Neutrophil aldh2 is a new therapeutic target for the effective treatment of sepsis-induced ards
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

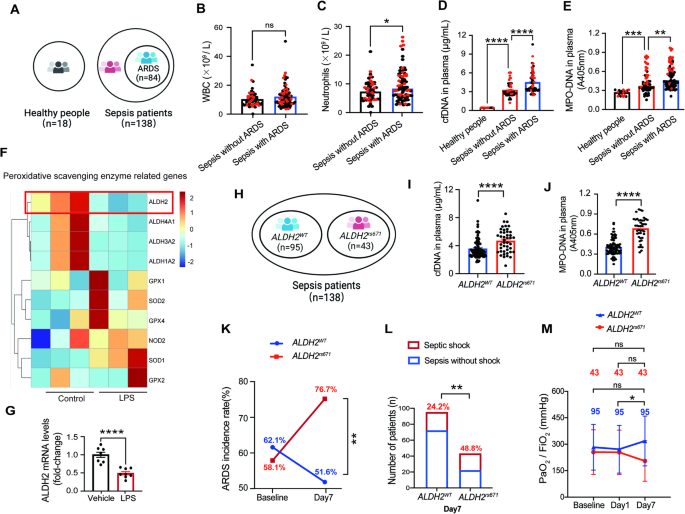
ABSTRACT Acetaldehyde dehydrogenase 2 (_ALDH2_) mutations are commonly found in a subgroup of the Asian population. However, the role of ALDH2 in septic acute respiratory distress syndrome
(ARDS) remains unknown. Here, we showed that human subjects carrying the _ALDH2__rs671_ mutation were highly susceptible to developing septic ARDS. Intriguingly, _ALDH2__rs671_-ARDS patients
showed higher levels of blood cell-free DNA (cfDNA) and myeloperoxidase (MPO)-DNA than _ALDH2__WT_-ARDS patients. To investigate the mechanisms underlying ALDH2 deficiency in the
development of septic ARDS, we utilized _Aldh2_ gene knockout mice and _Aldh2__rs671_ gene knock-in mice. In clinically relevant mouse sepsis models, _Aldh2_-/- mice and _Aldh2__rs671_ mice
exhibited pulmonary and circulating NETosis, a specific process that releases neutrophil extracellular traps (NETs) from neutrophils. Furthermore, we discovered that NETosis strongly
promoted endothelial destruction, accelerated vascular leakage, and exacerbated septic ARDS. At the molecular level, ALDH2 increased K48-linked polyubiquitination and degradation of
peptidylarginine deiminase 4 (PAD4) to inhibit NETosis, which was achieved by promoting PAD4 binding to the E3 ubiquitin ligase CHIP. Pharmacological administration of the ALDH2-specific
activator Alda-1 substantially alleviated septic ARDS by inhibiting NETosis. Together, our data reveal a novel ALDH2-based protective mechanism against septic ARDS, and the activation of
ALDH2 may be an effective treatment strategy for sepsis. Access through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS
OPTIONS Access through your institution Subscribe to this journal Receive 12 digital issues and online access to articles $119.00 per year only $9.92 per issue Learn more Buy this article *
Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn
about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS RIBONUCLEASE INHIBITOR 1 EMERGES AS A POTENTIAL BIOMARKER AND MODULATES
INFLAMMATION AND IRON HOMEOSTASIS IN SEPSIS Article Open access 28 June 2024 ENAMPT NEUTRALIZATION REDUCES PRECLINICAL ARDS SEVERITY VIA RECTIFIED NFKB AND AKT/MTORC2 SIGNALING Article Open
access 13 January 2022 DECODING THE MULTIPLE FUNCTIONS OF ZBP1 IN THE MECHANISM OF SEPSIS-INDUCED ACUTE LUNG INJURY Article Open access 21 October 2024 REFERENCES * Bos LDJ, Ware LB. Acute
respiratory distress syndrome: causes, pathophysiology, and phenotypes. Lancet. 2022;400:1145–56. PubMed Google Scholar * ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT,
Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–33. Google Scholar * Bellani G, Laffey JG, Pham T, Fan E, Brochard L,
Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. CAS
PubMed Google Scholar * Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319:698–710. PubMed Google Scholar * Rubenfeld
GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, et al. Incidence and outcomes of acute lung injury. N. Engl J Med. 2005;353:1685–93. CAS PubMed Google Scholar * Joffre J, Hellman
J, Ince C, Ait-Oufella H. Endothelial responses in sepsis. Am J Respir Crit Care Med. 2020;202:361–70. CAS PubMed Google Scholar * Jaffee W, Hodgins S, McGee WT. Tissue Edema, fluid
balance, and patient outcomes in severe sepsis: an organ systems review. J Intensive Care Med. 2018;33:502–9. PubMed Google Scholar * Chang R, Holcomb JB. Choice of fluid therapy in the
initial management of sepsis, severe sepsis, and septic shock. Shock. 2016;46:17–26. PubMed PubMed Central Google Scholar * Zhang J, Guo Y, Zhao X, Pang J, Pan C, Wang J, et al. The role
of aldehyde dehydrogenase 2 in cardiovascular disease. Nat Rev Cardiol. 2023;20:495–509. PubMed Google Scholar * Zhang J, Zhao X, Guo Y, Liu Z, Wei S, Yuan Q, et al. Macrophage ALDH2
(Aldehyde Dehydrogenase 2) stabilizing Rac2 is required for efferocytosis internalization and reduction of atherosclerosis development. Arterioscler Thromb Vasc Biol. 2022;42:700–16. CAS
PubMed PubMed Central Google Scholar * Zhang Y, Lv Y, Zhang Q, Wang X, Han Q, Liang Y, et al. ALDH2 attenuates myocardial pyroptosis through breaking down Mitochondrion-NLRP3 inflammasome
pathway in septic shock. Front Pharm. 2023;14:1125866. CAS Google Scholar * Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, et al. Conventional and genetic evidence on alcohol and
vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet. 2019;393:1831–42. PubMed PubMed Central Google Scholar * Chen CH, Ferreira JC, Gross ER,
Mochly-Rosen D. Targeting aldehyde dehydrogenase 2: new therapeutic opportunities. Physiol Rev. 2014;94:1–34. PubMed PubMed Central Google Scholar * Hsu LA, Tsai FC, Yeh YH, Chang CJ, Kuo
CT, Chen WJ, et al. Aldehyde Dehydrogenase 2 ameliorates chronic alcohol consumption-induced atrial fibrillation through detoxification of 4-HNE. Int J Mol Sci. 2020;21:6678. CAS PubMed
PubMed Central Google Scholar * Chang JS, Hsiao JR, Chen CH. ALDH2 polymorphism and alcohol-related cancers in Asians: a public health perspective. J Biomed Sci. 2017;24:19. PubMed PubMed
Central Google Scholar * Perez-Miller S, Younus H, Vanam R, Chen CH, Mochly-Rosen D, Hurley TD. Alda-1 is an agonist and chemical chaperone for the common human aldehyde dehydrogenase 2
variant. Nat Struct Mol Biol. 2010;17:159–64. CAS PubMed PubMed Central Google Scholar * Sidramagowda Patil S, Hernández-Cuervo H, Fukumoto J, Krishnamurthy S, Lin M, Alleyn M, et al.
Alda-1 attenuates hyperoxia-induced acute lung injury in mice. Front Pharm. 2020;11:597942. Google Scholar * Kuroda A, Hegab AE, Jingtao G, Yamashita S, Hizawa N, Sakamoto T, et al. Effects
of the common polymorphism in the human aldehyde dehydrogenase 2 (ALDH2) gene on the lung. Respir Res. 2017;18:69. PubMed PubMed Central Google Scholar * Oka Y, Hamada M, Nakazawa Y,
Muramatsu H, Okuno Y, Higasa K, et al. Digenic mutations in ALDH2 and ADH5 impair formaldehyde clearance and cause a multisystem disorder, AMeD syndrome. Sci Adv. 2020;6:eabd7197. CAS
PubMed Google Scholar * Hu Y, Yan JB, Zheng MZ, Song XH, Wang LL, Shen YL, et al. Mitochondrial aldehyde dehydrogenase activity protects against lipopolysaccharide‑induced cardiac
dysfunction in rats. Mol Med Rep. 2015;11:1509–15. CAS PubMed Google Scholar * Pang J, Zheng Y, Han Q, Zhang Y, Sun R, Wang J, et al. The role of ALDH2 in sepsis and the to-be-discovered
mechanisms. Adv Exp Med Biol. 2019;1193:175–94. CAS PubMed Google Scholar * Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and
adaptive immunity. Nat Rev Immunol. 2011;11:519–31. CAS PubMed Google Scholar * Liew PX, Kubes P. The neutrophil’s role during health and disease. Physiol Rev. 2019;99:1223–48. CAS
PubMed Google Scholar * Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–5. CAS PubMed
Google Scholar * Fuchs TA, Abed U, Goosmann C, Hurwitz R, Schulze I, Wahn V, et al. Novel cell death program leads to neutrophil extracellular traps. J Cell Biol. 2007;176:231–41. CAS
PubMed PubMed Central Google Scholar * Yipp BG, Kubes P. NETosis: how vital is it? Blood. 2013;122:2784–94. CAS PubMed Google Scholar * Thiam HR, Wong SL, Wagner DD, Waterman CM.
Cellular Mechanisms of NETosis. Annu Rev Cell Dev Biol. 2020;36:191–218. CAS PubMed PubMed Central Google Scholar * Chen L, Zhao Y, Lai D, Zhang P, Yang Y, Li Y, et al. Neutrophil
extracellular traps promote macrophage pyroptosis in sepsis. Cell Death Dis. 2018;9:597. PubMed PubMed Central Google Scholar * Perdomo J, Leung H, Ahmadi Z, Yan F, Chong J, Passam FH, et
al. Neutrophil activation and NETosis are the major drivers of thrombosis in heparin-induced thrombocytopenia. Nat Commun. 2019;10:1322. PubMed PubMed Central Google Scholar * Mattox AK,
Douville C, Wang Y, Popoli M, Ptak J, Silliman N, et al. The origin of highly elevated cell-free DNA in healthy individuals and patients with pancreatic, colorectal, lung, or ovarian
cancer. Cancer Discov. 2023;13:2166–2179. PubMed PubMed Central Google Scholar * Thiam HR, Wong SL, Qiu R, Kittisopikul M, Vahabikashi A, Goldman AE, et al. NETosis proceeds by
cytoskeleton and endomembrane disassembly and PAD4-mediated chromatin decondensation and nuclear envelope rupture. Proc Natl Acad Sci USA. 2020;117:7326–37. CAS PubMed PubMed Central
Google Scholar * Neubert E, Meyer D, Rocca F, Günay G, Kwaczala-Tessmann A, Grandke J, et al. Chromatin swelling drives neutrophil extracellular trap release. Nat Commun. 2018;9:3767.
PubMed PubMed Central Google Scholar * Li P, Li M, Lindberg MR, Kennett MJ, Xiong N, Wang Y. PAD4 is essential for antibacterial innate immunity mediated by neutrophil extracellular
traps. J Exp Med. 2010;207:1853–62. CAS PubMed PubMed Central Google Scholar * Martinod K, Demers M, Fuchs TA, Wong SL, Brill A, Gallant M, et al. Neutrophil histone modification by
peptidylarginine deiminase 4 is critical for deep vein thrombosis in mice. Proc Natl Acad Sci USA. 2013;110:8674–9. CAS PubMed PubMed Central Google Scholar * Biron BM, Chung CS, Chen Y,
Wilson Z, Fallon EA, Reichner JS, et al. PAD4 deficiency leads to decreased organ dysfunction and improved survival in a dual insult model of hemorrhagic shock and sepsis. J Immunol.
2018;200:1817–28. CAS PubMed Google Scholar * Alsabani M, Abrams ST, Cheng Z, Morton B, Lane S, Alosaimi S, et al. Reduction of NETosis by targeting CXCR1/2 reduces thrombosis, lung
injury, and mortality in experimental human and murine sepsis. Br J Anaesth. 2022;128:283–93. CAS PubMed Google Scholar * Pham T, Rubenfeld GD. Fifty years of research in ARDS. The
epidemiology of acute respiratory distress syndrome. a 50th birthday review. Am J Respir Crit Care Med. 2017;195:860–70. PubMed Google Scholar * Rezoagli E, Fumagalli R, Bellani G.
Definition and epidemiology of acute respiratory distress syndrome. Ann Transl Med. 2017;5:282. PubMed PubMed Central Google Scholar * Matthay MA, Zemans RL, Zimmerman GA, Arabi YM,
Beitler JR, Mercat A, et al. Acute respiratory distress syndrome. Nat Rev Dis Prim. 2019;5:18. PubMed Google Scholar * Parotto M, Gyöngyösi M, Howe K, Myatra SN, Ranzani O, Shankar-Hari M,
et al. Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations. Lancet Respir Med. 2023;11:739–54. PubMed Google Scholar * Carmona-Rivera C,
Zhao W, Yalavarthi S, Kaplan MJ. Neutrophil extracellular traps induce endothelial dysfunction in systemic lupus erythematosus through the activation of matrix metalloproteinase-2. Ann
Rheum Dis. 2015;74:1417–24. CAS PubMed Google Scholar * Kato N, Takeuchi F, Tabara Y, Kelly TN, Go MJ, Sim X, et al. Meta-analysis of genome-wide association studies identifies common
variants associated with blood pressure variation in east Asians. Nat Genet. 2011;43:531–8. CAS PubMed PubMed Central Google Scholar * Ma H, Guo R, Yu L, Zhang Y, Ren J. Aldehyde
dehydrogenase 2 (ALDH2) rescues myocardial ischaemia/reperfusion injury: role of autophagy paradox and toxic aldehyde. Eur Heart J. 2011;32:1025–38. CAS PubMed Google Scholar * Dingler
FA, Wang M, Mu A, Millington CL, Oberbeck N, Watcham S, et al. Two aldehyde clearance systems are essential to prevent lethal formaldehyde accumulation in mice and humans. Mol Cell.
2020;80:996–1012.e9. CAS PubMed PubMed Central Google Scholar * Liu H, Hu Q, Ren K, Wu P, Wang Y, Lv C. ALDH2 mitigates LPS-induced cardiac dysfunction, inflammation, and apoptosis
through the cGAS/STING pathway. Mol Med. 2023;29:171. CAS PubMed PubMed Central Google Scholar * Jin J, Chang RS, Xu S, Xia G, Wong J, Fang Y, et al. Aldehyde Dehydrogenase 2 ameliorates
LPS-induced acute kidney injury through detoxification of 4-HNE and suppression of the MAPK pathway. J Immunol Res. 2023;2023:5513507. PubMed PubMed Central Google Scholar * Ji W, Wan T,
Zhang F, Zhu X, Guo S, Mei X. Aldehyde Dehydrogenase 2 protects against lipopolysaccharide-induced myocardial injury by suppressing mitophagy. Front Pharm. 2021;12:641058. CAS Google
Scholar * Ning L, Wei W, Wenyang J, Rui X, Qing G. Cytosolic DNA-STING-NLRP3 axis is involved in murine acute lung injury induced by lipopolysaccharide. Clin Transl Med. 2020;10:e228.
PubMed PubMed Central Google Scholar * Rittirsch D, Huber-Lang MS, Flierl MA, Ward PA. Immunodesign of experimental sepsis by cecal ligation and puncture. Nat Protoc. 2009;4:31–6. CAS
PubMed PubMed Central Google Scholar * Ho J, Chan H, Liang Y, Liu X, Zhang L, Li Q, et al. Cathelicidin preserves intestinal barrier function in polymicrobial sepsis. Crit Care.
2020;24:47. PubMed PubMed Central Google Scholar * Han S, Lee SJ, Kim KE, Lee HS, Oh N, Park I, et al. Amelioration of sepsis by TIE2 activation-induced vascular protection. Sci Transl
Med. 2016;8:335ra55. PubMed Google Scholar * Peng X, Hassoun PM, Sammani S, McVerry BJ, Burne MJ, Rabb H, et al. Protective effects of sphingosine 1-phosphate in murine endotoxin-induced
inflammatory lung injury. Am J Respir Crit Care Med. 2004;169:1245–51. PubMed Google Scholar * Kulkarni HS, Lee JS, Bastarache JA, Kuebler WM, Downey GP, Albaiceta GM, et al. Update on the
features and measurements of experimental acute lung injury in animals: An Official American Thoracic Society Workshop Report. Am J Respir Cell Mol Biol. 2022;66:e1–e14. CAS PubMed PubMed
Central Google Scholar * Jin H, Aziz M, Murao A, Kobritz M, Shih AJ, Adelson RP, et al. Antigen-presenting aged neutrophils induce CD4+ T cells to exacerbate inflammation in sepsis. J
Clin Invest. 2023;133:e164585. CAS PubMed PubMed Central Google Scholar * Kim B, Jang C, Dharaneeswaran H, Li J, Bhide M, Yang S, et al. Endothelial pyruvate kinase M2 maintains vascular
integrity. J Clin Invest. 2018;128:4543–56. PubMed PubMed Central Google Scholar * Newman AM, Bratman SV, To J, Wynne JF, Eclov NC, Modlin LA, et al. An ultrasensitive method for
quantitating circulating tumor DNA with broad patient coverage. Nat Med. 2014;20:548–54. CAS PubMed PubMed Central Google Scholar * Middleton EA, He XY, Denorme F, Campbell RA, Ng D,
Salvatore SP, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–79. CAS PubMed Google Scholar *
Najmeh, S, Cools-Lartigue J, Giannias B, Spicer J, Ferri LE, Simplified Human Neutrophil Extracellular Traps (NETs) Isolation and Handling. J Vis Exp. 2015;98:52687. * Deng M, Tang Y, Li W,
Wang X, Zhang R, Zhang X, et al. The endotoxin delivery protein HMGB1 mediates Caspase-11-dependent lethality in sepsis. Immunity. 2018;49:740–753.e7. CAS PubMed PubMed Central Google
Scholar Download references ACKNOWLEDGEMENTS This study was supported by the State Key Program of the National Natural Science Foundation of China (82030059), the National Science Fund for
Distinguished Young Scholars (82325031), the National Natural Science Regional Innovation Fund Joint Fund Key Support Projects (U23A20485), the National Natural Science Foundation of China
(82072144, 82172127), the National Key R&D Program of China (2020YFC1512700, 2020YFC1512705, 2020YFC1512703), the Key R&D Program of Shandong Province (2021ZLGX02, 2021SFGC0503,
2022ZLGX03), the Taishan Pandeng Scholar Program of Shandong Province (tspd20181220), the Taishan Young Scholar Program of Shandong Province (tsqn202211312), the Clinical Research Project of
Shandong University (2021SDUCRCC006), and the Interdisciplinary Young Researcher Groups Program of Shandong University (2020QNQT004). Illustrations were made using BioRender. AUTHOR
INFORMATION Author notes * These authors contributed equally: Changchang Xu, Lin Zhang. AUTHORS AND AFFILIATIONS * Department of Emergency Medicine, Qilu Hospital of Shandong University,
Jinan, China Changchang Xu, Lin Zhang, Shaoyu Xu, Zichen Wang, Qi Han, Ying Lv, Xingfang Wang, Xiangxin Zhang, Qingju Zhang, Ying Zhang, Simeng He, Qiuhuan Yuan, Yuan Bian, Chuanbao Li,
Jiali Wang, Feng Xu, Jiaojiao Pang & Yuguo Chen * Chest Pain Center, Shandong Provincial Clinical Research Center for Emergency and Critical Care Medicine, Institute of Emergency and
Critical Care Medicine of Shandong University, Qilu Hospital of Shandong University, Jinan, China Changchang Xu, Lin Zhang, Shaoyu Xu, Zichen Wang, Qi Han, Ying Lv, Xingfang Wang, Xiangxin
Zhang, Qingju Zhang, Ying Zhang, Simeng He, Qiuhuan Yuan, Yuan Bian, Chuanbao Li, Jiali Wang, Feng Xu, Jiaojiao Pang & Yuguo Chen * Key Laboratory of Emergency and Critical Care Medicine
of Shandong Province, Key Laboratory of Cardiopulmonary-Cerebral Resuscitation Research of Shandong Province, Shandong Provincial Engineering Laboratory for Emergency and Critical Care
Medicine, Qilu Hospital of Shandong University, Jinan, China Changchang Xu, Lin Zhang, Shaoyu Xu, Zichen Wang, Qi Han, Ying Lv, Xingfang Wang, Xiangxin Zhang, Qingju Zhang, Ying Zhang,
Simeng He, Qiuhuan Yuan, Yuan Bian, Chuanbao Li, Jiali Wang, Feng Xu, Jiaojiao Pang & Yuguo Chen * The Key Laboratory of Cardiovascular Remodeling and Function Research, Chinese Ministry
of Education, Chinese Ministry of Health and Chinese Academy of Medical Sciences, The State and Shandong Province Joint Key Laboratory of Translational Cardiovascular Medicine, Qilu
Hospital of Shandong University, Jinan, China Changchang Xu, Lin Zhang, Shaoyu Xu, Zichen Wang, Qi Han, Ying Lv, Xingfang Wang, Xiangxin Zhang, Qingju Zhang, Ying Zhang, Simeng He, Qiuhuan
Yuan, Yuan Bian, Chuanbao Li, Jiali Wang, Feng Xu, Jiaojiao Pang & Yuguo Chen * Department of Microbiology, Tumor and Cell Biology, Karolinska Institute, Stockholm, 171 65, Sweden Yihai
Cao Authors * Changchang Xu View author publications You can also search for this author inPubMed Google Scholar * Lin Zhang View author publications You can also search for this author
inPubMed Google Scholar * Shaoyu Xu View author publications You can also search for this author inPubMed Google Scholar * Zichen Wang View author publications You can also search for this
author inPubMed Google Scholar * Qi Han View author publications You can also search for this author inPubMed Google Scholar * Ying Lv View author publications You can also search for this
author inPubMed Google Scholar * Xingfang Wang View author publications You can also search for this author inPubMed Google Scholar * Xiangxin Zhang View author publications You can also
search for this author inPubMed Google Scholar * Qingju Zhang View author publications You can also search for this author inPubMed Google Scholar * Ying Zhang View author publications You
can also search for this author inPubMed Google Scholar * Simeng He View author publications You can also search for this author inPubMed Google Scholar * Qiuhuan Yuan View author
publications You can also search for this author inPubMed Google Scholar * Yuan Bian View author publications You can also search for this author inPubMed Google Scholar * Chuanbao Li View
author publications You can also search for this author inPubMed Google Scholar * Jiali Wang View author publications You can also search for this author inPubMed Google Scholar * Feng Xu
View author publications You can also search for this author inPubMed Google Scholar * Yihai Cao View author publications You can also search for this author inPubMed Google Scholar *
Jiaojiao Pang View author publications You can also search for this author inPubMed Google Scholar * Yuguo Chen View author publications You can also search for this author inPubMed Google
Scholar CONTRIBUTIONS Y Chen and JP conceived and designed the experiments. CX and LZ performed most of the experiments with the help of SX, ZW, QH, YL, XW, XZ, QZ, YZ, SH, and QY CX, LZ,
SX, ZW, and YB performed the data analysis. Y Cao and JP assisted in revising the draft. CL, JW, and FX provided valuable experimental advice and guidance. All authors have read and approved
the final manuscript. CORRESPONDING AUTHORS Correspondence to Jiaojiao Pang or Yuguo Chen. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare that the research was conducted in the
absence of any commercial or financial relationships that could be construed as potential conflicts of interest. SUPPLEMENTARY INFORMATION 41423_2024_1146_MOESM1_ESM.DOCX Sup Fig1-11,
Tab1-5, unprocessed original images (Supplementary Materials for Neutrophil ALDH2 is a new therapeutic target for effective treatment of sepsis-triggered ARDS) RIGHTS AND PERMISSIONS
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author
self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law. Reprints and permissions ABOUT THIS ARTICLE
CITE THIS ARTICLE Xu, C., Zhang, L., Xu, S. _et al._ Neutrophil ALDH2 is a new therapeutic target for the effective treatment of sepsis-induced ARDS. _Cell Mol Immunol_ 21, 510–526 (2024).
https://doi.org/10.1038/s41423-024-01146-w Download citation * Received: 03 October 2023 * Accepted: 09 February 2024 * Published: 12 March 2024 * Issue Date: May 2024 * DOI:
https://doi.org/10.1038/s41423-024-01146-w SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * NETosis * ALDH2 * ARDS * Sepsis
