTION PREDICTORS IN PATIENTS WITH HEART FAILURE AND
RECOVERED EJECTION FRACTION Article Open access 24 May 2022 PREDICTORS OF OUTCOMES IN PATIENTS WITH MITRAL REGURGITATION UNDERGOING PERCUTANEOUS VALVE REPAIR Article Open access 13 October
2020 LEFT ATRIAL SIZE PREDICTS OUTCOME IN SEVERE BUT ASYMPTOMATIC MITRAL REGURGITATION Article Open access 08 March 2023 INTRODUCTION Patients with left ventricular (LV) dysfunction often
have mitral regurgitation (MR). The mechanism of MR includes apical and posterior displacement of the papillary muscles, which results in abnormal coaptation of the mitral leaflets. Annular
dilation may also contribute to the creation of MR.1 This condition is termed as functional MR and is frequently observed in patients with LV systolic dysfunction (LVSD).2, 3 Chronic MR
leads to further depression in LV contractility4 and may result in adverse outcomes through a progressive spiral of LV remodeling.5 Previous studies conducted in Western countries have shown
that the presence of MR in patients with LVSD was associated with poor prognosis.3, 5, 6 In contrast, the epidemiology of cardiovascular disease in Japan is different from that of Western
countries with respect to ethnic background and etiology. Moreover, previous reports regarding functional MR and LVSD were based on clinical practices in the 1980s to 1990s.7, 8
Sophisticated patient care and cutting edge therapeutic strategies have prolonged the lifespan of patients with heart failure (HF), and the management of severe HF patients, such as with
advanced LV remodeling, has become more important recently. Therefore, functional MR has attracted more attention in the contemporary era of HF management. However, little is known about the
current prevalence and prognosis of functional MR in Japanese patients with LVSD in real-world clinical settings. Thus we examined a hospital-based cohort from the Shinken Database using
data obtained between 2004 and 2011.9, 10, 11 In the present study, we aimed to clarify the current prevalence and long-term clinical outcomes of FMR in Japanese LVSD patients by using a
hospital-based cohort. METHODS STUDY POPULATION AND PROTOCOL The Shinken Database is composed of all new patients at the Cardiovascular Institute in Tokyo, Japan (‘Shinken’ is an abbreviated
name in Japanese for the name of the hospital), excluding patients with active cancer and any foreign travelers.9, 10, 11 The principal aim of this hospital-based database is to survey the
prevalence and prognosis of cardiovascular diseases in urban areas of Japan.12 The registry started in June 2004, and thereafter, patients have been continually registered to the database
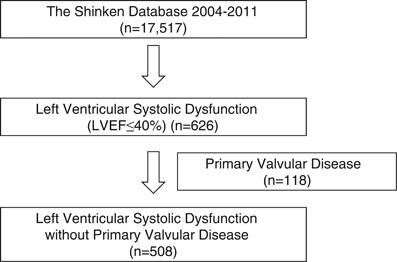
annually. The data in the present study were derived from this database between June 2004 and March 2012 (Shinken Database 2004–2011), including 17 517 new visiting patients. Of these
patients, 626 patients were found to have LVSD (LV ejection fraction (LVEF) ⩽40%). We excluded patients with primary valvular heart disease (_n_=118). Valvular heart disease was defined as
long-standing mitral or aortic valve involvement, as documented by physical examination, echocardiography and angiography. Finally, 508 patients were examined and tracked for an average of
978±789 days in this study (Figure 1). ETHICS The ethics committee at the Cardiovascular Institute granted permission for this study, and all of the patients gave written informed consent.
The study was performed in accordance with the Declaration of Helsinki. DATA COLLECTION After obtaining the electrocardiogram and chest X-ray readings, cardiovascular status was evaluated in
each patient using echocardiography, an exercise test and blood laboratory data according to the attending physician’s decision within 3 months after the first visit. All echocardiographic
studies were performed as part of routine clinical care. MR, as assessed by color Doppler echocardiography, was performed at the first hospital visit (HP Sonos 5500, Philips Medical Systems,
Andover, MA, USA; SSD 6500, Aloka, Mitaka, Tokyo, Japan; iE33, Phillips Medical Systems, Andover, MA, USA; Pro Sound α10, Aloka, Mitaka, Tokyo, Japan; Vivid E9 GE Healthcare Japan, Hino,
Tokyo, Japan; Artida, Toshiba Medical Systems, Otawara, Tochigi, Japan). Functional MR was diagnosed based on the findings of normal leaflet structures with a maximum systolic position of
one or both mitral leaflets above the mitral annulus level. The severity of the MR (none, mild, moderate and severe) was determined by more than two experienced echocardiographers without
the knowledge of the patients’ background and was based on the quantitative assessment by visually comparing the turbulent flow jet area with the left atrial area.13 Patients were divided
into two groups according to the baseline MR grade: 86 FMR (moderate-to-severe functional MR) patients and 420 non-FMR (none or mild FMR) patients. The following were collected as the
initial clinical parameters: sex, age, drug information, and coexisting conditions. The following echocardiographic parameters were also collected: LV end-diastolic dimension, LV
end-systolic dimension, interventricular septum thickness, posterior wall thickness, and LVEF. The estimated glomerular filtration rate was calculated using the glomerular filtration rate
equation for the Japanese population: glomerular filtration rate=194 × (serum creatinine)1.094 × (age)0.287 × (0.739 if female).14 Chronic kidney disease was defined as an estimated
glomerular filtration rate <60 ml min−1 1.73 m−2.14, 15 Idiopathic dilated cardiomyopathy was diagnosed by the presence of global LV dilatation with impaired systolic function occurring
in the absence of known cardiac causes. Hypertrophic cardiomyopathy was diagnosed by echocardiography when hypertrophy (interventricular septum thickness or posterior wall thickness >12
mm) without hypertension was present. We confirmed the deaths of study patients from the medical records of our hospital or from the obtained follow-up information. Surgical mitral valve
intervention included surgical mitral valve repair or placement. PATIENT FOLLOW-UP The health status of patients, incidence of cardiovascular events and mortality are maintained in the
database through a link to the hospital medical records. Study documents on prognosis were sent once per year to patients who have discontinued hospital visits or have been referred to other
hospitals. In the present data analysis, follow-up data after 1 April 2012 were excluded. Therefore, the end of the follow-up period was defined as one of the following three time points:
(1) date of death if before 31 March 2012; (2) final hospital visit or the date of the final response to our study documents of prognosis with the confirmation of being alive before 31 March
2012; or (3) 31 March 2012, date of death, final hospital visit, or if the final response to our study questions on prognosis were later than 1 April 2012. We confirmed the HF events (HF
requiring hospitalization or death due to HF), which were classified according to the International Classification of Diseases (tenth revision, code I50) using the medical records of our
hospital or from the information obtained during follow-up. Cardiovascular death included death resulting from acute myocardial infarction, sudden cardiac death, death due to HF, death due
to stroke and death due to other cardiovascular causes.16 STATISTICAL ANALYSIS The categorical and consecutive data of the patients’ background characteristics are presented as number (%)
and mean±s.d., respectively. The _χ_2 test was used for group comparisons, and the unpaired _t_-test was used to compare the consecutive variables. Long-term event-free survival was
estimated using the Kaplan–Meier curves, and the log-rank test was used to assess the significance of differences between the two groups. Cox regression analyses were performed to identify
the effects of FMR on the long-term clinical outcomes. In the adjusted Cox regression model, univariate Cox regression analysis was adjusted for the following covariates (step-wise method):
age ⩾65 years, hypertension, chronic kidney disease, brain natriuretic peptide (BNP) ⩾100 pg ml−1, ischemic heart disease (IHD), idiopathic dilated cardiomyopathy, New York Heart Association
(NYHA) class ⩾II, and renin–angiotensin system inhibitor (RAS-I), diuretics and digitalis use. As a sub-analysis, we compared the characteristics and long-term outcomes of FMR patients with
and without surgical MR intervention. A probability value of <0.05 indicated statistical significance. These analyses were performed using the SPSS version 19.0 software (SPSS, Chicago,
IL, USA). RESULTS Among the 17 517 patients who visited our hospital, a total of 506 patients with LVSD were enrolled in this study. FMR patients were observed in 86 patients (17.0%),
whereas 420 were non-FMR patients. FMR patients had lower rates of hypertension, dyslipidemia and ischemic heart disease and higher rates of idiopathic dilated cardiomyopathy. The average
BNP level in FMR patients was higher than those in non-FMR patients. FMR patients had a lower prevalence of NYHA II classification but a higher prevalence of NYHA III and IV than non-FMR
patients (Table 1). Echocardiography showed that LV end-diastolic dimension and LV end-systolic dimension were greater in FMR patients than in non-FMR patients. LVEF was lower in FMR
patients (Table 2). The use of RAS-Is, diuretics and digitalis was more common in FMR patients _vs._ non-FMR patients. Beta-blocker use was comparable between the two groups (Table 3).
Overall, all-cause death (cardiovascular death) occurred in 11.0% (5.5%) of non-FMR patients, compared with 23.3% (17.4%) in FMR patients. HF admission occurred in 37.2% of FMR patients and
in 16.9% of non-FMR patients (Table 4). Kaplan–Meier curves revealed that the rates of all-cause death, cardiovascular death and HF admission were significantly higher in FMR patients _vs._
non-FMR patients (Figure 2). Similarly, the Cox regression analysis with unadjusted models showed that FMR was associated with a significantly higher risk for all-cause death (hazard ratio
(HR) 2.076, 95% confidence interval (95% CI) 1.228–3.511, _P_=0.006), cardiovascular death (HR 3.123, 95% CI 1.629–5.988, _P_=0.001) and HF admission (HR 2.533, 95% CI 1.688–3.847,
_P_<0.001). The adjusted Cox regression analysis showed that in addition to chronic kidney disease, BNP ⩾100 pg ml−1 and ischemic heart disease, the presence of FMR was still associated
with a significantly higher risk for composite end point, including all-cause death and/or HF admission (HR 1.551, 95% CI 1.045–2.303, _P_=0.029) (Table 5). In a sub-analysis, we compared
the background characteristics of FMR patients between patients with and without surgical MR intervention. Among FMR patients (_n_=86), 36 (42%) had undergone surgical MR intervention.
Patients who had undergone surgery tended to be younger than those who had not undergone surgery. The prevalence of hypertension was lower in patients who had undergone surgical MR
intervention than in those who had not undergone surgical MR intervention. The average BNP level and NYHA class was comparable between the two groups. The etiology of LVSD was not different
between the two groups (Supplementary Table S1). Echocardiography showed that LV wall thickness was thinner and LV dimension was greater in patients who had undergone surgical MR
intervention than in those who had not undergone surgical MR intervention (Supplementary Table S2). Calcium channel blockers tended to be commonly used in patients who had undergone MR
surgery than in those who had not undergone surgical MR intervention (Supplementary Table S3). The Kaplan–Meier curve showed FMR patient mortality for patient who had and had not undergone
surgical MR intervention (Log-rank _P_=0.190; Figure 3). Similar to the Kaplan–Meier curve in Figure 3, the univariate Cox regression analysis showed that surgical MR intervention was not
associated with long-term mortality (HR 1.790, 95% CI 0.740–4.329, _P_=0.197). We adjusted the univariate Cox regression analysis with the following covariates: age ⩾65 years, hypertension,
LV end-diastolic dimension, and calcium channel blocker use. After these adjustments, surgical MR intervention was not associated with long-term mortality (HR 2.188, 95% CI 0.781–6.128,
_P_=0.136). DISCUSSION The present study was performed in an observational cohort of patients with LVSD, and the results of this study demonstrated the prevalence and clinical outcomes of
Japanese FMR patients in a recent, real-world, clinical setting. The major findings of the present study were as follows: (1) FMR was complicated in 17.0% of LVSD patients who visited a
cardiovascular hospital in Japan, (2) FMR patients had worse background clinical characteristics, such as lower LVEF, higher BNP and higher rates of NYHA III/VI, and (3) the presence of FMR
was still associated with higher incidences of all-cause death, cardiovascular death and HF admission in recent, real-world clinical practice in Japan. Functional MR is a common condition in
patients with LVSD, and its prevalence varies according to the severity of HF and the background characteristics of the study patients. Regarding the etiology of LVSD, the prevalence of IHD
is different between the Japanese population and patients previously studied in Western countries. Trichon _et al._8 reported that the prevalence of IHD in patients with functional MR and
LVSD was approximately 60%, whereas this was only 39% in the present study. As previous studies have revealed, the presence of IHD was strongly associated with worse clinical outcomes in HF
patients. Furthermore, in the present study, the presence of IHD is associated with higher incidences of all-cause death and/or HF admission. Therefore, the different prevalence of IHD might
affect the differences in clinical outcomes between the Western and Japanese populations. Furthermore, previous studies focusing on functional MR and LVSD were based on clinical practices
in the 1980s to 1990s.7, 8 Our hospital database started in 2004, and the treatment strategy for LVSD gradually changed from the 1980s to 2000s. In addition, we should pay attention to the
ethnic differences in cardiovascular disease. However, to our knowledge, there is limited data focusing on the presentation and long-term clinical outcomes of patients with functional MR and
LVSD in clinical practices in Japan. In the present study, FMR was observed in 17.0% of Japanese patients with LVSD. Along with the previous studies performed in Western countries,7 FMR
patients had worse background clinical characteristics, such as higher BNP levels and more severe HF symptom, compared with those of non-FMR patients (Table 1). The presence of FMR was
associated with higher incidences of all-cause death, cardiovascular death and HF admission. Even after covariate adjustments, the presence of FMR was still associated with worse long-term
outcomes in patients with LVSD. The optimal medical treatment for patients with FMR and LVSD is not established. Some anti-hypertensive and cardio-protective drugs, such as beta-blockers and
RAS-Is, might have potential. Varadarajan _et al._17 reported that the use of beta-blockers was associated with improved survival in patients with severe MR. However, this study included
patients with normal LV function. The beneficial effects of beta-blockers for patients with FMR and LVSD need to be clarified. However, RAS-Is also have potential. The administration of
ramipril was reported to reduce MR severity in patients with baseline systolic blood pressure ⩾140 mm Hg but not in patients with systolic blood pressure <140 mm Hg.18 Beta-blockers and
RAS-Is are not only anti-hypertensive drugs but also cardio-protective drugs, and these drugs are strongly recommended for patients with LVSD. The clinical impact of beta-blockers and RAS-Is
on FMR patients with LVSD through various pharmacological effects, such as blood pressure lowering and protection against further LV remodeling, needs to be clarified. In the present study,
the prevalence of hypertension was lower in patients with FMR than those without, and beta-blockers and RAS-Is were administered in 58.1% and 77.9% of patients with FMR and LVSD,
respectively. However, we might need to use these potential medications more aggressively to aim for an optimal blood pressure control and cardiac protection for these patients. Patients
with functional MR and advanced HF pose a particularly difficult management dilemma, because the surgical risk of this population is extremely high and the benefits of surgical MR reduction
have been variable, inconsistent and suboptimal.19, 20 Along with the previous studies, we could not find any significant differences between patients with and without surgical MR
intervention. As shown in the sub-analysis, the background characteristics of study patients were different between the two groups. However, even after adjustments with covariates, there
were no significant differences in the long-term survival between these two groups. Early intervention for patients with FMR and LVSD with MR surgery might be a potential option. The optimal
surgical candidate and timing of functional MR is still currently unclear. Cardiac resynchronization therapy also has a potential for the treatment of FMR patients.21 Focusing on the
functional MR patients with high operative risk, the therapeutic potential of cardiac resynchronization therapy for moderate to severe functional MR was examined. MR reduction was observed
in all patients who survived over 6 months after cardiac resynchronization therapy, and patients with improved MR had better outcomes than those with non-improvers.22 Percutaneous
edge-to-edge mitral valve repair has emerged as a novel therapeutic option for the treatment among them, of severe MR.23, 24, 25, 26 Auricchio _et al._27 examined 51 severely symptomatic
(NYHA ⩾III) cardiac resynchronization therapy nonresponders with significant FMR underwent percutaneous edge-to-edge mitral valve repair and reported that treatment with percutaneous
edge-to-edge mitral valve repair was feasible, safe and demonstrated improved HF symptom, increased LVEF and induced reverse LV remodeling in approximately 70% of the study population. In
cases of surgical MR intervention, we should pay attention to aggravated LV function after surgery. Therefore, if we can expect reverse LV remodeling (improved LV function) by percutaneous
procedure, percutaneous intervention for FMR might be an attractive option for patients with functional MR and LVSD. The present study has several clinical implications. Functional MR was
frequently associated with advanced LVSD. Therefore, the poor prognosis of patients with functional MR might reflect the adverse outcomes of severe LVSD. However, the presence of functional
MR further worsens LV remodeling. Moreover, the recent studies suggested that treating functional MR with percutaneous mitral valve repair improved LV function and resulted in reverse
remodeling.27, 28 Thus, paradoxically, it is possible that functional MR has the potential to be a treatable target of advanced LV remodeling. We recognize several limitations in this study.
The sample size of the present study was limited, thus the statistical power might not be sufficient for any negative data to be conclusive. The etiology of LVSD was not determined in 10%
of the study populations and may affect the results. We used a semi-quantitative grading of MR in this study. Although the regurgitant jet of functional MR is usually central and correlated
well with the regurgitant volume,29 the quantitative grading of MR might be performed in a further study. Moreover, because of the nature of a single hospital-based cohort, we could not
conclude the effect of surgical MR intervention on functional MR and LVSD with only this study. Further studies, especially randomized studies, are needed to clarify the optimal candidate
for MR surgery in patients with functional MR and LVSD in the future. In conclusion, this observational study of a cohort of unselected, Japanese, LVSD patients revealed that FMR was a
common condition in LVSD patients. FMR is still currently associated with long-term mortality and HF admission in the cardiovascular clinical practice. Further study is warranted to
establish optimal therapeutic strategies for FMR and LVSD. REFERENCES * Harris PJ, Harrell FE Jr, Lee KL, Behar VS, Rosati RA . Survival in medically treated coronary artery disease.
_Circulation_ 1979; 60: 1259–1269. Article CAS Google Scholar * Bart BA, Shaw LK, McCants CB Jr, Fortin DF, Lee KL, Califf RM, O'Connor CM . Clinical determinants of mortality in
patients with angiographically diagnosed ischemic or nonischemic cardiomyopathy. _J Am Coll Cardiol_ 1997; 30: 1002–1008. Article CAS Google Scholar * Smith LR, Harrell FE Jr, Rankin JS,
Califf RM, Pryor DB, Muhlbaier LH, Lee KL, Mark DB, Jones RH, Oldham HN _et al_. Determinants of early versus late cardiac death in patients undergoing coronary artery bypass graft surgery.
_Circulation_ 1991; 84: III245–III253. CAS PubMed Google Scholar * Sheehan FH, Bolson EL, Dodge HT, Mathey DG, Schofer J, Woo HW . Advantages and applications of the centerline method for
characterizing regional ventricular function. _Circulation_ 1986; 74: 293–305. Article CAS Google Scholar * Felker GM, Shaw LK, O'Connor CM . A standardized definition of ischemic
cardiomyopathy for use in clinical research. _J Am Coll Cardiol_ 2002; 39: 210–218. Article Google Scholar * Strauss RH, Stevenson LW, Dadourian BA, Child JS . Predictability of mitral
regurgitation detected by Doppler echocardiography in patients referred for cardiac transplantation. _Am J Cardiol_ 1987; 59: 892–894. Article CAS Google Scholar * Koelling TM, Aaronson
KD, Cody RJ, Bach DS, Armstrong WF . Prognostic significance of mitral regurgitation and tricuspid regurgitation in patients with left ventricular systolic dysfunction. _Am Heart J_ 2002;
144: 524–529. Article Google Scholar * Trichon BH, Felker GM, Shaw LK, Cabell CH, O'Connor CM . Relation of frequency and severity of mitral regurgitation to survival among patients
with left ventricular systolic dysfunction and heart failure. _Am J Cardiol_ 2003; 91: 538–543. Article Google Scholar * Kaneko H, Koike A, Senoo K, Tanaka S, Suzuki S, Nagayama O, Sagara
K, Otsuka T, Matsuno S, Funada R, Uejima T, Oikawa Y, Yajima J, Nagashima K, Kirigaya H, Sawada H, Aizawa T, Yamashita T . Role of cardiopulmonary dysfunction and left atrial remodeling in
development of acute decompensated heart failure in chronic heart failure with preserved left ventricular ejection fraction. _J Cardiol_ 2012; 59: 359–365. Article Google Scholar * Kaneko
H, Yajima J, Oikawa Y, Tanaka S, Fukamachi D, Suzuki S, Sagara K, Otsuka T, Matsuno S, Funada R, Kano H, Uejima T, Koike A, Nagashima K, Kirigaya H, Sawada H, Aizawa T, Yamashita T . Obesity
paradox in Japanese patients after percutaneous coronary intervention: an observation cohort study. _J Cardiol_ 2013; 62: 18–24. Article Google Scholar * Kaneko H, Suzuki S, Yajima J,
Oikawa Y, Sagara K, Otsuka T, Matsuno S, Kano H, Uejima T, Koike A, Nagashima K, Kirigaya H, Sawada H, Aizawa T, Yamashita T . Clinical characteristics and long-term clinical outcomes of
Japanese heart failure patients with preserved versus reduced left ventricular ejection fraction: a prospective cohort of Shinken Database 2004–2011. _J Cardiol_ 2013; 62: 102–109. Article
Google Scholar * Suzuki S, Yamashita T, Ohtsuka T, Sagara K, Uejima T, Oikawa Y, Yajima J, Koike A, Nagashima K, Kirigaya H, Ogasawara K, Sawada H, Aizawa T . Prevalence and prognosis of
patients with atrial fibrillation in Japan: a prospective cohort of Shinken Database 2004. _Circ J_ 2008; 72: 914–920. Article Google Scholar * Van Dantzig JM, Delemarre BJ, Koster RW, Bot
H, Visser CA . Pathogenesis of mitral regurgitation in acute myocardial infarction: importance of changes in left ventricular shape and regional function. _Am Heart J_ 1996; 131: 865–871.
Article CAS Google Scholar * Kaneko H, Yajima J, Oikawa Y, Tanaka S, Fukamachi D, Suzuki S, Sagara K, Otsuka T, Matsuno S, Funada R, Kano H, Uejima T, Koike A, Nagashima K, Kirigaya H,
Sawada H, Aizawa T, Yamashita T . Effects of statin treatment in patients with coronary artery disease and chronic kidney disease. _Heart Vessels_ 2014; 29: 21–28. Article Google Scholar *
Tonelli M, Jose P, Curhan G, Sacks F, Braunwald E, Pfeffer M . Proteinuria, impaired kidney function, and adverse outcomes in people with coronary disease: analysis of a previously
conducted randomised trial. _BMJ_ 2006; 332: 1426. Article Google Scholar * Kaneko H, Yajima J, Oikawa Y, Tanaka S, Fukamachi D, Suzuki S, Sagara K, Otsuka T, Matsuno S, Funada R, Kano H,
Uejima T, Koike A, Nagashima K, Kirigaya H, Sawada H, Aizawa T, Yamashita T . Impact of aging on the clinical outcomes of Japanese patients with coronary artery disease after percutaneous
coronary intervention. _Heart Vessels_ 2014; 29: 156–164. Article Google Scholar * Varadarajan P, Joshi N, Appel D, Duvvuri L, Pai RG . Effect of Beta-blocker therapy on survival in
patients with severe mitral regurgitation and normal left ventricular ejection fraction. _J Am Coll Cardiol_ 2008; 102: 611–615. Article CAS Google Scholar * Harris KM, Aeppli DM, Carey
CF . Effects of angiotensin-converting enzyme inhibition on mitral regurgitation severity, left ventricular size, and functional capacity. _Am Heart J_ 2005; 150: 1106. Article Google
Scholar * Mihaljevic T, Lam BK, Rajeswaran J, Takagaki M, Lauer MS, Gillinov AM, Blackstone EH, Lytle BW . Impact of mitral valve annuloplasty combined with revascularization in patients
with functional ischemic mitral regurgitation. _J Am Coll Cardiol_ 2007; 49: 2191–2201. Article Google Scholar * Wu AH, Aaronson KD, Bolling SF, Pagani FD, Welch K, Koelling TM . Impact of
mitral valve annuloplasty on mortality risk in patients with mitral regurgitation and left ventricular systolic dysfunction. _J Am Coll Cardiol_ 2005; 45: 381–387. Article Google Scholar
* Breithardt OA, Sinha AM, Schwammenthal E, Bidaoui N, Markus KU, Franke A, Stellbrink C . Acute effects of cardiac resynchronization therapy on functional mitral regurgitation in advanced
systolic heart failure. _J Am Coll Cardiol_ 2003; 41: 765–770. Article Google Scholar * van Bommel RJ, Marsan NA, Delgado V, Borleffs CJ, van Rijnsoever EP, Schalij MJ, Bax JJ . Cardiac
resynchronization therapy as a therapeutic option in patients with moderate-severe functional mitral regurgitation and high operative risk. _Circulation_ 2011; 124: 912–919. Article Google
Scholar * Feldman T, Wasserman HS, Herrmann HC, Gray W, Block PC, Whitlow P, St Goar F, Rodriguez L, Silvestry F, Schwartz A, Sanborn TA, Condado JA, Foster E . Percutaneous mitral valve
repair using the edge-to-edge technique: six-month results of the EVEREST Phase I Clinical Trial. _J Am Coll Cardiol_ 2005; 46: 2134–2140. Article Google Scholar * Feldman T, Kar S,
Rinaldi M, Fail P, Hermiller J, Smalling R, Whitlow PL, Gray W, Low R, Herrmann HC, Lim S, Foster E, Glower D . Percutaneous mitral repair with the MitraClip system: safety and midterm
durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. _J Am Coll Cardiol_ 2009; 54: 686–694. Article Google Scholar * Feldman T, Foster E, Glower DD, Kar
S, Rinaldi MJ, Fail PS, Smalling RW, Siegel R, Rose GA, Engeron E, Loghin C, Trento A, Skipper ER, Fudge T, Letsou GV, Massaro JM, Mauri L . Percutaneous repair or surgery for mitral
regurgitation. _N Engl J Med_ 2011; 364: 1395–1406. Article CAS Google Scholar * Neuss M, Schau T, Schoepp M, Seifert M, Holschermann F, Meyhofer J, Butter C . Patient selection criteria
and midterm clinical outcome for MitraClip therapy in patients with severe mitral regurgitation and severe congestive heart failure. _Eur J Heart Fail_ 2013; 15: 786–795. Article Google
Scholar * Auricchio A, Schillinger W, Meyer S, Maisano F, Hoffmann R, Ussia GP, Pedrazzini GB, van der Heyden J, Fratini S, Klersy C, Komtebedde J, Franzen O . Correction of mitral
regurgitation in nonresponders to cardiac resynchronization therapy by MitraClip improves symptoms and promotes reverse remodeling. _J Am Coll Cardiol_ 2011; 58: 2183–2189. Article Google
Scholar * Grayburn PA, Foster E, Sangli C, Weissman NJ, Massaro J, Glower DG, Feldman T, Mauri L . Relationship between the magnitude of reduction in mitral regurgitation severity and left
ventricular and left atrial reverse remodeling after MitraClip therapy. _Circulation_ 2013; 128: 1667–1674. Article Google Scholar * Enriquez-Sarano M, Tajik AJ, Bailey KR, Seward JB .
Color flow imaging compared with quantitative Doppler assessment of severity of mitral regurgitation: influence of eccentricity of jet and mechanism of regurgitation. _J Am Coll Cardiol_
1993; 21: 1211–1219. Article CAS Google Scholar Download references ACKNOWLEDGEMENTS We thank Shiro Ueda and Nobuko Ueda at the Medical Edge for assembling the database using the Clinical
Study Support System (CliSSS) and Ineko Hayakawa, Hiroaki Arai and Hiroshi Aoki for data management and system administration. This work was supported by the Japanese society for the
promotion of science (to HK). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Cardiovascular Medicine, The Cardiovascular Institute, Tokyo, Japan Hidehiro Kaneko, Shinya Suzuki,
Tokuhisa Uejima, Hiroto Kano, Shunsuke Matsuno, Hideaki Takai, Yuji Oikawa, Junji Yajima, Tadanori Aizawa & Takeshi Yamashita Authors * Hidehiro Kaneko View author publications You can
also search for this author inPubMed Google Scholar * Shinya Suzuki View author publications You can also search for this author inPubMed Google Scholar * Tokuhisa Uejima View author
publications You can also search for this author inPubMed Google Scholar * Hiroto Kano View author publications You can also search for this author inPubMed Google Scholar * Shunsuke Matsuno
View author publications You can also search for this author inPubMed Google Scholar * Hideaki Takai View author publications You can also search for this author inPubMed Google Scholar *
Yuji Oikawa View author publications You can also search for this author inPubMed Google Scholar * Junji Yajima View author publications You can also search for this author inPubMed Google
Scholar * Tadanori Aizawa View author publications You can also search for this author inPubMed Google Scholar * Takeshi Yamashita View author publications You can also search for this
author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to Hidehiro Kaneko. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no conflict of interest. ADDITIONAL
INFORMATION Supplementary Information accompanies the paper on Hypertension Research website SUPPLEMENTARY INFORMATION SUPPLEMENTARY TABLE S1 (DOC 44 KB) SUPPLEMENTARY TABLE S2 (DOC 36 KB)
SUPPLEMENTARY TABLE S3 (DOC 36 KB) RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Kaneko, H., Suzuki, S., Uejima, T. _et al._ Functional mitral
regurgitation and left ventricular systolic dysfunction in the recent era of cardiovascular clinical practice, an observational cohort study. _Hypertens Res_ 37, 1082–1087 (2014).
https://doi.org/10.1038/hr.2014.122 Download citation * Received: 29 January 2014 * Revised: 29 May 2014 * Accepted: 06 June 2014 * Published: 28 August 2014 * Issue Date: December 2014 *
DOI: https://doi.org/10.1038/hr.2014.122 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * functional mitral regurgitation * left ventricular
dysfunction * prognosis
