Blocking of oestrogen signals improves anti-tumour effect regardless of oestrogen receptor alpha expression in cancer cells
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

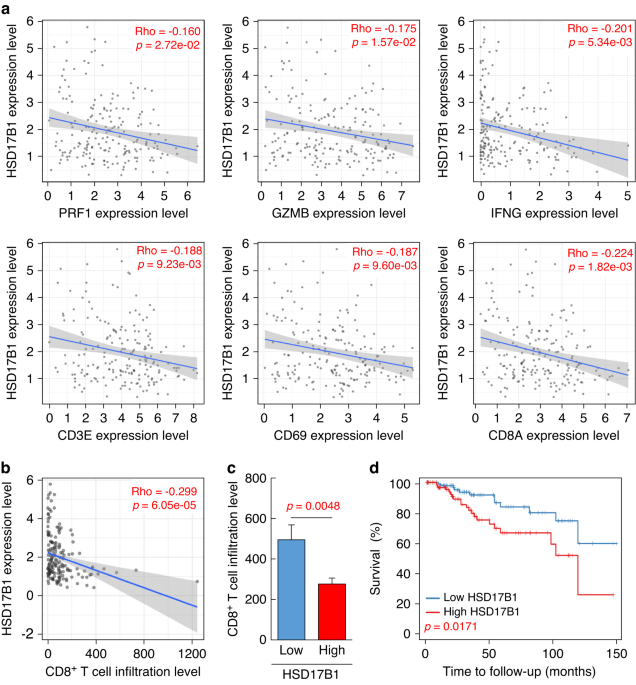
ABSTRACT BACKGROUND Anti-oestrogenic therapy has been used for breast cancer patients with oestrogen susceptibility cancer cells. However, little has been known about its potential role for
immune cell biology within TME, particularly in cancer patients without oestrogen sensitivity of tumour cells. Therefore, we aimed to study the effect of oestrogen on immunity within TME.
METHODS Using a clinical dataset, immune cells of humans and mice, female mice with and without ovaries, and several murine ERα-negative cancer cell lines, we evaluated the effect of
oestrogen on immunity in TME. RESULTS Clinical data analysis suggested oestrogen’s suppressive efficacy against CTLs. Additionally, in vitro and in vivo experiments revealed intra-tumoural
CTLs’ direct repressive action by oestrogen in both mice and humans; blockade of oestrogen signals cancelled its immunosuppression resulting in tumour growth reduction in vivo. Most notably,
immunotherapy (immune checkpoint inhibitor; ICI) combined with anti-oestrogenic therapy exhibited a dramatic anti-tumour effect. CONCLUSIONS This study provides novel insights into how
oestrogen contributes to tumour progression and a therapeutic rationale for blocking oestrogen signalling to boost the anti-tumour effect of ICI, regardless of tumour cells’ ERα expression.
Access through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Subscribe to this
journal Receive 24 print issues and online access $259.00 per year only $10.79 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now
Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer
support SIMILAR CONTENT BEING VIEWED BY OTHERS IMMUNE LANDSCAPE OF BREAST TUMORS WITH LOW AND INTERMEDIATE ESTROGEN RECEPTOR EXPRESSION Article Open access 13 May 2023 INHIBITION OF RANK
SIGNALING IN BREAST CANCER INDUCES AN ANTI-TUMOR IMMUNE RESPONSE ORCHESTRATED BY CD8+ T CELLS Article Open access 10 December 2020 MOLECULAR CORRELATES OF RESPONSE TO ERIBULIN AND
PEMBROLIZUMAB IN HORMONE RECEPTOR-POSITIVE METASTATIC BREAST CANCER Article Open access 21 September 2021 DATA AVAILABILITY Data are available on reasonable request. The datasets used and/or
analysed during the current study are available from the corresponding author. REFERENCES * Chen C, Gong X, Yang X, Shang X, Du Q, Liao Q, et al. The roles of estrogen and estrogen
receptors in gastrointestinal disease (Review). Oncol Lett. 2019;18:5673–80. CAS PubMed PubMed Central Google Scholar * Tohyama S, Ogino Y, Lange A, Myosho T, Kobayashi T, Hirano Y, et
al. Establishment of estrogen receptor 1 (ESR1)-knockout medaka: ESR1 is dispensable for sexual development and reproduction in medaka, _Oryzias latipes_. Dev Growth Differ. 2017;59:552–61.
Article CAS PubMed Google Scholar * Gompel A. Hormone and breast cancer. Presse Medicale. 2019;48:1085–91. Article PubMed Google Scholar * Lin CY, Ström A, Vega VB, Kong SL, Yeo AL,
Thomsen JS, et al. Discovery of estrogen receptor alpha target genes and response elements in breast tumor cells. Genome Biol. 2004;5:R66. * Cunningham M, Gilkeson G. Estrogen receptors in
immunity and autoimmunity. Clin Rev Allergy Immunol. 2011;40:66–73. Article CAS PubMed Google Scholar * Wang T, Jin J, Qian C, Lou J, Lin J, Xu A, et al. Estrogen/ER in anti-tumor
immunity regulation to tumor cell and tumor microenvironment. Cancer Cell Int. 2021;21:1–13. Google Scholar * Chuffa LGdA, Lupi-Júnior LA, Costa AB, Amorim JPdA, Seiva FR. The role of sex
hormones and steroid receptors on female reproductive cancers. Steroids. 2017;118:93–108. Article CAS PubMed Google Scholar * Hsieh CC, Trichopoulos D, Katsouyanni K, Yuasa S. Age at
menarche, age at menopause, height and obesity as risk factors for breast cancer: Associations and interactions in an international case‐control study. Int J Cancer. 1990;46:796–800. Article
CAS PubMed Google Scholar * Zattarin E, Leporati R, Ligorio F, Lobefaro R, Vingiani A, Pruneri G, et al. Hormone receptor loss in breast cancer: molecular mechanisms, clinical settings,
and therapeutic implications. Cells. 2020;9:2644. Article CAS PubMed PubMed Central Google Scholar * Morgan DAL, Refalo NA, Cheung KL. Strength of ER-positivity in relation to survival
in ER-positive breast cancer treated by adjuvant tamoxifen as sole systemic therapy. Breast. 2011;20:215–9. Article PubMed Google Scholar * Braun L, Mietzsch F, Seibold P, Schneeweiss A,
Schirmacher P, Chang-Claude J, et al. Intrinsic breast cancer subtypes defined by estrogen receptor signalling-prognostic relevance of progesterone receptor loss. Mod Pathol.
2013;26:1161–71. Article CAS PubMed Google Scholar * Backes FJ, Walker CJ, Goodfellow PJ, Hade EM, Agarwal G, Mutch D, et al. Estrogen receptor-alpha as a predictive biomarker in
endometrioid endometrial cancer. Gynecol Oncol. 2016;141:312–7. Article CAS PubMed PubMed Central Google Scholar * Deepak KGK, Vempati R, Nagaraju GP, Dasari VR, Nagini S, Rao DN, et
al. Tumor microenvironment: challenges and opportunities in targeting metastasis of triple negative breast cancer. Pharmacol Res. 2020;153:104683. Article CAS PubMed Google Scholar *
Kajihara N, Kobayashi T, Otsuka R, Nio J, Tomohiro K. Tumor - derived interleukin-34 creates an immunosuppressive and chemoresistant tumor microenvironment by modulating myeloid-derived
suppressor cells in triple-negative breast cancer. Cancer Immunol Immunother. 2023;72:851–64. Article CAS PubMed Google Scholar * Hangai S, Kawamura T, Kimura Y, Chang CY, Hibino S,
Yamamoto D, et al. Orchestration of myeloid-derived suppressor cells in the tumor microenvironment by ubiquitous cellular protein TCTP released by tumor cells. Nat Immunol. 2021;22:947–57.
Article CAS PubMed Google Scholar * Márquez-Garbán DC, Deng G, Comin-Anduix B, Garcia AJ, Xing Y, Chen HW, et al. Antiestrogens in combination with immune checkpoint inhibitors in breast
cancer immunotherapy. J Steroid Biochem Mol Biol. 2019;193:105415. Article PubMed PubMed Central Google Scholar * Chakraborty B, Byemerwa J, Shepherd J, Haines CN, Baldi R, Gong W, et
al. Inhibition of estrogen signaling in myeloid cells increases tumor immunity in melanoma. J Clin Investig. 2021;131:1–16. Article Google Scholar * Salem ML. Estrogen, a double-edged
sword: modulation of TH1- and TH2-mediated inflammations by differential regulation of TH1/TH2 cytokine production. Curr Drug Targets Inflamm Allergy. 2004;3:97–104. Article CAS PubMed
Google Scholar * Nakamura N, Miyazaki K, Kitano Y, Fujisaki S, Okamura H. Suppression of cytotoxic T-lymphocyte activity during human pregnancy. J Reprod Immunol. 1993;23:119–30. Article
CAS PubMed Google Scholar * Haghmorad D, Amini AA, Mahmoudi MB, Rastin M, Hosseini M, Mahmoudi M. Pregnancy level of estrogen attenuates experimental autoimmune encephalomyelitis in both
ovariectomized and pregnant C57BL/6 mice through expansion of Treg and Th2 cells. J Neuroimmunol. 2014;277:85–95. Article CAS PubMed Google Scholar * Conforti F, Pala L, Bagnardi V, De
Pas T, Martinetti M, Viale G, et al. Cancer immunotherapy efficacy and patients’ sex: a systematic review and meta-analysis. Lancet Oncol. 2018;19:737–46. Article CAS PubMed Google
Scholar * Svoronos N, Perales-Puchalt A, Allegrezza MJ, Rutkowski MR, Payne KK, Tesone AJ, et al. Tumor cell–independent estrogen signaling drives disease progression through mobilization
of myeloid-derived suppressor cells. Cancer Discov. 2017;7:72–85. Article CAS PubMed Google Scholar * Grumbach MM, Auchus RJ. Estrogen: consequences and implications of human mutations
in synthesis and action. J Clin Endocrinol Metab. 1999;84:4677–94. CAS PubMed Google Scholar * Wu AH, Seow A, Arakawa K, Van Den Berg D, Lee HP, Yu MC. HSD17B1 and CYP17 polymorphisms and
breast cancer risk among Chinese women in Singapore. Int J Cancer. 2003;104:450–7. Article CAS PubMed Google Scholar * Setiawan VW, Hankinson SE, Colditz GA, Hunter DJ, De Vivo I.
HSD17B1 gene polymorphisms and risk of endometrial and breast cancer. Cancer Epidemiol Biomarkers Prev. 2004;13:213–9. Article CAS PubMed Google Scholar * Treeck O, Schüler-Toprak S,
Ortmann O. Estrogen actions in triple-negative breast cancer. Cells. 2020;9:2358. * Howell SJ, Johnston SRD, Howell A. The use of selective estrogen receptor modulators and selective
estrogen receptor down-regulators in breast cancer. Best Pract Res Clin Endocrinol Metab. 2004;18:47–66. Article CAS PubMed Google Scholar * Tang H, Liao Y, Zhang C, Chen G, Xu L, Liu Z,
et al. Fulvestrant-mediated inhibition of estrogen receptor signaling slows lung cancer progression. Oncol Res. 2014;22:13–20. Article PubMed PubMed Central Google Scholar * Mishra AK,
Abrahamsson A, Dabrosin C. Fulvestrant inhibits growth of triple negative breast cancer and synergizes with tamoxifen in ERα positive breast cancer by up-regulation of ERβ. Oncotarget.
2016;7:56876–88. Article PubMed PubMed Central Google Scholar * Lumachi F, Brunello A, Maruzzo M, Basso U, Basso S. Treatment of estrogen receptor-positive breast cancer. Curr Med Chem.
2013;20:596–604. Article CAS PubMed Google Scholar * Ross SH, Cantrell DA. Signaling and function of interleukin-2 in T lymphocytes. Annu Rev Immunol. 2018;36:411–33. Article CAS
PubMed PubMed Central Google Scholar * Feau S, Arens R, Togher S, Schoenberger SP. Autocrine IL-2 is required for secondary population expansion of CD8 + memory T cells. Nat Immunol.
2011;12:908–13. Article CAS PubMed PubMed Central Google Scholar * Dai Z, Konieczny BT, Lakkis FG. The dual role of IL-2 in the generation and maintenance of CD8 + memory T cells. J
Immunol. 2000;165:3031–6. Article CAS PubMed Google Scholar * Johnston JA, Bacon CM, Finbloom DS, Rees RC, Kaplan D, Shibuya K, et al. Tyrosine phosphorylation and activation of STAT5,
STAT3, and Janus kinases by interleukins 2 and 15. Proc Natl Acad Sci USA. 1995;92:8705–9. Article CAS PubMed PubMed Central Google Scholar * Kajihara N, Kitagawa F, Kobayashi T, Wada
H, Otsuka R, Seino KI. Interleukin-34 contributes to poor prognosis in triple-negative breast cancer. Breast Cancer. 2020;27:1198–204. Article PubMed Google Scholar * Balkwill FR, Capasso
M, Hagemann T. The tumor microenvironment at a glance. J Cell Sci. 2012;125:5591–6. Article CAS PubMed Google Scholar * Liu R, Yang F, Yin JY, Liu YZ, Zhang W, Zhou HH. Influence of
tumor immune infiltration on immune checkpoint inhibitor therapeutic efficacy: a computational retrospective study. Front Immunol. 2021;12:1–15. Google Scholar * Chapman PB, Jayaprakasam
VS, Panageas KS, Callahan M, Postow MA, Shoushtari AN, et al. Risks and benefits of reinduction ipilimumab/nivolumab in melanoma patients previously treated with ipilimumab/nivolumab. J
Immunother Cancer. 2021;9:1–6. Article Google Scholar * Kagihara JA, Andress M, Diamond JR. Nab-paclitaxel and atezolizumab for the treatment of PD-L1-positive, metastatic triple-negative
breast cancer: review and future directions. Expert Rev Precis Med Drug Dev. 2020;5:59–65. Article PubMed PubMed Central Google Scholar * Zhao X, Subramanian S. Intrinsic resistance of
solid tumors to immune checkpoint blockade therapy. Cancer Res. 2017;77:817–22. Article CAS PubMed Google Scholar * Tie Y, Tang F, Wei YQ, Wei XW. Immunosuppressive cells in cancer:
mechanisms and potential therapeutic targets. J Hematol Oncol. 2022;15:61. Article CAS PubMed PubMed Central Google Scholar * Guan X, Polesso F, Wang C, Sehrawat A, Hawkins RM, Murray
SE, et al. Androgen receptor activity in T cells limits checkpoint blockade efficacy. Nature. 2022;606:791–6. Article CAS PubMed PubMed Central Google Scholar * Hama N, Kobayashi T, Han
N, Kitagawa F, Kajihara N, Otsuka R, et al. Interleukin-34 limits the therapeutic effects of immune checkpoint blockade. iScience. 2020;23:101584. Article CAS PubMed PubMed Central
Google Scholar * Sade-Feldman M, Yizhak K, Bjorgaard SL, Ray JP, de Boer CG, Jenkins RW, et al. Defining T cell states associated with response to checkpoint immunotherapy in melanoma.
Cell. 2018;175:998.e20–1013.e20. Article Google Scholar * Boyman O, Sprent J. The role of interleukin-2 during homeostasis and activation of the immune system. Nat Rev Immunol.
2012;12:180–90. Article CAS PubMed Google Scholar * Mitchell DM, Ravkov EV, Williams MA. Distinct roles for IL-2 and IL-15 in the differentiation and survival of CD8+ effector and memory
T cells. J Immunol. 2010;184:6719–30. Article CAS PubMed Google Scholar * Cho JH, Boyman O, Kim HO, Hahm B, Rubinstein MP, Ramsey C, et al. An intense form of homeostatic proliferation
of naive CD8+ cells driven by IL-2. J Exp Med. 2007;204:1787–801. Article CAS PubMed PubMed Central Google Scholar * Sun Z, Ren Z, Yang K, Liu Z, Cao S, Deng S, et al. A next-generation
tumor-targeting IL-2 preferentially promotes tumor-infiltrating CD8 + T-cell response and effective tumor control. Nat Commun. 2019;10:3874. Article CAS PubMed PubMed Central Google
Scholar * Kovats S. Estrogen receptors regulate innate immune cells and signaling pathways. Cell Immunol. 2015;294:63–9. Article CAS PubMed PubMed Central Google Scholar * Phiel KL,
Henderson RA, Adelman SJ, Elloso MM. Differential estrogen receptor gene expression in human peripheral blood mononuclear cell populations. Immunol Lett. 2005;97:107–13. Article CAS PubMed
Google Scholar Download references ACKNOWLEDGEMENTS The authors thank Tomoki Murata, Masafumi Tanji, Nanumi Han, Haruka Wada, and Yoshinori Hasegawa for their helpful discussions and
advice, and technical assistance with part of some experiments. FUNDING This work was partly supported by JST SPRING (#JPMJSP2119, NK) and JSPS KAKENHI (#22J21076, NK). AUTHOR INFORMATION
AUTHORS AND AFFILIATIONS * Division of Immunobiology, Graduate School of Medicine, Institute for Genetic Medicine, Hokkaido University, Kita-15 Nishi-7, Sapporo, 060-0815, Japan Nabeel
Kajihara, Yunqi Ge & Ken-ichiro Seino Authors * Nabeel Kajihara View author publications You can also search for this author inPubMed Google Scholar * Yunqi Ge View author publications
You can also search for this author inPubMed Google Scholar * Ken-ichiro Seino View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS NK and K-iS
designed the study. NK and YG performed experiments. All authors analysed data and discussed the results. NK and K-iS contributed to manuscript preparation. All authors approved the final
version of this manuscript for publication. CORRESPONDING AUTHOR Correspondence to Ken-ichiro Seino. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE All animal procedures were approved by the Animal Care Committee of Hokkaido University (Approval number: 19-0094). CONSENT FOR PUBLICATION Not
applicable. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY
INFORMATION SUPPLEMENTARY FIGURE RIGHTS AND PERMISSIONS Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement
with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and
applicable law. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Kajihara, N., Ge, Y. & Seino, Ki. Blocking of oestrogen signals improves anti-tumour effect regardless of
oestrogen receptor alpha expression in cancer cells. _Br J Cancer_ 129, 935–946 (2023). https://doi.org/10.1038/s41416-023-02381-0 Download citation * Received: 31 January 2023 * Revised: 10
July 2023 * Accepted: 25 July 2023 * Published: 03 August 2023 * Issue Date: 05 October 2023 * DOI: https://doi.org/10.1038/s41416-023-02381-0 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative
