Increased piezo1 channel activity in interstitial cajal-like cells induces bladder hyperactivity by functionally interacting with ncx1 in rats with cyclophosphamide-induced cystitis
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT The Piezo1 channel is a mechanotransduction mediator, and Piezo1 abnormalities have been linked to several clinical disorders. However, the role of the Piezo1 channel in
cystitis-associated bladder dysfunction has not been documented. The current study aimed to discover the functional role of this channel in regulating bladder activity during
cyclophosphamide (CYP)-induced cystitis. One hundred four female rats were randomly assigned to the control, CYP-4h, CYP-48h and CYP-8d groups. CYP successfully induced acute or chronic
cystitis in these rats. CYP treatment for 48h or 8d significantly increased Piezo1 channel expression in bladder interstitial Cajal-like cells (ICC-LCs), and the increase in CYP-8d rats was
more prominent. In addition, 2.5 μM Grammostola spatulata mechanotoxin 4 (GsMTx4) significantly attenuated bladder hyperactivity in CYP-8d rats by inhibiting the Piezo1 channel in bladder
ICC-LCs. Furthermore, by using GsMTx4 and siRNA targeting the Piezo1 channel, we demonstrated that hypotonic stress-induced Piezo1 channel activation significantly triggered Ca2+ and Na+
influx into bladder ICC-LCs during CYP-induced chronic cystitis. In addition, the Piezo1 channel functionally interacted with the relatively activated reverse mode of Na+/Ca2+ exchanger 1
(NCX1) in bladder ICC-LCs from CYP-8d rats. In conclusion, we suggest that the functional role of the Piezo1 channel in CYP-induced chronic cystitis is based on its synergistic effects with
NCX1, which can significantly enhance [Ca2+]i and result in Ca2+ overload in bladder ICC-LCs, indicating that the Piezo1 channel and NCX1 are potential novel therapeutic targets for chronic
cystitis-associated bladder hyperactivity. SIMILAR CONTENT BEING VIEWED BY OTHERS EXCITATORY PURINERGIC AND CHOLINERGIC EXPRESSION CHANGED IN A PARTIAL BLADDER OUTLET OBSTRUCTION-INDUCED
OVERACTIVE BLADDER RAT MODEL Article Open access 26 October 2023 ROLE OF DETRUSOR PDGFRΑ+ CELLS IN MOUSE MODEL OF CYCLOPHOSPHAMIDE-INDUCED DETRUSOR OVERACTIVITY Article Open access 24 March
2022 SPINAL CRH FACILITATES THE MICTURITION REFLEX VIA THE CRH2 RECEPTOR IN RATS WITH NORMAL BLADDER AND BLADDER OUTLET OBSTRUCTION Article Open access 29 January 2025 INTRODUCTION
Interstitial cystitis/painful bladder syndrome (IC/PBS) is a clinical syndrome characterized by chronic pelvic pain and other micturition symptoms, such as frequency, urgency, and nocturia1.
The prevalence of IC/PBS ranges from 1 in 100 000 to 5.1 in 1000 in the worldwide population2. The etiology and pathophysiology of IC/BPS are poorly understood, and the therapeutic
strategies against this disorder are still limited and unsatisfactory3. Therefore, more research is needed to clarify the pathogenesis of IC/BPS In recent years, increasing evidence has
demonstrated that bladder interstitial Cajal-like cells (ICC-LCs), which display many of the morphological features of gastrointestinal interstitial Cajal cells (ICCs), play a crucial role
in regulating bladder activity4,5,6,7,8. Two populations of ICC-LCs have been identified, including ICC-LCs in the lamina propria (LP, area between the urothelium and detrusor smooth muscle)
and ICC-LCs in the detrusor (intramuscular and interbundle)9. The functional character of bladder ICC-LCs has not been completely clarified. The common hypothesis is that ICC-LCs in the LP
primarily play a role in nonneural sensory signal transduction from the urothelium to the detrusor, whereas detrusor ICC-LCs might be involved in pacemaking and/or transduction of pacemaking
signals in the detrusor10. It has been shown that abnormalities in bladder ICC-LC quantity and function are involved in several bladder disorders, such as bladder outlet obstruction,
diabetic cystopathy, and neurogenic bladder11. The data on functional changes in IC/PBS are still limited. Although we have found that bladder ICC-LC hyperactivity induced by alterations in
the hyperpolarization-activated cyclic nucleotide 1 (HCN1) channel are involved in cyclophosphamide (CYP)-induced cystitis12, investigations attempting to more comprehensively elucidate the
mechanisms underlying the functional role of bladder ICC-LCs in cystitis will be beneficial in developing more therapeutic strategies for cystitis-associated bladder dysfunction. Piezo
proteins, including Piezo1 and Piezo2, have recently been identified as mechanically activated cation channels in mammalian cells13. In vertebrates, the Piezo2 channel mediates gentle touch
sensation, whereas the Piezo1 channel has multiple roles in various physiological processes, including regulating vascular development, controlling cell migration and differentiation,
maintaining blood pressure, and triggering rapid epithelial cell division14,15,16. Aberrant Piezo1 channel activity has been linked to several diseases, such as hereditary xerocytosis17, 18,
generalized lymphatic dysplasia19, and heart failure20. In the bladder, the Piezo1 channel is found to be associated with the Ca2+ influx and ATP release in urothelial cells21, and its
expression is significantly increased in rats after partial bladder outlet obstruction (PBOO)22. The functional changes in the Piezo1 channel in other bladder dysfunctions, such as IC, need
to be further explored. To date, several animal models that mimic IC/BPS symptoms have been well-established using CYP, potassium chloride (KCl), protamine sulfate, lipopolysaccharide (LPS),
and immunogenic peptide, among others23,24,25,26. Among these, CYP-induced cystitis is one of the most commonly used models23, 27. In this study, we used this model and demonstrated that
increased Piezo1 channel activity in bladder ICC-LCs is a crucial factor for CYP-induced cystitis-associated bladder hyperactivity. The functional role of the Piezo1 channel is based on its
synergistic effects with Na+/Ca2+ exchanger 1 (NCX1), which significantly enhances the intracellular Ca2+ concentration, leading to Ca2+ overload in bladder ICC-LCs. MATERIALS AND METHODS
ANIMALS Female Sprague–Dawley (SD) rats (220–250 g) were purchased from Experimental Animals Center of Third Military Medical University (Chongqing, China). Initially, 24 rats were randomly
assigned to control, CYP-4h, CYP-48h, and CYP-8d groups. For further research, 80 rats were randomly assigned into the control and CYP-8d groups. All rats were maintained in light-controlled
(12-h light/dark cycle) cages with free access to rodent chow and water. All experimental procedures were approved by the Research Council and Animal Care and Use Committee of the Third
Military Medical University, China and were performed in accordance with the Guide for the Care and Use of Laboratory Animals published by the National Institutes of Health. INDUCTION OF
CYP-INDUCED CYSTITIS Rat models of CYP-induced cystitis were established according to previously described protocols28, 29. To induce acute cystitis, rats in the CYP-4h and CYP-48h groups
received a single administration (150 mg/kg; intraperitoneally) of CYP (Sigma, St Louis, MO, USA) and were sacrificed 4 or 48 h after CYP administration. Chronic cystitis was induced by
three injections of low-dose CYP. Rats in the CYP-8d and control groups received the administration of CYP (75 mg/kg; intraperitoneally) or an equal volume of vehicle (sterile saline) on
days 1, 4, and 7 and were sacrificed 24 h after the last CYP administration. HEMATOXYLIN AND EOSIN (H&E) STAINING Bladders isolated from sacrificed rats were sequentially fixed with 4%
paraformaldehyde, dehydrated, embedded in paraffin, and cut into 4-µm sections. Then, the sections were deparaffinized and rehydrated in a graded ethanol series. H&E staining was
performed according to a standard protocol30. WESTERN BLOT ANALYSIS Rat bladders were lysed in RIPA lysis buffer (Beyotime, Shanghai, China) to extract total protein. Protein concentrations
were measured with a Bio-Rad DC Protein Assay Kit (Bio-Rad, Hercules, USA). Then, 50 μg protein aliquots were separated using 8–12% sodium dodecyl sulfate polyacrylamide gel electrophoresis
(SDS-PAGE) gels and transferred to polyvinylidene fluoride (PVDF) membranes (Merck Millipore, Darmstadt, Germany). After being blocked with 5% skim milk dissolved in Tris-buffered saline at
room temperature for 2 h, the membranes were incubated overnight at 4 °C with various primary antibodies targeting the following proteins: IL-6 (Abcam, Cambridge, UK, ab9324, 1:800), TNF-α
(Abcam, ab199013, 1:500), Piezo1 (Alomone labs, Jerusalem, Israel, APC-087, 1:500), NCX1 (Abcam, ab2869, 1:800), NCX2 (Alomone labs, ANX-012, 1:500), NCX3 (Alomone labs, ANX-013, 1:500),
glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (Beyotime, AG019, 1:1000), and α-tubulin (Beyotime, AT819, 1:1000). Following incubation with horseradish peroxidase-conjugated secondary
antibodies (Zhongshan Co., Beijing, China, ZB-2301, ZB-2305, 1:5000), antibody–antigen complexes were detected using an ECL substrate (Millipore, Billerica, USA) and visualized with an Image
Quant LAS-4000 BioImaging System (GE Healthcare, Stockholm, Sweden). QUANTITATIVE REVERSE TRANSCRIPTION-PCR (RT-PCR) Total RNA was isolated from rat bladders using TRIzol reagent (Takara,
Dalian, China) according to the manufacturer’s protocol. Total RNA (2 μg) was subsequently reverse transcribed to complementary DNA (cDNA) using a PrimeScript™ RT reagent kit (Takara). The
primers used in our study are listed in Table S1. Quantitative real-time PCR was performed using SYBR Green mix (Toyobo, Osaka, Japan) in a StepOnePlus Real-Time PCR system (Life
Technologies, Carlsbad, CA). The thermocycling program was run as follows: 95 °C for 30 s, 95 °C for 5 s, 60 °C for 10 s, and 72 °C for 15 s (40 cycles). Gene expression was normalized to
GAPDH expression and the fold changes were calculated using the 2-△△Ct method. The negative control was performed without templates. IMMUNOHISTOCHEMISTRY (IHC) For IHC, bladder sections
stained with H&E were incubated overnight at 4 °C with primary antibody against Piezo1 (Alomone labs, APC-087, 1:100). Phosphate-buffered saline (PBS) was substituted for the primary
antibody as a negative control. Following incubation with primary antibody, the sections were incubated with a streptavidin–biotin peroxidase (SP)-conjugated secondary goat anti-rabbit IgG
from a standard SP kit (Zhongshan Co., SPN-9002) for 30 min at 37 °C. Finally, the sections were stained with diaminobenzidine (DAB) (Zhongshan Co., ZLI-9019) and counterstained with
hematoxylin. All sections were visualized and photographed with an optical microscope (Olympus) and evaluated by two individuals in a double-blind manner. IMMUNOFLUORESCENCE (IF) STAINING
After being snap frozen, the isolated rat bladders were cut into 6-µm sections on a freezing microtome. For IF staining, these tissue sections and cells on coverslips were fixed with 4%
paraformaldehyde (Boster, Wuhan, China) for 30 min and then washed in PBS (10 min × 3 times). After being blocked with immunostaining blocking buffer (Beyotime, Shanghai, China) for 1 h,
tissue sections and cells were incubated overnight at 4 °C with primary antibodies targeting the following proteins: C-kit (Santa Cruz, Dallas, TX, USA, sc-1494, 1:50), Piezo1 (Alomone labs,
APC-087, 1:100) and NCX1 (Abcam, ab2869, 1:100), or with PBS as the negative control. Afterward, the tissue sections and cells were incubated at room temperature for 90 min with appropriate
secondary antibodies (Alexa 488-conjugated mouse anti-goat IgG (Bioss, Beijing, China, 1:200) or goat anti-mouse IgG (Beyotime, 1:200) and Alexa 647-conjugated donkey anti-mouse IgG or
donkey anti-rabbit IgG (Bioss, 1:200)) and then incubated with 2-(4-amidinophenyl)-6-indolecarbamidine dihydrochloride (DAPI, Beyotime) to label cytoblasts. Each incubation step was followed
by PBS washes (5 min × 3 times). All tissue sections and cells were viewed and photographed with a laser-scanning confocal microscope (Leica, Wetzlar and Mannheim, Germany). URODYNAMIC
MEASUREMENTS Urodynamic measurements were performed in unconscious rats as previously described31. Rats were anesthetized with an intraperitoneal injection of urethane (1 g/kg). A PE-50
polyethylene catheter was inserted into the bladder dome via a mid-line abdominal incision, and a purse-string suture was utilized to close the bladder dome incision tightly. The other end
of the PE-50 catheter (Becton Dickinson & Company, Franklin Lakes, New Jersey, USA) was connected to a pressure transducer (Chengyi Co., Chengdu, China) and an infusion pump (AVI 270, 3
M, Saint Paul, MN, USA) with a three-way connector. Physiological saline containing Grammostola spatulata mechanotoxin 4 (GsMTx4, Piezo1 antagonist, 2.5 μM, Abcam) or dimethyl sulfoxide
(DMSO) (Beyotime) at room temperature was infused into the bladder at a constant rate (10 mL/h). Continuous urodynamic curves were digitized and recorded using a multichannel signal
processing system (RM6240C, Chengyi Co.). The maximum bladder pressure (MBP) and intercontractile interval (ICI) were analyzed, which represent the bladder contractility and voiding
frequency, respectively. CONTRACTILITY STUDIES The whole bladder was carefully resected from each sacrificed rat and placed in Kreb’s solution containing the following compounds (in mM): 119
NaCl, 4.7 KCl, 1.2 KH2PO4, 1.2 MgSO4•7H2O, 25 NaHCO3, 2.5 CaCl2 and 11 glucose, adjusted to pH 7.4 with NaOH. Then, bladders were longitudinally cut into 3 × 4 × 8 mm strips. Each strip was
suspended vertically in a 15-mL organ bath filled with 37 °C Kreb’s solution and maintained in a mixture of 95% O2 and 5% CO2. One end of each strip was fixed to the bottom of the bath, and
the other end was linked with the tension transducer. After equilibration for 30 min, 0.75 g of tension was applied to each strip to elicit spontaneous contraction, and stable continuous
curves were visualized and recorded in the RM6240C signal processing system (Chengyi Co.). Pharmaceuticals, including GsMTx4 (2.5 μM), the c-kit blocker imatinib mesylate (Glivec, 100 μM,
Sigma, St Louis, MO, USA), the NCX reverse mode inhibitor (KB-R7943, 10 μM, Sigma) and the vehicle (DMSO), were added to the bathing solution at 6-min intervals. BLADDER ICC-LC ISOLATION Rat
bladders were aseptically resected and washed in sterile Ca2+-free Hank’s solution (Boster). After the urothelium layer was removed, bladders were cut into small fragments and digested at
37 °C for 5 min in 5 mL of enzyme solution containing the following reagents (mg/mL): 2.0 type II collagenase, 2.0 bovine serum albumin (BSA) and 2.0 trypsin inhibitor (all were purchased
from Sigma). To terminate digestion, RMPI-1640 medium (HyClone, Logan, USA) containing 10% fetal bovine serum (Gibco-Life Technologies, Grand Island, NY, USA) was added to the enzyme
solution. Afterward, the isolated cells were filtered via a 200-mesh cell strainer and plated onto sterile polylysine-coated glass coverslips or laser confocal dishes. The cells were
cultured at 37 °C in a 95% O2 and 5% CO2 incubator in RMPI-1640 medium supplemented with 10% fetal bovine serum and 1% antibiotics/antimycotics (Beyotime). MEASUREMENT OF INTRACELLULAR
CALCIUM AND SODIUM CONCENTRATIONS ([CA2+]I AND [NA+]I) [Ca2+]i and [Na+]i measurements were conducted on isolated bladder ICC-LCs that were cultured for 2–3 days. Bladder ICC-LCs were washed
with Hank’s solution (Boster) for 5 min and then incubated with Fluo-4 AM (for [Ca2+]i measurement, 10 μM, Molecular Probes, Eugene, OR, USA) or SBFI-AM (for [Na+]i measurement, 10 μM,
Sigma) for 30 min at 37 °C. After incubation, the bladder ICC-LCs were washed thrice in Hank’s solution for 5 min. Bladder ICC-LCs were distinguished according to their distinctive
morphology: stellate- or elongated-shaped, with several branches9. Ca2+ and Na+ imaging was performed on the laser-scanning confocal microscope (Leica, Germany). The excitation wavelength
for [Ca2+]i measurement and [Na+]i measurement was 488 nm and 405 nm, respectively. After imaging for 1 min, the effects of hypotonic stress with or without GsMTx4 (2.5 μM) on bladder ICC-LC
real-time [Ca2+]i and [Na+]i were detected, and the effects of hypotonic stress on real-time [Ca2+]i and [Na+]i in small interfering RNA (siRNA)-treated bladder ICC-LCs were also tested.
The results are presented as relative fluorescence intensities (RFI = F1/F0, where F0 is the baseline fluorescence intensity before hypotonic stress application, and F1 is the real-time
fluorescence intensity after hypotonic stress application). In the [Ca2+]i and [Na+]i measurements, to activate the Piezo1 channel, we applied hypotonic stress to bladder ICC-LCs similar to
previous reports32. The Hank’s solution used comprised the following (in mM): 138 NaCl, 5.33 KCl, 4.17 NaHCO3, 0.441 KH2PO4, 0.338 NaH2PO4, 1.26 CaCl2, 0.407 MgSO4, 0.493 MgCl2 and 5.56
d-glucose, pH 7.4 (308 mOsm/L). First, we prepared a low NaCl solution (113 mOsm/L) by decreasing the NaCl concentration to 45 mM in the Hank’s solution. Isotonic (300 mOsm/L) and hypotonic
(120 mOsm/L) solutions were prepared by adding 187 mM mannitol and 7 mM mannitol, respectively, to the low NaCl solution. In the [Ca2+]i and [Na+]i measurements, bladder ICC-LCs were
initially maintained in 100 μL of isotonic solution (300 mOsm/L). After imaging for 1 min, 100 μL of hypotonic solution (120 mOsm/L) was added to the isotonic solution to obtain the final
hypotonic solution (210 mOsm/L). PATCH-CLAMP EXPERIMENTS Bladder ICC-LCs were routinely cultured for 2–3 days and identified according to their distinctive morphology, as described above.
INCX was recorded in the whole-cell patch-clamp mode. Glass electrodes possessing approximate resistances of 4–6 MΩ were pulled from a Model P-97 Flaming/Brown Micropipette Puller (Sutter
Instrument Co., Novato, CA, USA). For recording, the glass electrodes were filled with pipette solution containing the following compounds (in mM): 51 NaCl, 100 CsOH, 5 KCl, 2 MgCl, 4.94
CaCl2, 20 tetraethylammonium Cl, 10 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES), 1 adenosine 5′-triphosphate disodium salt hydrate (Na2ATP), 5 ethylene glycol tetraacetic acid
(EGTA), and 8 d-glucose (pH 7.2). Bladder ICC-LCs were maintained in bath solution containing the following compounds (in mM): 137 NaCl, 5 KCl, 1.5 CaCl2,1 MgCl2, 10 HEPES, and 10 d-glucose
(312 mOsm/L, pH 7.4). To continuously activate the Piezo1 channel with hypotonic stress, the osmotic pressure in the bath solution was changed to 200 mOsm/L by adjusting the NaCl
concentration to 81 mM. GsMTx4 (2.5 μM) was added to the bath solution to block the Piezo1 channel. INCX was elicited by a step potential ranging from −100 to + 60 mV in increments of 10 mV
for 200 ms, with a holding potential of -40 mV. INCX was amplified and recorded using a HEKA EPC10USB amplifier (HEKA Elektronik, Heidelberg, Germany) and filtered at a threshold frequency
of 2.9 kHz. The data were analyzed using FitMaster software (HEKA Elektronik) and the density of INCX was normalized to cell capacitance. SINGLE-CELL RT-PCR We performed single-cell RT-PCR
to confirm the authenticity of isolated bladder ICC-LCs, according to our previous description12. After electrophysiological testing, a single bladder ICC-LC was sucked into the recording
pipette by applying negative pressure. Subsequently, the collected bladder ICC-LC was expelled instantly into NP-40 lysis buffer (Beyotime) containing RNAase inhibitor (Beyotime). After
being centrifuged at 4 °C for 30 s with 1000 r.p.m., each cell was lysed on ice for 20 min. Single-stranded cDNA was synthesized using a Sensiscript RT Kit (Qiagen, Hilden, Germany)
according to the manufacturer’s instructions. The primers used in this experiment are listed in Table S1. The thermocycling procedure was set up as follows: 94 °C for 1 min, 94 °C for 30 s,
60 °C for 30 s, and 72 °C for 1 min (40 cycles). The negative control reaction was performed by removing templates. Amplification products were viewed via GoldView (SBS Genetech Co.,
Beijing, China) staining in 1.5% agarose gels. Only the INCX values recorded in c-kit-positive cells were included in the statistical analysis. CO-IMMUNOPRECIPITATION (CO-IP) ANALYSIS Whole
bladders removed from rats in the CYP-8d group were separately lysed with RIPA lysis buffer (Beyotime) and centrifuged at 12,000 rpm at 4 °C for 30 min to collect the supernatant. The
lysates were precleared with Dynabeads Protein G magnetic beads (Thermo Fisher Scientific) at 4 °C for 15 min and then incubated with anti-Piezo1 (Alomone labs) and anti-NCX1 (Abcam) primary
antibodies or negative control IgG overnight at 4 °C. Sequentially, immunocomplexes were precipitated with Dynabeads Protein G magnetic beads. After the beads were washed with PBS
containing 0.1% (v/v) TX-100 (Beyotime) three times, the precipitates were loaded onto SDS-PAGE gels for western blot analysis. RNA INTERFERENCE To knockdown endogenous Piezo1 channel
expression, siRNA targeting rat Piezo1 or negative control siRNA (both purchased from Genema, Shanghai, China) were used to transfect isolated bladder ICC-LCs at 0.2 μM concentration with
Lipofectamine 2000 (Thermo Fisher Scientific, Waltham, MA, USA). The siRNA sequences were as follows: siRNA-Piezo1, (forward) 5′-CGGCCAACAUAAAGAACAUTT-3′ and (reverse)
5′-AUGUUCUUUAUGUUGGCCGTT-3′; negative control siRNA, (forward) 5′-UUCUCCGAACGUGUCACGUTT-3′ and (reverse) 5′-ACGUGACACGUUCGGAGAATT-3′. After transfection for 48 h, quantitative RT-PCR and IF
staining were used to detect the interference efficiency. siRNA-treated bladder ICC-LCs were subsequently utilized for [Ca2+]i or [Na+]i measurement and electrophysiological recordings.
STATISTICAL ANALYSIS The data are presented as the mean ± S.D. Statistical analyses were performed with SPSS 16.0 software (SPSS Inc., Chicago, IL), and significant differences between each
group were calculated using unpaired two-tailed Student’s _t-_tests or one-way analysis of variance. _P_ < 0.05 was considered statistically significant. All experiments were performed
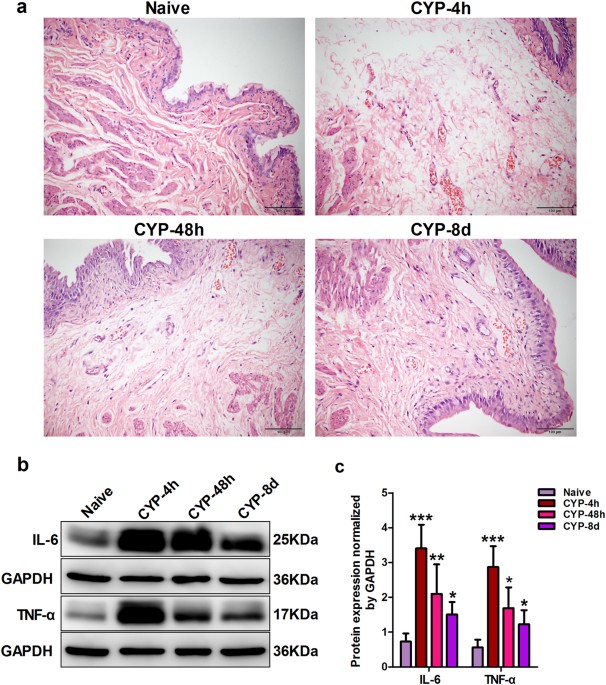
with at least three independent replications. RESULTS RAT MODELS WITH CYP-INDUCED CYSTITIS WERE SUCCESSFULLY ESTABLISHED To test whether the CYP-induced cystitis models were successfully
established in rats, H&E staining was primarily performed on rat bladder sections from four groups: control, CYP-4h, CYP-48h, and CYP-8d groups. Compared with that from the control rats,
bladder sections from CYP-4h and CYP-48h rats (acute cystitis models) exhibited severe edema and hyperemia in the LP, and bladder sections from CYP-8d rats (chronic cystitis model) showed
moderate edema and hyperemia in the LP accompanied by urothelial hyperplasia (Fig. 1a). Furthermore, we found that the protein levels of two inflammation-associated cytokines (interleukin-6
(IL-6) and tumor necrosis factor-α (TNF-α)) in CYP-4h, CYP-48h, and CYP-8d rats were all significantly higher than those in the control group, and the increase in CYP-4h and CYP-48h rats was
more obvious than that in CYP-8d rats (Fig. 1b, c). Meanwhile, we found that CYP-8d rats exhibited obvious urodynamic abnormalities characterized by a significant increase in MBP and a
significant decrease in ICI compared with naive rats (Figure S1 a–c). Furthermore, isolated detrusor strips from CYP-8d rats showed more vigorous spontaneous contractions than those from
naive rats (Figure S1d and c). These data indicated that rat models with CYP-induced cystitis were successfully established. PIEZO1 CHANNEL EXPRESSION WAS SIGNIFICANTLY INCREASED IN BLADDER
ICC-LCS FROM CYP-48H AND CYP-8D RATS Herein, we first found that protein and mRNA levels of Piezo1 channel were significantly increased in whole bladders from the CYP-48h and CYP-8d rats,
and those levels in CYP-8d rat bladders were more prominent. These phenomena were not detected in the CYP-4h rats (Fig. 2a–c). Moreover, consistent results were detected with IHC staining,
in which Piezo1 channel expression in bladder sections from CYP-48h and CYP-8d rats was significantly higher than that in bladder sections from control and CYP-4h rats, and the changes in
CYP-8d rats were more remarkable. Interestingly, we found that increases in Piezo1 channel expression were mainly present in the urothelium and mesenchymal layers (LP and intermuscular
region) but not in detrusor smooth muscle cells (Fig. 2d). To the best of our knowledge, bladder ICC-LCs are located in the LP and intermuscular region, and thus, we further focused on
whether Piezo1 channel expression was upregulated in bladder ICC-LCs. The IF staining results showed that the Piezo1 channel was expressed in bladder ICC-LCs, and Piezo1 channel expression
was significantly enhanced in both the LP ICC-LCs and detrusor ICC-LCs in CYP-48h and CYP-8d rat bladders compared with that in control and CYP-4h rat bladders. Consistently, the increases
in bladder ICC-LCs in CYP-8d rats were more prominent (Fig. 2e). GSMTX4 SIGNIFICANTLY DECREASED BLADDER HYPERACTIVITY IN CYP-8D RATS BY INHIBITING THE PIEZO1 CHANNEL IN BLADDER ICC-LCS We
used the Piezo1 channel inhibitor GsMTx4 to test whether increased Piezo1 channel activity was involved in the bladder hyperactivity in CYP-8d rats. Upon GsMTx4 (2.5 μM) administration, the
MBP was significantly reduced and the ICI was significantly extended in naive and CYP-8d rats. The effects of GsMTx4 administration on MBP and ICI in naive rats were less obvious than in
CYP-8d rats (Fig. 3a–c). In contractility studies, we found that GsMTx4 significantly decreased the phasic amplitude of spontaneous contractions in isolated strips from naive and CYP-8d
rats. Similarly, the isolated strips from naive rats exhibited lower sensitivity to GsMTx4 than those from CYP-8d rats (Fig. 3d–f). The vehicle (DMSO) had no significant influence on either
the urodynamic parameters or the spontaneous contractions in naive and CYP-8d rats. Based on these results, we speculated that the Piezo1 channel plays a more important role in regulating
bladder activity in CYP-induced chronic cystitis than under physiologic conditions. Because the Piezo1 channel was significantly increased in bladder ICC-LCs during cystitis but not in
detrusor smooth muscles, we attempted to further identify whether the effects of GsMTx4 on bladder activity were mediated through Piezo1 channel inhibition in bladder ICC-LCs. We utilized
the c-kit blocker Glivec to inhibit bladder ICC-LC function as previously reported4. We found that upon the application of Glivec (100 μM), the effects of GsMTx4 on the phasic amplitude of
spontaneous contractions in isolated strips from naive and CYP-8d rats were eliminated (Fig. 3g, h). Based on this result, we suggest that the Piezo1 channel may control bladder activity by
regulating bladder ICC-LC function. PIEZO1 CHANNEL ACTIVATION SIGNIFICANTLY ENHANCED THE [CA2+]I AND [NA+]I IN BLADDER ICC-LCS DURING CYP-INDUCED CHRONIC CYSTITIS To further explore the
mechanisms underlying the functional role of the Piezo1 channel in regulating bladder ICC-LC function, we focused on the two most important ions associated with cell excitation, Ca2+ and
Na+. Hypotonic stress was applied to bladder ICC-LCs to activate the Piezo1 channel. In bladder ICC-LCs from naive and CYP-8d rats, hypotonic stress significantly increased [Ca2+]i and
[Na+]i, and such increases in both the [Ca2+]i and [Na+]i were significantly weakened by GsMTx4 (2.5 μM) (Fig. 4a–d). We speculated that the reduction in [Ca2+]i and [Na+]i induced by GsMTx4
accounted for the Ca2+ and Na+ influx elicited by Piezo1 channel activation. Therefore, we concluded that the Ca2+ and Na+ influx induced by Piezo1 channel activation was significantly
enhanced in bladder ICC-LCs from CYP-8d rats compared with that in bladder ICC-LCs from naive rats, and the enhancement in Ca2+ influx was more remarkable (Fig. 4e, f). Moreover, upon
hypotonic stress application, [Ca2+]i continuously rose to a high level in bladder ICC-LCs from CYP-8d rats. However, [Na+]i stably increased followed by a rapid decrease (Fig. 4b, d). A
similar phenomenon was not detected in bladder ICC-LCs from naive rats. These data prompted us to consider that, in addition to the Piezo1 channel, [Ca2+]i and [Na+]i in bladder ICC-LCs may
be regulated by other factors during CYP-induced chronic cystitis. NA+/CA2+ EXCHANGER (NCX) EXPRESSION WAS SIGNIFICANTLY INCREASED AND THE REVERSE MODE OF NCX WAS RELATIVELY ACTIVATED IN
BLADDER ICC-LCS FROM CYP-8D RATS NCX is thought to be a key transporter in the regulation of cytosolic Ca2+ dynamics through its ability to transport three Na+ ions for every one Ca2+ ion.
NCX normally operates to maintain Ca2+ homeostasis by removing Ca2+ from the cells in the forward mode and bringing Ca2+ into the cells in the reverse mode33. To determine whether NCX is
involved in the control of Ca2+ dynamics in bladder ICC-LCs during CYP-induced chronic cystitis, we first examined changes in NCX subtype (NCX1-3) expression and function in CYP-8d rats. The
results showed that NCX1 and NCX3 mRNA and protein expression was significantly increased in CYP-48h and CYP-8d rat bladders compared with naive and CYP-4h rat bladders, and increases in
CYP-8d rat bladders were more significant. NCX2 mRNA and protein expression was only altered in CYP-8d rat bladders (Fig. 5a–c). Based on the fact that NCX1 protein expression was the most
dominant in whole rat bladders under both physiologic and pathologic conditions, we proposed that NCX1 may play a vital role in regulating bladder function. Hence, we subsequently identified
changes in NCX1 protein expression in bladder ICC-LCs using IF staining. We found that NCX1 protein expression in bladder ICC-LCs from CYP-8d rats was significantly higher than that in
ICC-LCs from naive rats (Fig. 5d). Furthermore, we conducted whole-cell patch-clamp experiments to record the NCX current (INCX) in isolated bladder ICC-LCs. As shown in Fig. 5e, the INCX
was recorded in bladder ICC-LCs from naive and CYP-8d rats. When normalized to cell capacitance, the absolute value of INCX density in bladder ICC-LCs from CYP-8d rats was significantly
enhanced compared with that in bladder ICC-LCs from naive rats over a voltage range of −100 to −80 mV (forward mode) and +10 to +60 mV (reverse mode). In bladder ICC-LCs from CYP-8d rats,
the absolute value of INCX density was enhanced (at −100 mV: naive: 38.82 ± 4.03 versus CYP-8d: 59.02 ± 6.36; at +60 mV: naive: 49.07 ± 2.77 versus CYP-8d: 80.93 ± 12.78) (Fig. 5f). We found
that the enhancement in the reverse mode of NCX was more significant, which indicated that the reverse mode of NCX was relatively activated in bladder ICC-LCs during CYP-induced chronic
cystitis. In addition, the results of single-cell RT-PCR following electrophysiological testing demonstrated that only amplified c-kit (235 bp) and GAPDH (181 bp) products were found in the
agarose gel lanes (Figure S2). According to this result, the authenticity of the isolated bladder ICC-LCs was confirmed. PIEZO1 CHANNEL FUNCTIONALLY INTERACTED WITH THE REVERSE MODE OF NCX1
IN BLADDER ICC-LCS FROM CYP-8D RATS To further examine the relationships between the Piezo1 channel and NCX1, we performed IF staining and a co-IP analysis. We found that the Piezo1 channel
was colocalized with NCX1 in cells located in the LP and detrusor region in naive and CYP-8d rat bladders (Fig. 6a). Moreover, the co-IP analysis results showed that the Piezo1 channel and
NCX1 interact with each other in CYP-8d rat bladders (Fig. 6b). Subsequently, we conducted contractility studies and patch-clamp experiments to test the functional interaction between the
Piezo1 channel and NCX1. After administration of the NCX reverse mode inhibitor KB-R7943 (10 μM), GsMTx4 no longer reduced the phasic amplitude of spontaneous contractions in isolated strips
from CYP-8d rats (Fig. 6c, d). Furthermore, we found that upon the application of hypotonic stress, the absolute value of the INCX density was significantly increased in bladder ICC-LCs
from CYP-8d rats (at −100 mV: 75.92 ± 7.30; at + 60 mV: 103.30 ± 9.66 versus that in Fig. 5f). GsMTx4 significantly decreased the absolute value of the INCX density (at −100 mV: 59.68 ±
11.06; at + 60 mV: 75.87 ± 15.19), whereas DMSO had no effects on INCX density (Fig. 6e). These results showed that compared with the forward mode of NCX, the reverse mode of NCX was more
significantly altered by Piezo1 channel activation or inhibition in bladder ICC-LCs from CYP-8d rats. Taken together, the results suggest that the Piezo1 channel functionally interacts with
the reverse mode of NCX, especially NCX1, in bladder ICC-LCs during CYP-induced chronic cystitis. SIRNA TARGETING THE PIEZO1 CHANNEL SIGNIFICANTLY REDUCED [CA2+]I AND[NA+]I AND THE INCX
DENSITY IN BLADDER ICC-LCS FROM CYP-8D RATS To more specifically identify the functional role of the Piezo1 channel in bladder ICC-LCs during CYP-induced chronic cystitis, we utilized siRNA
targeting rat Piezo1 (siPiezo1) to knockdown Piezo1 channel expression. Compared with negative control siRNA (ncPiezo1), siPiezo1 significantly decreased Piezo1 channel mRNA and protein
expression in bladder ICC-LCs (Fig. 7a, b). After Piezo1 channel knockdown using siPiezo1, [Ca2+]i and [Na+]i measurements and patch-clamp experiments were performed in bladder ICC-LCs.
Similar to GsMTx4, siPiezo1 attenuated the increases in [Ca2+]i and [Na+]i induced by hypotonic stress application in bladder ICC-LCs from naive and CYP-8d rats, and reductions caused by
siPiezo1 were more obvious in bladder ICC-LCs from CYP-8d rats (Fig. 7c–f). Hence, we confirmed again that Ca2+ and Na+ influx induced by Piezo1 channel activation was significantly stronger
in bladder ICC-LCs from CYP-8d rats than in bladder ICC-LCs from naive rats. In addition, siPiezo1 significantly reduced the absolute value of the INCX density that was recorded under
hypotonic conditions in bladder ICC-LCs from CYP-8d rats (at −100 mV: ncPiezo1: 75.04 ± 7.54 versus siPiezo1: 61.12 ± 8.44; at + 60 mV: ncPiezo1: 103.16 ± 8.92 versus siPiezo1: 78.42 ± 6.88)
(Fig. 7g, h). We also found that the siPiezo1-induced decrease in the reverse mode of NCX was more significant than that in the forward mode of NCX. Taken together, the results suggested
that during CYP-induced chronic cystitis, the significantly upregulated Piezo1 channel in bladder ICC-LCs can be activated by mechanical stimulus (including stretch and hypotonic stress) and
subsequently facilitate robust Ca2+ and Na+ influx into bladder ICC-LCs. Meanwhile, the Piezo1 channel functionally interacted with the reverse mode of NCX1 that was relatively activated in
bladder ICC-LCs during CYP-induced chronic cystitis. As a consequence, three cytosolic Na+ ions that permeated the membrane via the Piezo1 channel were transported out of cells in exchange
for one Ca2+ ion brought into the cytoplasm through the reverse mode of NCX1 in bladder ICC-LCs. The synergistic effects of the Piezo1 channel and NCX1 significantly increased [Ca2+]i and
led to Ca2+ overload in bladder ICC-LCs, which may consequently induce ICC-LC hyperactivity and chronic cystitis-associated hyperactive bladder (Fig. 8). DISCUSSION In the present study, we
demonstrated that increased Piezo1 channel activity in bladder ICC-LCs plays a crucial role in chronic cystitis-associated bladder hyperactivity by regulating bladder ICC-LC function. The
potential mechanism in CYP-induced chronic cystitis involves hypotonic stress-induced Piezo1 channel activation that significantly elicits robust Ca2+ and Na+ influx into bladder ICC-LCs,
and the Piezo1 channel functionally interacts with the relatively activated NCX1 reverse mode, which significantly enhances the intracellular Ca2+ concentration and leads to Ca2+ overload in
bladder ICC-LCs. A previous study reported that Piezo1 mRNA and protein expression was significantly increased only in the suburothelial and detrusor layers in rats after PBOO22. In the
current study, we also demonstrated that Piezo1 protein expression was significantly enhanced in the suburothelial layers (LP) during chronic cystitis. However, in the detrusor region, we
found that Piezo1 protein expression was significantly increased in interstitial cells located in the intermuscular region but not in detrusor smooth muscle cells. Meanwhile, we observed
that the Piezo1 channel was significantly overexpressed in the urothelial layer during chronic cystitis. We speculated that such conformity and discrepancy may be ascribed to the complicated
regulatory mechanisms of Piezo1 channel expression in diverse pathologic states in various experimental models. Further research is needed to clarify the exact mechanism underlying this
phenomenon. Furthermore, we verified that Piezo1 channel expression was significantly increased in bladder ICC-LCs located in the LP and intermuscular region. This finding prompted us to
consider that the Piezo1 channel may participate in chronic cystitis-associated bladder dysfunction by regulating ICC-LC activity. McCloskey and Gurney suggested that bladder ICC-LCs could
act as pacemakers to regulate spontaneous detrusor contraction or as intermediaries in the transmission of nerve signals to detrusor smooth muscle cells34. Bladder ICC-LCs express the
proto-oncogene c-kit, which not only is an identification marker of these cells but also plays a critical role in the control of bladder function35. Several studies have reported that
selective inhibition of c-kit by imatinib mesylate (Glivec) significantly reduces bladder activity via the c-kit receptor in bladder ICC-LCs in some bladder disorders, including overactive
bladder, diabetic cystopathy, and neurogenic bladder5, 7, 36. c-kit mutation in bladder ICC-LCs is also associated with certain voiding dysfunctions6. Based on the functional importance of
ICC-LCs with respect to the regulation of bladder function indicated by the above results, although significantly increased Piezo1 channel expression was detected in both the bladder ICC-LCs
and the urothelial layer during chronic cystitis, we mainly focused our attention on the functional role of the Piezo1 channel in bladder ICC-LCs. As expected, we subsequently confirmed
that the Piezo1 channel blocker GsMTx4 significantly attenuated chronic cystitis-associated bladder hyperactivity by inhibiting the Piezo1 channel in bladder ICC-LCs. Bladder ICC-LCs possess
the ability to generate spontaneous Ca2+ signaling and fire Ca2+ waves in response to cholinergic and purinergic stimuli, which is their functional underpinning for controlling bladder
activity9. Moreover, it has been shown that Ca2+ signaling in bladder ICC-LCs is upregulated or downregulated in bladder dysfunction associated with suprasacral or sacral spinal cord injury,
respectively36. In our previous research, we demonstrated that bladder ICC-LC hyperactivity accounted for bladder hyperactivity in CYP-induced chronic cystitis, which was characterized by
excessive Ca2+ entry into cells upon carbachol application12. Furthermore, Ca2+ overload in cardiomyocytes is closely related to cardiac dysfunction37, 38. Thus, we suggest that abnormal
Ca2+ signaling in bladder ICC-LCs may be involved in the pathogenesis of bladder dysfunction. To the best of our knowledge, the mechanosensitive Piezo1 cation channel may utilize its
peripheral domains as force sensors to gate the central ion-conducting pore14 and is permeated by a series of ions, including Ca2+, Mg2+, K+, and Na+39. In the current study, we found that
Piezo1 channel activation induced by hypotonic stress significantly provoked Ca2+ influx in bladder ICC-LCs in CYP-induced chronic cystitis. Hence, we speculate that the Piezo1 channel is
susceptible to being activated during bladder filling or by cellular swelling under cystitis conditions, and Piezo1 channel activation can facilitate robust Ca2+ influx and lead to Ca2+
overload in bladder ICC-LCs during chronic cystitis, which may be an important etiological factor for bladder ICC-LC hyperactivity and the consequent chronic cystitis-associated bladder
hyperactivity. Piezo1 channel activation also significantly provoked Na+ influx into bladder ICC-LCs, but the elevated intracellular Na+ concentration was subsequently mediated. We
speculated that NCX may be involved in this process. NCX plays a central role in cellular Ca2+ homeostasis by removing Ca2+ through its forward mode under physiological conditions33.
However, augmented Ca2+ entry through reverse NCX activity is responsible for arrhythmia associated with heart failure or ischemia/reperfusion injury40. Furthermore, the accelerated Ca2+
influx (reverse) mode of NCX in smooth muscle can lead to an overactive bladder41. Consistently, we also observed that the reverse mode of NCX was relatively activated in bladder ICC-LCs
during chronic cystitis. Using GsMTx4 or siRNA targeting Piezo1, we confirmed that the Piezo1 channel functionally interacted with the reverse mode of NCX. Through these functional
interactions, Na+ introduced by the Piezo1 channel will be extracted from the cells via reverse NCX activity, especially that of NCX1, which can aggravate Ca2+ overload in bladder ICC-LCs.
In addition, the Piezo1 channel was found to be colocalized with NCX1 in cells located in the LP and detrusor region. Based on the finding that the Piezo1 channel and NCX1 were both
expressed in bladder ICC-LCs, we speculated that the Piezo1 channel was colocalized with NCX1 in bladder ICC-LCs. Moreover, we found that the Piezo1 channel bound to NCX1. These
relationships between the Piezo1 channel and NCX1 can provide the structural foundation for their functional interaction in bladder ICC-LCs. In the present study, we examined the functional
role of the Piezo1 channel in bladder ICC-LCs in CYP-induced chronic cystitis, and the results will serve as a potent supplement to clarify the comprehensive mechanisms underlying the
control of bladder activity by the Piezo1 channel under pathologic conditions. However, a limitation of our study is that we did not test the functional effects of the Piezo2 channel on
bladder function regulation. Additional research is required to elucidate the functional role of the Piezo2 channel in regulating bladder activity. Furthermore, it is commonly known that the
sarcoplasmic reticulum (SR) plays an important role in regulation of cytosolic Ca2+ dynamics42, and further studies are needed to explore the functional relationship between the Piezo1
channel and SR in CYP-induced chronic cystitis or other bladder disorders. In summary, our study reveals an important interplay among Piezo1 and the NCX1 channel in CYP-induced chronic
cystitis. The synergistic effects of the Piezo1 channel and NCX1 significantly increased the intracellular Ca2+ concentration and led to Ca2+ overload in bladder ICC-LCs, which are essential
for chronic cystitis-associated bladder hyperactivity. These findings indicate the functional importance of the Piezo1 channel and NCX1 in bladder ICC-LCs during CYP-induced chronic
cystitis, as well as their potential as therapeutic targets for chronic cystitis-associated bladder hyperactivity. REFERENCES * de Oliveira, M. G. et al. Activation of soluble guanylyl
cyclase by BAY 58-2667 improves bladder function in cyclophosphamide-induced cystitis in mice. _Am. J. Physiol. Ren. Physiol._ 311, F85–F93 (2016). Google Scholar * Lv, J. W. et al.
Inhibition of microRNA-214 promotes epithelial-mesenchymal transition process and induces interstitial cystitis in postmenopausal women by upregulating Mfn2. _Exp. Mol. Med._ 49, e357
(2017). PubMed PubMed Central Google Scholar * Neuhaus, J. & Schwalenberg, T. Intravesical treatments of bladder pain syndrome/interstitial cystitis. _Nat. Rev. Urol._ 9, 707–720
(2012). CAS PubMed Google Scholar * Kubota, Y., Biers, S. M., Kohri, K. & Brading, A. F. Effects of imatinib mesylate (Glivec) as a c-kit tyrosine kinase inhibitor in the guinea-pig
urinary bladder. _Neurourol. Urodyn._ 25, 205–210 (2006). CAS PubMed Google Scholar * Biers, S. M., Reynard, J. M., Doore, T. & Brading, A. F. The functional effects of a c-kit
tyrosine inhibitor on guinea-pig and human detrusor. _BJU Int._ 97, 612–616 (2006). CAS PubMed Google Scholar * Okada, S. et al. Attenuation of bladder overactivity in KIT mutant rats.
_BJU Int._ 108, E97–E103 (2011). PubMed Google Scholar * Vahabi, B., McKay, N. G., Lawson, K. & Sellers, D. J. The role of c-kit-positive interstitial cells in mediating phasic
contractions of bladder strips from streptozotocin-induced diabetic rats. _BJU Int._ 107, 1480–1487 (2011). CAS PubMed Google Scholar * Juszczak, K., Maciukiewicz, P., Drewa, T. &
Thor, P. J. Cajal-like interstitial cells as a novel target in detrusor overactivity treatment: true or myth? _Cent. Eur. J. Urol._ 66, 413–417 (2014). Google Scholar * McCloskey, K. D.
Interstitial cells in the urinary bladder–localization and function. _Neurourol. Urodyn._ 29, 82–87 (2010). PubMed Google Scholar * Gevaert, T. et al. Identification of different
phenotypes of interstitial cells in the upper and deep lamina propria of the human bladder dome. _J. Urol._ 192, 1555–1563 (2014). PubMed Google Scholar * McCloskey, K. D. Bladder
interstitial cells: an updated review of current knowledge. _Acta Physiol. (Oxf.)._ 207, 7–15 (2013). CAS PubMed Google Scholar * Liu, Q. et al. Cyclophosphamide-induced HCN1 channel
upregulation in interstitial Cajal-like cells leads to bladder hyperactivity in mice. _Exp. Mol. Med._ 49, e319 (2017). CAS PubMed PubMed Central Google Scholar * Coste, B. et al. Piezo1
and Piezo2 are essential components of distinct mechanically activated cation channels. _Science_ 330, 55–60 (2010). CAS PubMed PubMed Central Google Scholar * Ge, J. et al.
Architecture of the mammalian mechanosensitive Piezo1 channel. _Nature_ 527, 64–69 (2015). CAS PubMed Google Scholar * Wang, S. et al. Endothelial cation channel PIEZO1 controls blood
pressure by mediating flow-induced ATP release. _J. Clin. Invest._ 126, 4527–4536 (2016). PubMed PubMed Central Google Scholar * Gudipaty, S. A. et al. Mechanical stretch triggers rapid
epithelial cell division through Piezo1. _Nature_ 543, 118–121 (2017). CAS PubMed PubMed Central Google Scholar * Albuisson, J. et al. Dehydrated hereditary stomatocytosis linked to
gain-of-function mutations in mechanically activated PIEZO1 ion channels. _Nat. Commun._ 4, 1884 (2013). PubMed PubMed Central Google Scholar * Glogowska, E. et al. Novel mechanisms of
PIEZO1 dysfunction in hereditary xerocytosis. _Blood_ 130, 1845–1856 (2017). CAS PubMed PubMed Central Google Scholar * Fotiou, E. et al. Novel mutations in PIEZO1 cause an autosomal
recessive generalized lymphatic dysplasia with non-immune hydrops fetalis. _Nat. Commun._ 6, 8085 (2015). PubMed PubMed Central Google Scholar * Liang, J. et al. Stretch-activated channel
Piezo1 is up-regulated in failure heart and cardiomyocyte stimulated by AngII. _Am. J. Transl. Res._ 9, 2945–2955 (2017). CAS PubMed PubMed Central Google Scholar * Miyamoto, T. et al.
Functional role for Piezo1 in stretch-evoked Ca(2)(+) influx and ATP release in urothelial cell cultures. _J. Biol. Chem._ 289, 16565–16575 (2014). CAS PubMed PubMed Central Google
Scholar * Michishita, M., Yano, K., Tomita, K. I., Matsuzaki, O. & Kasahara, K. I. Piezo1 expression increases in rat bladder after partial bladder outlet obstruction. _Life. Sci._ 166,
1–7 (2016). CAS PubMed Google Scholar * Lee, G., Romih, R. & Zupancic, D. Cystitis: from urothelial cell biology to clinical applications. _Biomed. Res. Int._ 2014, 473536 (2014).
PubMed PubMed Central Google Scholar * Tyagi, P., Hsieh, V. C., Yoshimura, N., Kaufman, J. & Chancellor, M. B. Instillation of liposomes vs dimethyl sulphoxide or pentosan
polysulphate for reducing bladder hyperactivity. _BJU Int._ 104, 1689–1692 (2009). CAS PubMed Google Scholar * Charrua, A. et al. Co-administration of transient receptor potential
vanilloid 4 (TRPV4) and TRPV1 antagonists potentiate the effect of each drug in a rat model of cystitis. _BJU Int._ 115, 452–460 (2015). CAS PubMed Google Scholar * Zhang, L. et al. An
immunogenic peptide, T2 induces interstitial cystitis/painful bladder syndrome: an autoimmune mouse model for interstitial cystitis/painful bladder syndrome. _Inflammation_ 40, 2033–2041
(2017). CAS PubMed Google Scholar * Coelho, A. et al. Urinary bladder inflammation induces changes in urothelial nerve growth factor and TRPV1 channels. _Br. J. Pharmacol._ 172, 1691–1699
(2015). CAS PubMed PubMed Central Google Scholar * Takahara, Y. et al. Expression of pancreatitis associated proteins in urothelium and urinary afferent neurons following
cyclophosphamide induced cystitis. _J. Urol._ 179, 1603–1609 (2008). CAS PubMed Google Scholar * Zhang, Q. H., Zhou, Z. S., Lu, G. S., Song, B. & Guo, J. X. Melatonin improves bladder
symptoms and may ameliorate bladder damage via increasing HO-1 in rats. _Inflammation_ 36, 651–657 (2013). CAS PubMed Google Scholar * Fischer, A. H., Jacobson, K. A., Rose, J. &
Zeller, R. Hematoxylin and eosin staining of tissue and cell sections. _CSH Protoc._ 2008, pdb.prot4986 (2008). PubMed Google Scholar * Tu, H. et al. Serotonin (5-HT)2A/2C receptor agonist
(2,5-dimethoxy-4-idophenyl)-2-aminopropane hydrochloride (DOI) improves voiding efficiency in the diabetic rat. _BJU Int._ 116, 147–155 (2015). CAS PubMed Google Scholar * Soya, M. et
al. Plasma membrane stretch activates transient receptor potential vanilloid and ankyrin channels in Merkel cells from hamster buccal mucosa. _Cell Calcium_ 55, 208–218 (2014). CAS PubMed
Google Scholar * Ander, B. P. et al. Differential sensitivities of the NCX1.1 and NCX1.3 isoforms of the Na+ -Ca2+ exchanger to alpha-linolenic acid. _Cardiovasc. Res._ 73, 395–403 (2007).
CAS PubMed Google Scholar * McCloskey, K. D. & Gurney, A. M. Kit positive cells in the guinea pig bladder. _J. Urol._ 168, 832–836 (2002). PubMed Google Scholar * Kubota, Y. et al.
Role of KIT-positive interstitial cells of Cajal in the urinary bladder and possible therapeutic target for overactive bladder. _Adv. Urol._ 2011, 816342 (2011). PubMed PubMed Central
Google Scholar * Deng, J. et al. The effects of Glivec on the urinary bladder excitation of rats with suprasacral or sacral spinal cord transection. _J. Surg. Res._ 183, 598–605 (2013). CAS
PubMed Google Scholar * Kojima, A., Kitagawa, H., Omatsu-Kanbe, M., Matsuura, H. & Nosaka, S. Sevoflurane protects ventricular myocytes against oxidative stress-induced cellular Ca2+
overload and hypercontracture. _Anesthesiology_ 119, 606–620 (2013). CAS PubMed Google Scholar * Zhao, Y. et al. Shensong Yangxin capsules prevent ischemic arrhythmias by prolonging
action potentials and alleviating Ca2+ overload. _Mol. Med. Rep._ 13, 5185–5192 (2016). CAS PubMed Google Scholar * Gnanasambandam, R., Bae, C., Gottlieb, P. A. & Sachs, F. Ionic
selectivity and permeation properties of human PIEZO1 channels. _PLoS. ONE._ 10, e0125503 (2015). PubMed PubMed Central Google Scholar * Nagy, N. et al. Selective Na(+) /Ca(2+) exchanger
inhibition prevents Ca(2+) overload-induced triggered arrhythmias. _Br. J. Pharmacol._ 171, 5665–5681 (2014). CAS PubMed PubMed Central Google Scholar * Yamamura, H. et al. Overactive
bladder mediated by accelerated Ca2 + influx mode of Na + /Ca2 + exchanger in smooth muscle. _Am. J. Physiol. Cell. Physiol._ 305, C299–C308 (2013). CAS PubMed Google Scholar * Zhang, H.
et al. STIM1-Ca2 + signaling modulates automaticity of the mouse sinoatrial node. _Proc. Natl. Acad. Sci. USA_ 112, E5618–E5627 (2015). CAS PubMed Google Scholar Download references
ACKNOWLEDGEMENTS This work was supported by the National Natural Science Foundation of China (nos. 81770761 and 81500580). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of
Urology, Second Affiliated Hospital, Third Military Medical University, Chongqing, 400037, China Qian Liu, Bishao Sun, Jiang Zhao, Qingqing Wang, Xiaoyan Hu, Zhenxing Yang, Jie Xu &
Longkun Li * Cancer Center, Institute of Cancer Stem Cell, Dalian Medical University, Dalian, 116044, China Fan An * Division of Radiation and Cancer Biology, Department of Radiation
Oncology, University of Michigan, Ann Arbor, MI, 48105, USA Mingjia Tan Authors * Qian Liu View author publications You can also search for this author inPubMed Google Scholar * Bishao Sun
View author publications You can also search for this author inPubMed Google Scholar * Jiang Zhao View author publications You can also search for this author inPubMed Google Scholar *
Qingqing Wang View author publications You can also search for this author inPubMed Google Scholar * Fan An View author publications You can also search for this author inPubMed Google
Scholar * Xiaoyan Hu View author publications You can also search for this author inPubMed Google Scholar * Zhenxing Yang View author publications You can also search for this author
inPubMed Google Scholar * Jie Xu View author publications You can also search for this author inPubMed Google Scholar * Mingjia Tan View author publications You can also search for this
author inPubMed Google Scholar * Longkun Li View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Q.L. performed the major experiments and
drafted the manuscript. J.X. and Z.Y. analyzed the data. B.S. and J.Z. were involved in the H&E staining, western blotting, quantitative PCR, and immunostaining. Q.W. and X.H.
participated in the urodynamic measurements, contractility studies, [Ca2+]i and [Na+]i measurements, and patch-clamp experiments. F.A. drew the schematic representation. L.L. and M.T.
designed the study and edited the paper. All authors reviewed and approved the submission of the paper. CORRESPONDING AUTHORS Correspondence to Mingjia Tan or Longkun Li. ETHICS DECLARATIONS
CONFLICT OF INTEREST The authors declare that they have no conflict of interest. ADDITIONAL INFORMATION PUBLISHER’S NOTE: Springer Nature remains neutral with regard to jurisdictional
claims in published maps and institutional affiliations. ELECTRONIC SUPPLEMENTARY MATERIAL SUPPLEMENTARY TABLE SUPPLEMENTARY FIGURES SUPPLEMENTARY INFORMATION RIGHTS AND PERMISSIONS OPEN
ACCESS This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and
reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, and provide a link to the Creative Commons license. You do not have
permission under this license to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s
Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not
permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license,
http://creativecommons.org/licenses/by-nc-nd/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Liu, Q., Sun, B., Zhao, J. _et al._ Increased Piezo1 channel activity in
interstitial Cajal-like cells induces bladder hyperactivity by functionally interacting with NCX1 in rats with cyclophosphamide-induced cystitis. _Exp Mol Med_ 50, 1–16 (2018).
https://doi.org/10.1038/s12276-018-0088-z Download citation * Received: 21 November 2017 * Revised: 31 January 2018 * Accepted: 14 February 2018 * Published: 07 May 2018 * Issue Date: May
2018 * DOI: https://doi.org/10.1038/s12276-018-0088-z SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable
link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
