A randomized exploratory trial of an alpha-7 nicotinic receptor agonist (tc-5619) for cognitive enhancement in schizophrenia
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT This exploratory trial was conducted to test the effects of an alpha7 nicotinic receptor partial agonist, TC-5619, on cognitive dysfunction and negative symptoms in subjects with
schizophrenia. In the United States and India, 185 outpatients (18–60 years; male 69%; 46% tobacco users) with schizophrenia treated with quetiapine or risperidone monotherapy were
randomized to 12 weeks of placebo (_n_=91) or TC-5619 (_n_=94; orally once daily 1 mg day 1 to week 4, 5 mg week 4 to 8, and 25 mg week 8 to 12). The primary efficacy outcome measure was the
Groton Maze Learning Task (GMLT; executive function) of the CogState Schizophrenia Battery (CSB). Secondary outcome measures included: CSB composite score; Scale for Assessment of Negative
Symptoms (SANS); Clinical Global Impression-Global Improvement (CGI-I); CGI-severity (CGI-S); and Subject Global Impression-Cognition. GMLT statistically favored TC-5619 (_P_=0.036) in this
exploratory trial. SANS also statistically favored TC-5619 (_P_=0.030). No other secondary outcome measure demonstrated a drug effect in the total population; there was a statistically
significant drug effect on working memory in tobacco users. The results were typically stronger in favor of TC-5619 in tobacco users and occasionally better in the United States than in
India. TC-5619 was generally well tolerated with no clinically noteworthy safety findings. These results support the potential benefits of TC-5619 and alpha7 nicotinic receptor partial
agonists for cognitive dysfunction and negative symptoms in schizophrenia. SIMILAR CONTENT BEING VIEWED BY OTHERS PHASE 1 RANDOMIZED STUDY ON THE SAFETY, TOLERABILITY, AND PHARMACODYNAMIC
COGNITIVE AND ELECTROPHYSIOLOGICAL EFFECTS OF A DOPAMINE D1 RECEPTOR POSITIVE ALLOSTERIC MODULATOR IN PATIENTS WITH SCHIZOPHRENIA Article Open access 17 November 2020 LOW-DOSE LITHIUM
ADJUNCT TO ATYPICAL ANTIPSYCHOTIC TREATMENT NEARLY IMPROVED COGNITIVE IMPAIRMENT, DETERIORATED THE GRAY-MATTER VOLUME, AND DECREASED THE INTERLEUKIN-6 LEVEL IN DRUG-NAIVE PATIENTS WITH FIRST
SCHIZOPHRENIA SYMPTOMS: A FOLLOW-UP PILOT STUDY Article Open access 14 October 2023 EFFECTS OF RISPERIDONE/PALIPERIDONE VERSUS PLACEBO ON COGNITIVE FUNCTIONING OVER THE FIRST 6 MONTHS OF
TREATMENT FOR PSYCHOTIC DISORDER: SECONDARY ANALYSIS OF A TRIPLE-BLIND RANDOMISED CLINICAL TRIAL Article Open access 10 June 2023 INTRODUCTION Schizophrenia is a heterogeneous mental
disorder associated with different pathological features, including positive and negative symptoms (DSM IV-TR; American Psychiatric Association, 2000)) and cognitive dysfunction (Reichenberg
and Harvey, 2007). The negative and cognitive symptoms may precede onset of positive symptoms by many years and persist despite the remission of psychosis (Addington and Addington, 1993;
Fleischhacker, 2000; O’Carroll, 2000; Ojeda, 2000; Reichenberg et al, 2010; Tandon et al, 2009). Positive symptoms are highly responsive to antipsychotic medications in the majority of
patients, but negative symptoms and cognitive dysfunction are much less effectively treated (Erhart et al, 2006; Gold, 2004; Marder and Fenton, 2004; Miyamoto et al, 2005; Stahl and Buckley,
2007) and hence may prevent many patients from functioning productively and independently (Gold, 2004; Stahl et al, 2007). In contrast to psychotic symptoms in which the D2 receptor is a
proven target, the pharmacology of cognitive and negative symptoms is not well defined. To this end, the National Institute of Mental Health sponsored the Measurement and Treatment Research
to Improve Cognition in Schizophrenia (MATRICS) initiative to develop a consensus battery of neuropsychological tests that could measure therapeutic effects of agents for cognitive
dysfunction in schizophrenia (CDS; Gold, 2004; Kern et al, 2008; Nuechterlein et al, 2004; Nuechterlein et al, 2008). In the wake of the MATRICS initiative, molecular targets for the
treatment of CDS have been proposed (Gray and Roth, 2007; Marder et al, 2004). Among the prioritized targets was the alpha7 neuronal nicotinic receptor (NNR; Freedman et al, 2008; Kucinski
et al, 2011; Olincy and Stevens, 2007). Initially, preclinical studies indicated that antagonists of this receptor could induce sensory gating deficits in rodents that were similar to those
observed in schizophrenia (Luntz-Leybman et al, 1992). Shortly thereafter, genetic linkage was found for this deficit and the alpha7 NNR gene (Freedman et al, 1997). Post-mortem studies of
individuals with schizophrenia further supported these findings by showing reduced expression of this receptor in the hippocampus (Freedman et al, 1995) and thalamic reticular nucleus (Court
et al, 1999). Several alpha7 NNR agonists have shown promising results in preliminary trials by demonstrating efficacy against surrogate electrophysiological markers
(EnVivo_Pharmaceuticals, 2009; Olincy et al, 2006) and cognitive and negative symptoms of schizophrenia (Freedman et al, 2008). TC-5619 (a benzofuran-substituted pyridylmethylquinuclidine)
is a highly selective alpha7 NNR partial agonist with a Ki at the alpha7 NNR of 1 nM. It is 1000–10 000 times less potent at other NNRs and at other receptor subtypes (eg, 5HT3, opioid). Two
phase 1 studies of TC-5619 in healthy male volunteers showed that single doses of TC-5619 were well tolerated up to 406 mg (limited by orthostatic hypotension) and that multiple doses of
204 mg are well tolerated (Targacept, data on file). The half-life (20 h) and time to _C_max (approximately 2 h) were independent of dose. Finally, the Cognitive Drug Research cognitive test
battery revealed a statistically significant improvement in power of attention (_P_<0.05) in subjects taking 6.8 mg TC-5619 (Targacept Study TC-5619-CLP-002 (data on file)). Based on
these clinical data as well as data from a preclinical model suggesting cognitive benefits at a human dose of approximately 3 mg (Hauser et al, 2009) (Targacept, data on file), a dose range
of 1–25 mg was determined to be safe and conservatively chosen to encompass the anticipated efficacious dose range. SUBJECTS AND METHODS SUBJECTS The study was Institutional Review
Board-reviewed, filed with the US Food and Drug Administration (FDA), and registered on www.clinicaltrials.gov (NCT01003379) before study initiation, and conducted according to the
Guidelines of the Declaration of Helsinki (2008). It was conducted by the sponsor (Targacept) at 12 sites in India and 7 sites in the United States. Enrollment began in November 2009 and was
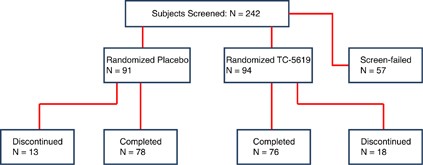
completed in December 2010. A total of 185 subjects were enrolled and randomized (Figure 1; Table 1). Tobacco users were stratified approximately equally across the treatment arms; tobacco
use was verified by urinary cotinine levels >500 ng/ml, and non-use by urinary cotinine levels <50 ng/ml. In all, 46% were tobacco users. In total, 154 subjects completed the study
(Figure 1); the most frequent reason for discontinuation was withdrawal of consent (12 subjects). All subjects met DSM-IV criteria for schizophrenia, primarily paranoid type (92%). Subjects
were required to be outpatients with: stable housing, availability of caregivers with personal contact at least four times weekly, and stable schizophrenia, defined as a lack of psychiatric
hospitalization and no change in quetiapine or risperidone monotherapy dose for 2 months before screening and during the study. Quetiapine and risperidone were chosen for this preliminary
adjunctive treatment study because they are prototypical atypical antipsychotics that are widely used in the clinic. Use of a wider range of underlying antipsychotic treatments will be
adopted in future studies. Subjects could have: a score no >4 on the Positive and Negative Syndrome Scale (PANSS) items assessing delusions, hallucinations, unusual thought content, and
conceptual disorganization; a score no >5 on the Calgary Depression Scale for Schizophrenia (CDSS); and no significant suicidality as assessed by the Columbia Suicide Severity Rating
Scale (CSSRS). Subjects could have no other comorbid axis 1 or axis 2 DSM-IV disorder nor any unstable medical condition. All subjects signed a written informed consent. EXPERIMENTAL DRUG
AND MATCHING PLACEBO The experimental drug was a blend of TC-5619 and excipients in gelatin capsules. Placebo was manufactured to match the experimental drug TC-5619 in identical-appearing
capsules in size, color, and shape. EXPERIMENTAL DRUG PROTOCOL AND ASSESSMENTS At screening, all subjects were trained to use the CogState Schizophrenia Battery (CSB). They also had
assessments using the PANSS, Scale For Assessment of Negative Symptom (SANS), Subject Global Impression-Cognition (SGI-Cog; a subject-rated seven-point Likert scale assessing three items:
memory and learning, attention and concentration, and speed of thinking), and Clinical Global Impression-Severity (CGI-S) scales. Physical examination, vital signs, serum chemistry and
hematology, urinalysis, urine drug screen for illicit drugs, and ECG were performed. Assessments were also made using the Abnormal Involuntary Movements Scale (AIMS), the CSSRS, and the
CDSS. On day 1, all subjects meeting eligibility criteria including absence of illicit drugs were randomized in a double-blind manner (subjects, caregivers, staff, sponsor were blinded)
using a 1 : 1 allocation to receive either TC-5619 or placebo orally once daily, in addition to quetiapine or risperidone monotherapy. The random allocation method was based on a blinded
sequence method applied by an independent statistician employed by an outside vendor. Approximately equal numbers of tobacco users and non-users were stratified and randomized to each
cohort. Blood samples were taken before and approximately 3 h after study drug was administered in the clinic, and these were processed for PK analyses of TC-5619 and for measuring blood
levels of quetiapine and risperidone. ECG and vital signs measurements were obtained just before each PK blood sample. Subjects in the TC-5619 cohort were to take 1 mg TC-5619 qd from day 1
to week 4; 5 mg qd from week 4 to 8; and 25 mg qd from week 8 to 12. Subjects were instructed to take their daily dose of study drug each morning, at least 90 min before tobacco use (if a
user) and at least 30 min before taking quetiapine or risperidone. Subjects returned for clinic visits at weeks 1, 4, 8, and 12 for safety and efficacy assessments. Subject compliance for
TC-5619 was monitored by pill counts at each visit. Compliance with quetiapine, risperidone, and other concomitant medications was monitored by subject self-report. Urinary drug screens were
used to monitor illicit drug use, and urinary cotinine levels discriminated tobacco use from non-use. There was a final clinic visit at week 14 for follow-up. Disposition of subjects is
shown in Figure 1. PLASMA LEVELS OF TC-5619, QUETIAPINE AND RISPERIDONE Serial and sparse blood sampling from a subset of subjects (_n_=62) was performed pre-dose and post-dose on day 1 and
weeks 4, 8, and 12 to estimate TC-5619 PK parameters and to document plasma levels of the concomitant antipsychotic medication with and without TC-5619 co-administration. Sample analyses
were performed using LC-MS/MS methods at Tandem Laboratories. All plasma samples were analyzed for TC-5619 levels (Salt Lake City, UT). All pre-dose samples were analyzed for either
quetiapine or risperidone and 9-hydroxy-risperidone (active metabolite) levels (Trenton, NJ). PK parameters were estimated for TC-5619, including _C_max, _T_max, and AUC to last collected
sample (8 h post-dose) and the dosing interval (extrapolated to 24 h post-dose). Plasma levels of the antipsychotic medication in the pre-dose samples were examined by cohort. STATISTICAL
ANALYSES The prospectively defined primary efficacy outcome measure was the change from day 1 to weeks 4, 8, and 12 in the Groton Maze Learning Task (GMLT) of the CSB, as filed to FDA and to
clinicaltrials.gov before study initiation. The CSB rather than other cognitive test batteries was used because of its shorter time for completion (20 min), its culturally neutral
computerized tasks (important for India), and its assessment of the seven cognitive domains judged important to CDS by the MATRICS initiative. The GMLT was chosen because it measures
executive function, the highest domain of cognitive function, and because CogState analyses of other alpha7 NNR agonists in previous studies showed that the GMLT was sensitive to effects
produced by this pharmacological class. Secondary outcomes included the CSB composite score, and scores for SANS, CGI-S, Clinical Global Impression-Global Improvement (CGI-I), and SGI-Cog.
Additional analyses included individual items of the CSB. Efficacy analysis was based on a mixed model repeated-measures methodology. The model considered change from baseline to weeks 4, 8,
and 12 as the response variable and included fixed effects for treatment, visit and treatment by visit interaction as well as baseline score and a random effect for center. Values reported
here use a 2-tailed test with an alpha of 0.05 in order to determine statistical significance. As this was an exploratory study, within-company success criteria for drug development
discussions were prospectively defined as _P_-values<0.10 (one-tailed) as specified in the FDA-submitted protocol. Outcomes were not corrected for multiplicity in this exploratory study.
For a number of CogState tasks (detection, identification, 1-card learning, and 1-back), data integrity criteria were specified _a priori_ to identify responses that reflect poor subject
cooperation. The analysis excluded subjects who failed to meet these criteria. Sample size calculations showed that 60 subjects should complete week 12 of the study to have a 90% power of
detecting a signal using a one-tailed test with an alpha of 0.10. As this study examined the efficacy of TC-5619 in both a tobacco user and a non-user cohort, 120 subjects were needed (60
per cohort) in order to be able to detect a signal in either of these cohorts. RESULTS EFFICACY PRIMARY EFFICACY OUTCOME MEASURE A blinded review by CogState during the study’s treatment
phase indicated a potentially greater-than-expected variance in the GMLT data, and analysis after database lock confirmed the existence of a positive skew to the GMLT data in the intent to
treat (ITT) population (sample skewness _g_1=1.03 in all patients at baseline). Consequently, a log (10) transformation of the GMLT data was performed (_g_1=−0.02). The treatment effect was
statistically significant in favor of TC-5619 (_P_=0.036, Week 4; Table 2), and the magnitude of the effect did not diminish following 12 weeks of randomized treatment (Cohen’s d for week 12
compared with day 1=0.40). The treatment effect in US patients (mean difference=0.082, 0.040, and 0.080 at 4, 8, and 12 weeks) was greater than the effect in Indian patients (mean
difference=0.020, 0.009, and 0.011 at 4, 8, and 12 weeks); this effect was significant at weeks 4 and 12 for US patients (_P_=0.0072, _P_=0.0044, respectively) but not for the Indian
patients (_P_>0.4 for all visits). The test for country (United States or India) by treatment interaction was not statistically significant (_P_=0.1577). This effect of TC-5619 was also
typically greater in tobacco users (Table 3). SECONDARY EFFICACY OUTCOME MEASURES Statistically significant results favoring TC-5619 in the ITT population were found in the SANS (_P_=0.030,
week 12; Cohen’s d for week 12 compared with day 1=0.26; Table 2). In the SGI-Cog, although the total score was not statistically significant, the attention/concentration item favored
TC-5619 (_P_=0.042). There was no drug effect identified in the ITT population in the other secondary outcome measures. The effect of TC-5619 was typically stronger in tobacco users (Table
3). The result in the SANS was driven by the avolition/apathy (_P_=0.110), anhedonia (_P_=0.062), and affective flattening (_P_=0.036) items. COGSTATE ANALYSES, TRAIL-MAKING TEST (TMT) A AND
B, DIGIT-SYMBOL SUBSTITUTION TEST (DSST) No measures in the CogState test battery, nor in the TMT or DSST, were statistically significant at the 0.05 level in the ITT population (Table 2).
A subgroup analysis of these data by tobacco use (Table 3) showed statistical significance in favor of TC-5619 in tobacco users on the 1-back test (ONB, a test of working memory: _P_=0.040,
week 12; Table 3). SAFETY AND TOLERABILITY ADVERSE EVENTS (AES) In all, 26% of subjects in the placebo cohort and 32% of subjects in the TC-5619 cohort reported AEs. All AEs were mild or
moderate in severity. AEs that were present in at least three subjects in either cohort were: constipation (2% placebo _vs_ 4% TC-5619); nausea (0% placebo _vs_ 5% TC-5619); body temperature
increased (2% placebo _vs_ 3% TC-5619); decreased appetite (5% placebo _vs_ 4% TC-5619); somnolence (2% placebo _vs_ 3% TC-5619); (worsening of) schizophrenia (2% placebo _vs_ 3% TC-5619);
headache (2% placebo _vs_ 3% TC-5619); and insomnia (0% placebo _vs_ 3% TC-5619). Nausea did not lead to discontinuation, and it was mild (_n_=4) or moderate (_n_=1) in severity. SERIOUS
ADVERSE EVENTS (SAES) Two SAEs were reported in the study, one in the placebo group (gastritis) and one in the TC-5619 group (acute exacerbation of schizophrenia). Both were considered not
drug related by the investigator. The subject with gastritis became dehydrated and was hospitalized to receive intravenous fluids. The subject with acute exacerbation of schizophrenia
stopped taking quetiapine and a week later was found wandering in the streets and acting bizarrely. He was hospitalized and treated. AES LEADING TO DISCONTINUATION Seven AEs led to
discontinuation, three in the placebo group and four in the TC-5619 group. All were considered not drug related by the investigator. In the placebo group, the events were: gastritis
(moderate), dermatitis (mild), and worsening schizophrenia (moderate). In the TC-5619 group, the events were: gastroenteritis (moderate), exacerbation of schizophrenia (two, moderate), and
exacerbation of psychotic symptoms (moderate). RESULTS OF THE CSSRS AND CDSS The CSSRS detected very low levels of suicidality during the trial between any visits, and all changes were in
the placebo cohort. The CDSS showed no meaningful change either within or between cohorts in the very low level of depression during the study. PHYSICAL EXAMINATION, AIMS, VITAL SIGNS,
LABORATORY ANALYTES, AND ECG There were no clinically meaningful changes between cohorts in physical examination, vital signs, orthostatic blood pressure changes, or urine or serum
laboratory measurements. The AIMS revealed no difference between cohorts in the very low mean severity of involuntary movements (AIMS score 0.1 in both cohorts on day 1 and at week 12).
There was no clinically meaningful difference in any ECG parameters or interpretations between cohorts. Mean QTcF values changed by a small and similar way in the cohorts between the
beginning (placebo: 394.4 ms pre-dose day 1; TC-5619: 392.9 ms pre-dose day 1) and end of the study (placebo: +1.6 ms post-dose week 12; TC-5619: +0.8 ms post-dose week 12). No QTcF values
were>480 ms in either cohort. PHARMACOKINETICS TC-5619 EXPOSURE LEVELS AND PHARMACOKINETIC PARAMETERS TC-5619 exposure, measured by steady-state concentrations (pre-dose (1.5–41.9 ng/ml)
and at _T_max (15.3–142 ng/ml)) and AUC24 h (129–1504 ng × hr/ml, estimated by extrapolation from 8-h collection time point), increased in a dose-dependent manner over the dose range. _T_max
(1.0–1.8 ng/ml) remained independent of dose. An analysis of the PK parameters of tobacco users and non-users was similar and could not account for differences in the effect of TC-5619
observed in the two sub-populations in the study. ANTIPSYCHOTIC EXPOSURE LEVELS Plasma levels of the concomitant antipsychotic were monitored in some subjects (_n_=62) to ensure that a
significant pharmacokinetic drug interaction could not contribute to observed efficacy. Levels of quetiapine and the ‘active moiety’ of risperidone (risperidone+9-hydroxy-risperidone levels;
(Risperdal prescribing information)) are presented (Table 4). Subjects were allowed to take any approved dose of antipsychotic, which contributed to the variability in levels. In addition,
several subjects in each antipsychotic subgroup did not have quantifiable antipsychotic levels, indicating either low doses or noncompliance with antipsychotic therapy. Subjects receiving
TC-5619 appeared to have lower (range of mean values: 208 to 284 nM) quetiapine levels than subjects receiving placebo (range of mean values: 512–743 nM). The number of subjects in the
analyzed quetiapine subgroup is small and differences in quetiapine doses or compliance across the two subgroups may have contributed to the observed differences in quetiapine levels between
the cohorts. Levels of active moiety of risperidone were similar among subjects receiving placebo and TC-5619. These findings indicate that a drug interaction did not contribute to the
effects observed in this study, because a lower quetiapine level in the TC-5619 group would be anticipated to produce smaller rather than greater beneficial effects in this cohort.
DISCUSSION There has been great interest and much effort to develop novel medications for the treatment of the cognitive and negative symptoms for which antipsychotic drugs are ineffective
(Gray et al, 2007; Miyamoto et al, 2005). In this context, nicotinic cholinergic receptors have emerged as priority targets and particularly the alpha7 and alpha4 beta2 NNRs (Freedman et al,
2008; Kucinski et al, 2011; Olincy et al, 2007; Ripoll et al, 2004). Although studies of the latter have yielded mixed results (Buchanan et al, 2008), studies of the former, using DMX-B and
EVP6124, have shown therapeutic potential in subjects with schizophrenia (EnVivo_Pharmaceuticals, 2009, 2011; Freedman et al, 2008; Olincy et al, 2006). The results of this exploratory
trial with TC-5619 are generally consistent with those of prior studies of alpha7 NNR partial agonists, and indicated statistically significant effects on the primary efficacy outcome (GMLT,
executive function) and on some secondary efficacy outcomes including SANS (negative symptoms). The results on the CSB task assessing working memory were statistically significant in favor
of TC-5619 in tobacco users. Although TC-5619 produced a statistically significant benefit in the ITT population on executive function as measured by the GMLT, it did not produce a
statistically significant benefit in the ITT population on the other six cognitive domains as measured in the CSB. Interestingly, despite the absence of a statistically significant benefit
of TC-5619 on the other six cognitive domains in the ITT population, there were statistically significant effects of TC-5619 on some of these other domains (eg, working memory, as measured
by the identification task) in the tobacco user cohort. The reason(s) for stronger effects of TC-5619 on executive function than on other cognitive domains is (are) unknown. TC-5619 was
generally well tolerated. Except for nausea, there were similar numbers of AEs, SAEs, and AEs leading to discontinuation. There were no clinically meaningful differences between cohorts in
suicidality, depression, physical examination, AIMS, vital signs, lab measurements of serum or urine analytes, or ECG. No differences in the drug levels between tobacco users and non-users
were observed to account for differences in efficacy between the two sub-populations. Antipsychotic levels across the TC-5619 and placebo groups were similar for risperidone, and we do not
believe that the difference in quetiapine would account for the effects observed. It is intriguing that the positive effects of TC-5619 were stronger in tobacco users. This finding may
pertain to observations that tobacco use is considerably higher in patients with schizophrenia than in the general population (de Leon et al, 1995; Goff et al, 1992; Hughes et al, 1986),
suggesting that these patients derive an NNR-mediated therapeutic benefit from nicotine. It is possible that the relatively small number of subjects in the study population caused this
finding in tobacco users to arise by chance. However, if this observation is confirmed by subsequent studies, at least three hypotheses may be invoked to explain this finding. First, alpha7
NNRs may be upregulated by tobacco use. In patients with schizophrenia who smoke, mRNA encoding the alpha7 NNR subtype was shown to be upregulated by 250% in comparison with patients who did
not smoke, and there were a greater number of functional alpha7 NNRs in smokers (Mexal et al, 2010). This finding suggests that there could be more alpha7 receptors in tobacco-users on
which TC-5619 could act. Second, nicotine increases blood–brain barrier permeability to small molecules in preclinical models (Hawkins et al, 2004; Manda et al, 2010), and hence a greater
brain concentration of TC-5619 may be present in tobacco users. Third, nicotine can act at NNR subtypes other than alpha7 (eg, alpha4 beta2) to enhance the effect of TC-5619 (Targacept, data
on file). These observed differences between tobacco users and non-users further underscore the complex and incompletely understood pharmacodynamic mechanisms by which alpha7 NNR agonists
work (Buchanan and Schwarcz, 2011). Recent studies have demonstrated how differences in dosing and schedule of administration, in addition to variation in the intrinsic activities of alpha7
NNR agonists, can influence cognitive and neurophysiological responses (Castner et al, 2011; Tregellas et al, 2011). If future studies confirm that TC-5619 or other alpha7 NNR agonists work
primarily in tobacco-using patients, it will be important to determine the pharmacodynamic basis of this effect. There is weak evidence suggesting that the positive effects of TC-5619 on
CogState items might be stronger in the United States than India, although the difference was not statistically significant. The modest difference between the effects in the US subjects
compared with Indian subjects could arise from the greater tobacco use in the US subjects (60%) than in the Indian subjects (38%). If the apparent difference in the magnitude of effect
between the US and Indian subjects is confirmed in future studies that equalize the percentage of tobacco users in the two geographic populations, it may instead reflect a cultural effect
and stem from relatively less familiarity of Indian subjects to computer-based tests. A number of caveats should be considered in the interpretation of this study. First, the number of
tobacco users in the study was relatively small (46% of the enrolled population), so the findings need to be replicated in larger studies. Second, approximately two-thirds of enrolled
subjects in this study were from sites in India, and therefore the findings need to be tested in other regions to assess translation into other populations, cultures, and ways of medical
practice. Nevertheless, these encouraging findings support the role of alpha7 NNR partial agonists like TC-5619 to treat the residual psychopathology of schizophrenia. An effective treatment
for these symptoms could be of great value for patients, their families and caregivers, and for the society and economy that could benefit from enhanced productivity of these individuals.
REFERENCES * Addington J, Addington D (1993). Premorbid functioning, cognitive functioning, symptoms and outcome in schizophrenia. _J Psychiatry Neurosci_ 18: 18–23. CAS PubMed PubMed
Central Google Scholar * American Psychiatric Association (2000) _Diagnostic and Statistical Manual of Mental Disorders_ 4th edn, Text Revision edn American Psychiatric Association:
Washington, DC. * Buchanan RW, Conley RR, Dickinson D, Ball MP, Feldman S, Gold JM _et al_ (2008). Galantamine for the treatment of cognitive impairments in people with schizophrenia. _Am J
Psychiatry_ 165: 82–89. Article PubMed Google Scholar * Buchanan RW, Schwarcz R (2011). Alpha7 nicotinic receptor agonists as cognitive treatments: is less (or less often) more? _Biol
Psychiatry_ 69: 5–6. Article PubMed Google Scholar * Castner SA, Smagin GN, Piser TM, Wang Y, Smith JS, Christian EP _et al_ (2011). Immediate and sustained improvements in working memory
after selective stimulation of alpha7 nicotinic acetylcholine receptors. _Biol Psychiatry_ 69: 12–18. Article CAS PubMed Google Scholar * Court J, Spurden D, Lloyd S, McKeith I, Ballard
C, Cairns N _et al_ (1999). Neuronal nicotinic receptors in dementia with Lewy bodies and schizophrenia: alpha-bungarotoxin and nicotine binding in the thalamus. _J Neurochem_ 73:
1590–1597. Article CAS PubMed Google Scholar * de Leon J, Dadvand M, Canuso C, White AO, Stanilla JK, Simpson GM (1995). Schizophrenia and smoking: an epidemiological survey in a state
hospital. _Am J Psychiatry_ 152: 453–455. Article CAS PubMed Google Scholar * EnVivo_Pharmaceuticals (2009). . EnVivo reports positive results of its EVP-6124 clinical biomarker study in
schizophrenia patients. * EnVivo_Pharmaceuticals (2011). . EnVivo announces positive phase 2b clinical data in schizophrenia: EVP 6124 meets primary endpoint with statistically significant
improvements in cognition and multiple secondary endpoints for improvement in function and impact on negative symptoms. * Erhart SM, Marder SR, Carpenter WT (2006). Treatment of
schizophrenia negative symptoms: future prospects. _Schizophr Bull_ 32: 234–237. Article PubMed PubMed Central Google Scholar * Fleischhacker W (2000). Negative symptoms in patients with
schizophrenia with special reference to the primary versus secondary distinction. _Encephale_ 1: 12–14. Google Scholar * Freedman R, Coon H, Myles-Worsley M, Orr-Urtreger A, Olincy A,
Davis A _et al_ (1997). Linkage of a neurophysiological deficit in schizophrenia to a chromosome 15 locus. _Proc Natl Acad Sci USA_ 94: 587–592. Article CAS PubMed PubMed Central Google
Scholar * Freedman R, Hall M, Adler LE, Leonard S (1995). Evidence in postmortem brain tissue for decreased numbers of hippocampal nicotinic receptors in schizophrenia. _Biol Psychiatry_
38: 22–33. Article CAS PubMed Google Scholar * Freedman R, Olincy A, Buchanan RW, Harris JG, Gold JM, Johnson L _et al_ (2008). Initial phase 2 trial of a nicotinic agonist in
schizophrenia. _Am J Psychiatry_ 165: 1040–1047. Article PubMed PubMed Central Google Scholar * Goff DC, Henderson DC, Amico E (1992). Cigarette smoking in schizophrenia: relationship to
psychopathology and medication side effects. _Am J Psychiatry_ 149: 1189–1194. Article CAS PubMed Google Scholar * Gold JM (2004). Cognitive deficits as treatment targets in
schizophrenia. _Schizophr Res_ 72: 21–28. Article PubMed Google Scholar * Gray JA, Roth BL (2007). Molecular targets for treating cognitive dysfunction in schizophrenia. _Schizophr Bull_
33: 1100–1119. Article PubMed PubMed Central Google Scholar * Hauser TA, Kucinski A, Jordan KG, Gatto GJ, Wersinger SR, Hesse RA _et al_ (2009). TC-5619: an alpha7 neuronal nicotinic
receptor-selective agonist that demonstrates efficacy in animal models of the positive and negative symptoms and cognitive dysfunction of schizophrenia. _Biochem Pharmacol_ 78: 803–812.
Article CAS PubMed PubMed Central Google Scholar * Hawkins BT, Abbruscato TJ, Egleton RD, Brown RC, Huber JD, Campos CR _et al_ (2004). Nicotine increases _in vivo_ blood-brain barrier
permeability and alters cerebral microvascular tight junction protein distribution. _Brain Res_ 1027: 48–58. Article CAS PubMed Google Scholar * Hughes JR, Hatsukami DK, Mitchell JE,
Dahlgren LA (1986). Prevalence of smoking among psychiatric outpatients. _Am J Psychiatry_ 143: 993–997. Article CAS PubMed Google Scholar * Kern RS, Nuechterlein KH, Green MF, Baade LE,
Fenton WS, Gold JM _et al_ (2008). The MATRICS Consensus Cognitive Battery, part 2: co-norming and standardization. _Am J Psychiatry_ 165: 214–220. Article PubMed Google Scholar *
Kucinski AJ, Stachowiak MK, Wersinger SR, Lippiello PM, Bencherif M (2011). Alpha7 neuronal nicotinic receptors as targets for novel therapies to treat multiple domains of schizophrenia.
_Curr Pharm Biotechnol_ 12: 437–448. Article CAS PubMed Google Scholar * Luntz-Leybman V, Bickford PC, Freedman R (1992). Cholinergic gating of response to auditory stimuli in rat
hippocampus. _Brain Res_ 587: 130–136. Article CAS PubMed Google Scholar * Manda VK, Mittapalli RK, Bohn KA, Adkins CE, Lockman PR (2010). Nicotine and cotinine increases the brain
penetration of saquinavir in rat. _J Neurochem_ 115: 1495–1507. Article CAS PubMed Google Scholar * Marder SR, Fenton W (2004). Measurement and treatment research to improve cognition in
schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. _Schizophr Res_ 72: 5–9. Article PubMed Google Scholar * Mexal S,
Berger R, Logel J, Ross RG, Freedman R, Leonard S (2010). Differential regulation of alpha7 nicotinic receptor gene (CHRNA7) expression in schizophrenic smokers. _J Mol Neurosci_ 40:
185–195. Article CAS PubMed Google Scholar * Miyamoto S, Duncan GE, Marx CE, Lieberman JA (2005). Treatments for schizophrenia: a critical review of pharmacology and mechanisms of action
of antipsychotic drugs. _Mol Psychiatry_ 10: 79–104. Article CAS PubMed Google Scholar * Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK (2004). Identification of
separable cognitive factors in schizophrenia. _Schizophr Res_ 72: 29–39. Article PubMed Google Scholar * Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD _et al_ (2008).
The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. _Am J Psychiatry_ 165: 203–213. Article PubMed Google Scholar * O’Carroll R (2000). Cognitive
impairment in schizophrenia. _Adv Psychiatric Treatment_ 6: 161–168. Article Google Scholar * Ojeda N (2000). Course of cognitive symptoms in schizophrenia: a review of the literature.
_Actas Esp Psiquiatr_ 35: 263–270. Google Scholar * Olincy A, Harris JG, Johnson LL, Pender V, Kongs S, Allensworth D _et al_ (2006). Proof-of-concept trial of an alpha7 nicotinic agonist
in schizophrenia. _Arch Gen Psychiatry_ 63: 630–638. Article CAS PubMed Google Scholar * Olincy A, Stevens KE (2007). Treating schizophrenia symptoms with an alpha7 nicotinic agonist,
from mice to men. _Biochem Pharmacol_ 74: 1192–1201. Article CAS PubMed PubMed Central Google Scholar * Reichenberg A, Caspi A, Harrington H, Houts R, Keefe RS, Murray RM _et al_
(2010). Static and dynamic cognitive deficits in childhood preceding adult schizophrenia: a 30-year study. _Am J Psychiatry_ 167: 160–169. Article PubMed PubMed Central Google Scholar *
Reichenberg A, Harvey PD (2007). Neuropsychological impairments in schizophrenia: integration of performance-based and brain imaging findings. _Psychol Bull_ 133: 833–858. Article PubMed
Google Scholar * Ripoll N, Bronnec M, Bourin M (2004). Nicotinic receptors and schizophrenia. _Curr Med Res Opin_ 20: 1057–1074. Article CAS PubMed Google Scholar * Stahl SM, Buckley PF
(2007). Negative symptoms of schizophrenia: a problem that will not go away. _Acta Psychiatr Scand_ 115: 4–11. Article CAS PubMed Google Scholar * Tandon R, Nasrallah HA, Keshavan MS
(2009). Schizophrenia, ‘just the facts’ 4. Clinical features and conceptualization. _Schizophr Res_ 110: 1–23. Article PubMed Google Scholar * Tregellas JR, Tanabe J, Rojas DC, Shatti S,
Olincy A, Johnson L _et al_ (2011). Effects of an alpha 7-nicotinic agonist on default network activity in schizophrenia. _Biol Psychiatry_ 69: 7–11. Article CAS PubMed Google Scholar
Download references ACKNOWLEDGEMENTS We thank Gaston Farr for clinical operations, Grace Li for statistical programming, LaTonya Bufford for data management, Dorothea Gibbs for trial
document management, Pete Zorn for thorough and expert review of the manuscript, and Katherine Pickett for administrative assistance. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department
of Psychiatry, Columbia College of Physicians and Surgeons, New York, NY, USA Jeffrey A Lieberman, Ragy R Girgis & Naihua Duan * Clinical Development and Regulatory Affairs, Targacept,
Winston-Salem, NC, USA Geoffrey Dunbar, Anthony C Segreti, Frances Seoane, Jessica S Beaver & David A Hosford Authors * Jeffrey A Lieberman View author publications You can also search
for this author inPubMed Google Scholar * Geoffrey Dunbar View author publications You can also search for this author inPubMed Google Scholar * Anthony C Segreti View author publications
You can also search for this author inPubMed Google Scholar * Ragy R Girgis View author publications You can also search for this author inPubMed Google Scholar * Frances Seoane View author
publications You can also search for this author inPubMed Google Scholar * Jessica S Beaver View author publications You can also search for this author inPubMed Google Scholar * Naihua Duan
View author publications You can also search for this author inPubMed Google Scholar * David A Hosford View author publications You can also search for this author inPubMed Google Scholar
CORRESPONDING AUTHOR Correspondence to Jeffrey A Lieberman. ETHICS DECLARATIONS COMPETING INTERESTS Drs Girgis and Duan also have no personal financial disclosures that are relevant to this
work. Dr Lieberman serves on the Advisory Board of Bioline, Intracellular Therapies, and PsychoGenics. He does not receive direct financial compensation or salary support for participation
in research, consulting, or advisory board activities. He receives grant support from Allon, F Hoffman-La Roche, GlaxoSmithKline, Eli Lilly, Merck, Novartis, Pfizer, Psychogenics, Sepracor
(Sunovion) and Targacept; and he holds a patent from Repligen. Dr Segreti and Dr Hosford are employees of Targacept, own Targacept stock, and have Targacept stock options. The remaining
authors are employed by the sponsor of this study, Targacept, and own shares of the common stock and/or options to purchase shares of the common stock of Targacept. These data were
previously presented at the International Congress of Schizophrenia Research (Colorado Springs, CO; April 2011); at the NCDEU Annual Meeting (Boca Raton, FLA; June 2011); and at the American
College of Neuropsychopharmacology Annual Meeting (ACNP; Hawaii; December 2011). ADDITIONAL INFORMATION These data were previously presented at the International Congress of Schizophrenia
Research (Colorado Springs, CO; April 2011); at the NCDEU Annual Meeting (Boca Raton, FL; June 2011); and at the American College of Neuropsychopharmacology Annual Meeting (ACNP; Hawaii;
December 2011). POWERPOINT SLIDES POWERPOINT SLIDE FOR FIG. 1 RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Lieberman, J., Dunbar, G., Segreti, A. _et
al._ A Randomized Exploratory Trial of an Alpha-7 Nicotinic Receptor Agonist (TC-5619) for Cognitive Enhancement in Schizophrenia. _Neuropsychopharmacol_ 38, 968–975 (2013).
https://doi.org/10.1038/npp.2012.259 Download citation * Received: 14 September 2012 * Revised: 30 November 2012 * Accepted: 03 December 2012 * Published: 18 December 2012 * Issue Date: May
2013 * DOI: https://doi.org/10.1038/npp.2012.259 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is
not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * schizophrenia * alpha7 nicotinic receptor * TC-5619
* cognitive function * negative symptoms * clinical trial
