A novel germline mutation of the sftpa1 gene in familial interstitial pneumonia
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT Different genes related to alveolar stability have been associated with familial interstitial pneumonia (FIP). Here, we report a novel, rare _SFTPA1_ variant in a family with
idiopathic interstitial pneumonia (IIP). We performed whole-exome sequencing on germline DNA samples from four members of one family; three of them showed signs of pulmonary fibrosis
(idiopathic interstitial pneumonia) with autosomal-dominant inheritance. A heterozygous single nucleotide variant c.532 G > A in the _SFTPA1_ gene has been identified. This variant
encodes the substitution p.(Val178Met), localized within the carbohydrate recognition domain of surfactant protein A and segregates with the genes causing idiopathic interstitial pneumonia.
This rare variant has not been previously reported. We also analyzed the detected sequence variant in the protein structure _in silico_. The replacement of valine by the larger methionine
inside the protein may cause a disruption in the protein structure. The c.532 G > A variant was further validated using Sanger sequencing of the amplicons, confirming the diagnosis in all
symptomatic family members. Moreover, this variant was also found by Sanger sequencing in one other symptomatic family member and one young asymptomatic family member. The
autosomal-dominant inheritance, the family history of IIP, and the evidence of a mutation occurring in part of the _SFTPA1_ gene all suggest a novel variant that causes FIP. SIMILAR CONTENT
BEING VIEWED BY OTHERS WHOLE-EXOME SEQUENCING IDENTIFIES SUSCEPTIBILITY GENES AND PATHWAYS FOR IDIOPATHIC PULMONARY FIBROSIS IN THE CHINESE POPULATION Article Open access 14 January 2021
IDENTIFICATION OF A MISSENSE VARIANT IN _SPDL1_ ASSOCIATED WITH IDIOPATHIC PULMONARY FIBROSIS Article Open access 23 March 2021 HYPOMORPHIC PATHOGENIC VARIANT IN _SFTPB_ LEADS TO ADULT
PULMONARY FIBROSIS Article 28 June 2023 INTRODUCTION Familial interstitial pneumonia (FIP) is defined as idiopathic interstitial pneumonia (IIP) and affects two or more first-degree
relatives who have been diagnosed with characteristics of IIP1. IIP belongs to a group of interstitial lung diseases (ILDs). ILDs are a heterogeneous group of predominantly chronic diseases
characterized by various degrees of inflammation and pulmonary fibrosis at the level of the interstitium, alveolar ducts, alveoli, pulmonary capillaries and respiratory bronchioles2. There
is evidence that the development of pulmonary fibrosis is genetically determined, and genetic testing is considered for IIP cases with (1) familial clustering of IIP; (2) IIP associated with
other inherited disorders; or (3) when there is significant variability in the development of pulmonary fibrosis among individuals exposed to a dusty environment3. Moreover, several
phenotypes of fibrotic interstitial lung processes may be present in members of one family. Idiopathic pulmonary fibrosis/usual idiopathic pneumonia (IPF/UIP) is the most frequently observed
phenotype in the familial occurrence of IIP4. There are no differences in clinical, radiologic, or histological features between familial IPF and nonfamilial IPF cases5. In FIP, many genes
may be pathogenic. FIP risk factor genes include telomerase catalytic activity genes (_TERT –_ telomerase reverse transcriptase; _TERC –_ telomerase RNA component), genes affecting
telomerase biogenesis (_DKC1_ – dyskerin; PARN _–_ polyadenylation-specific ribonuclease deadenylation nuclease; _NAF1 –_ nuclear assembly factor 1 ribonucleoprotein) and genes that alter
telomeres (_TINF2 –_ telomere-interacting factor 2; _RTEL1 –_ regulator of telomere-elongation helicase-1). Mutations associated with adult-onset FIP are also rarely found in genes that
encode surfactant proteins, such as the heterozygous mutations of surfactant proteins A and C (_SFTPA1, SFTPA2_, and _SFTPC_). Rare biallelic variants in the genes encoding surfactant
protein B (_SFTPB_) and branched-chain amino acid aminotransferase (_BCA3_) have also been described. Altogether, mutations in _SFTPC, SFTPA2, TERT_, and _TERC_ clarify a maximum of 20% of
all FIP cases6,7,8,9,10,11,12,13,14,15,16,17. However, common variants (an allele frequency in the population above 5%) in genes associated with a risk of FIP and IPF have been observed.
Most often, the single nucleotide polymorphism (SNP) rs35705950 of the _MUC5B_ gene has been strongly associated with both FIP and IPF across multiple different cohorts18,19. Here, we
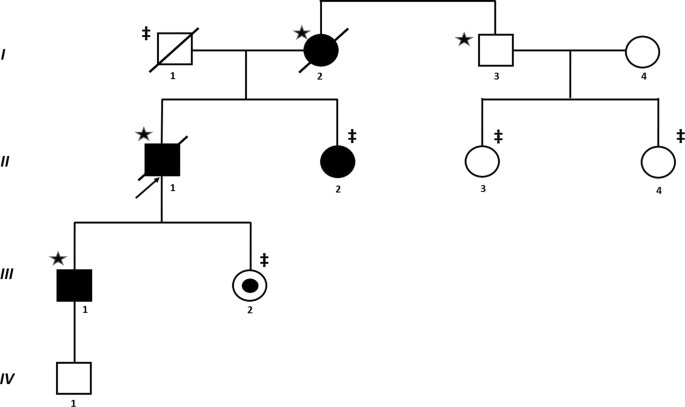
present the FIP case in which we have revealed a novel germline pathogenic variant in the _SFTPA1_ gene. MATERIALS AND METHODS SUBJECTS THE PROBAND Figure 1 (_II-1_) was a male nonsmoker who
was referred to the Department of Pneumology and Phtiseology, University Hospital, Brno, Czech Republic because of IIP at the age of 46 years. The diagnosis of IIP was based on standard
criteria2. The proband presented with dyspnea and a dry cough. Lung function testing showed a restrictive syndrome with a mild reduction in diffuse lung capacity. High-resolution computed
tomography (HRCT) of the patient’s chest showed interlobular septal thickening and ground glass opacities, especially in the lower lung areas (Fig. 2a). Video-assisted thoracoscopic (VATS)
lung biopsy revealed pulmonary fibrosis with a nonspecific interstitial pneumonia pattern. He died of respiratory failure due to acute exacerbation of pulmonary fibrosis 11 years after
diagnosis. A detailed family history revealed that several of the patient’s family members had pulmonary fibrosis or interstitial lung involvement. The proband´s mother (_I-2_), a nonsmoker,
died of respiratory failure at the age of 73 years. She was diagnosed with IIP seven years ago. HRCT of the thorax initially showed predominant ground glass opacities, inter- and
intralobular septal thickening and bronchiectasis that did not correspond with the possible, typical interstitial pneumonia (Fig. 2b). However, a VATS lung biopsy and histological
examination revealed a pattern of typical interstitial pneumonia. The clinical course gradually deteriorated over time despite therapy. THE PROBAND´S SISTER (II-2), a nonsmoker with digital
clubbing, developed dyspnea at the age of 44 years. An HRCT of her thorax showed ventral and dorsobasal subpleural interlobular septal thickening. THE PROBAND´S SON (III-1), a nonsmoker, had
suffered from shortness of breath during exercise since the age of 25. He also developed digital clubbing. An HRCT of his thorax revealed discrete nonspecific ground glass opacities in the
upper and lower right lobes. THE PROBAND´S DAUGHTER (_III-2_), a nonsmoker, was asymptomatic. All results of the clinical and radiology examinations, functional tests and treatment of family
members with pulmonary symptoms are summarized in Supplemental Table S1. The pedigree analysis (Fig. 1) indicates an autosomal-dominant mode of inheritance. FIP was therefore suspected, and
diagnostics were extended by genetic testing of the family members, who gave written informed consent according to the Declaration of Helsinki. MUTATIONAL SCREENING Blood samples from nine
family members were collected and processed for genomic DNA isolation using the MagCore® Genomic DNA Whole Blood Kit (RBC Bioscience, USA). We performed whole-exome sequencing (WES) on
samples from four family members (I-2, I-3, II-1, and III-1). Whole-exome libraries were prepared using the Kapa Hyper Prep Kit (Roche, USA) according to the protocol for NimbleGen SeqCap EZ
Exome v3 (Roche, USA). Paired-end 2 × 75 bp sequencing was performed on an Illumina NextSeq 500 sequencer (Illumina Inc., USA). The raw sequencing reads were aligned to the GRCh37 human
reference genome using the BWA mem algorithm, version 0.7.15. PCR duplicates were identified with the MarkDuplicates tool from Picard version 2.9.2. GATK HaplotypeCaller, version 3.7, was
used to detect germline single nucleotide variants (SNV) and indels. Obtained variants/indels have been annotated using Annovar program version (2018Apr16). On the basis of the current
knowledge, we have chosen 30 candidate genes previously associated with _IPF_: _TERC_, _TERT_, _SFTPC_, _SFTPA1_, _SFTPA2_, _MUC5B_, _MUC5C_, _RTEL1_, _PARN_, _ABCA3_, _DKC1_, _TINF2_,
_IL1RN_, _IL8_, _FAM13A_, _TLR3_, _HLA- DRB1_, _HLA- DQB1_, _DSP_, _OBFC1_, _MUC2_, _TOLLIP_, _ATP11A_, _MDGA2_, _MAPT_, _SPPL2C_, _DPP9_, _TGFB1_, _NAF1_, and
_OBFC1_7,8,9,10,11,12,13,14,15,16,17. We then looked more deeply into the exonic variants of these genes. RESULTS The analysis revealed a novel variation c.532 G > A in exon 6 of the
_SFPTA1_ gene (reference sequence: NM_005411.4), located within the carbohydrate recognition domain of surfactant protein A. The variant was found to be heterozygous in three affected family
members (I-2, II-1, III-1) with IIP but was absent in the healthy individual I-3 (Fig. 1). The coverage range of c.532 G > A was 66–126 in all affected samples, and the variant allele
frequency range was 41.41%-59.09%. This identified variant (c.532 G > A) has not been described previously and is absent in the ExAC, 1000 genomes, ESP (exome sequencing projects) 6500,
KAVIAR, gnomAD, and HGMD databases20,21. The c.532 G > A variant was further validated using PCR and Sanger sequencing of the amplicons, confirming the diagnosis in all affected family
members (I-2, II-1, and III-1). Due to the similarity of the _SFTPA1_ and _SFTPA2_ genes, we designed a specific primer set corresponding to the differences in the nucleotide sequence
(forward primer: 5´-TGGTCAGTGGCCTGACCC-3´ and reverse primer: 5´-AGAGTCAGGGCCCATCAGA-3´). PCR was performed with an annealing temperature of 60 °C using Q5 High-Fidelity DNA Polymerase (New
England Biolabs Inc., England) according to the manufacturer´s protocol. PCR products were purified using a Qiaquick PCR purification kit (QIAGEN, Germany). Capillary sequencing was
performed using BigDye-terminator chemistry on a 3500 Genetic Analyzer (Applied Biosystems, USA). The analysis showed that the variant c.532 G > A was heterozygous in the I-2, II-1, II-2
and III-1 family members (Fig. 3). Subsequently, PCR and Sanger sequencing of c.532 G > A was performed in the other family members (I-1, II-2, II-3, II-4, and III-2). Moreover, the c.532
G > A heterozygous variant was found in two additional family members: II-2 with disease symptoms and III-2, the young but still asymptomatic family member. IN SILICO ANALYSIS Currently,
there is no evidence for any known functional impacts of the c.532 G > A; p.Val178Met variant in the _SFPTA1_ gene, which encodes the missense substitution valine to methionine in the
α-helix (the carbohydrate recognition domain of surfactant protein A1). Valine178 is a highly conserved amino acid and is found in up to 11 frog species. We performed an assessment of the
severity of the identified variant using _in silico_ prediction analysis: the Sorting Intolerant from Tolerant (SIFT), Polymorphism Phenotyping v2 (Poly-Phen-2), MutationTaster, Align GVGD
and CADD_phred programs (http://sift.jcvi.org/www/SIFT_seq_submit2.html; http://genetics.bwh.harvard.edu/pph/; http://www.mutationtaster.org/; http://agvgd.hci.utah.edu/agvgd_input.php)22.
According to SIFT, this variant with a score of 0.01 was “deleterious” (the score of predicted damage was < 0.05). The Poly-Phen-2 program evaluated p.Val178Met as “probably damaging”
with a score of 1,0 (a maximum score). On the other hand, MutationTaster predicted this variant as a “polymorphism” with a p-value of 1 (score of predicted damage is < 0.09), and the
Align GVGD (Grantham Variation and Grantham Deviation) defined “the lowest risk” for the prediction of missense substitutions with the grade C0 (C0 is the first of a total of seven grades).
However, the scaled CADD_phred score was calculated as 16.72. This result of scaled transformation was assigned to the top 1% of single nucleotide variants and may predict a potentially
pathogenic variant. We therefore analyzed the c.532 G > A; p.Val178Met variant effects via protein structure modeling. Currently, there is no available crystal structure of this human
protein, so we used the homolog protein structure of porcine surfactant protein D neck and carbohydrate recognition domains complexed with mannose (PDB code 4DN8), which shows 43% sequence
homology with the human protein. In the homology model, valine178 is positioned in the α-helix, which is buried inside the protein. The replacement of this valine (its volume is 140.0 Å3)23
by larger methionine (its volume is 162.9 Å3) will probably cause a disruption of the protein structure (supplemental Figure S1). DISCUSSION Unfortunately, we do not have accurate FIP
prevalence and incidence data. However, some studies estimate that the incidence of FIP is approximately 2-10% of all IIP cases1,3,8,12. The inheritance of FIP is most commonly
autosomal-dominant with incomplete penetrance4,5,19,24,25,26. Autosomal-recessive types of inheritance have rarely been described27. Our case shows signs of an autosomal-dominant
inheritance. Both familial and sporadic cases of pulmonary fibrosis are not clinically or histologically recognizable, although familial cases can be diagnosed in younger individuals3. Rosas
et al.28 determined the clinical, radiographic, and histological features of asymptomatic ILDs in the relatives of patients with FIP. Histopathological findings in patients with FIP are
heterogeneous29. Steele et al.4 described several histopathological subtypes of IIP found in members of one family. Our case also shows different histological, clinical and radiological
findings in affected individuals. FIP is caused mainly by rare pathogenic gene variants (with an allele frequency in the population of less than 0.1%)30. Familial studies have found
FIP-associated genes influencing alveolar stability: _SFTPA1_15, _SFTPA2_14, and _SFTPC_;30,31,32 _ABCA3_ (ATP-binding cassette - type 3);32 genes related to telomerases, including _TERT_29,
and _TERC_;6,29 _DKC1_ (dyskeratin);8,29 _TINF2_;7,9,29 or _RTEL1_10,11,29,33. On the other hand, common variants are also observed in FIP; most often, the variant rs35705950 is located in
the promoter region of the _MUC5B_ gene29,34. Surfactant proteins (SPs) are divided into hydrophilic (SP-A and SP-D) and hydrophobic (SP-B and SP-C) categories. SP-A, SP-B, SP-C and SP-D are
synthesized by type II alveolar epithelial cells. SP-A and SP-D play roles in lung defense, and SP-B and SP-C ensure proper surfactant function35,36. The main protein of pulmonary
surfactant is SP-A37. The two closely related genes, _SFTPA1_ and _SFTPA2_, are located near _SFTPD_ on chromosome 10q22.3 and encode SP-A. The nucleotide sequence of the _SFTPA1_ gene is
70% identical to that of _SFTPA2_. The pathogenic variants of _SFTPA1_ and _SFTPA2_ can cause FIP and pulmonary adenocarcinoma. All pathogenic heterozygous mutations in the _SFTPA1_ and
_SFTPA2_ genes are missense and lead to a decreased secretion of mature protein by alveolar cells15,38,39,40. In our case, the novel single nucleotide variant c.532 G > A was detected in
the _SFTPA1_ gene and encodes a p.Val178Met substitution. To date, 5 missense/nonsense _SFTPA1_ variants have been identified (https://portal.biobase-international.com/hgmd/pro/gene.php?gene
= SFTPA1; 09 AUG 2018)15,20,41. Nathan et al. described in detail a molecular defect in _SFTPA1_ in FIP15. Unfortunately, there is no consensus to determine which IPF patient could benefit
from genetic testing. The international guidelines for IPF did not recommend genetic testing42, and genetic testing is not even mentioned in the guidelines43. On the other hand, the
international guidelines for IIP published in 2013 propose searching for genetic abnormalities in patients with FIP44. As proposed by Kropski et al.45, genetic testing is not recommended for
every ILD patient. Genetic counseling should be offered to patients with FIP, to patients with IIP in the context of rare inherited disorders, to individuals with disease onset before the
age of 18 years, or to patients with significant variability in the development of pulmonary fibrosis after exposure to a dusty environment3,45. For asymptomatic patients (similar to our
patient III-2), a chest HRCT is recommended at age 40 or 10 years before the age of disease onset in the proband. If signs of ILD are not present, an HRCT scan should be repeated every 5
years35. In conclusion, we have described a novel _SFTPA1_ heterozygous variant in family members with IIP. Such findings are of the utmost importance, and an early FIP diagnosis for the
patient’s family members will allow for effective therapies, including early lung transplantation or treatment, following clinical trials. REFERENCES * Talbert, J. L., Schwartz, D. A. &
Steele, M. S. Familial interstitial pneumonia. _Clin. Pulm. Med._ 21, 120–127 (2014). Article PubMed PubMed Central Google Scholar * American Thoracic Society/EuropeanRespiratory Society
International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS) and the European Respiratory
Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Americant Thoracic Society; European Respiratory Society. A_m. J. Respir.
Crit. Care Med_. 165, 277–304 (2002). * Spagnolo, P., Luppi, F., Cerri, S. & Richeldi, L. Genetic testing in difuse parenchymal lung disease. _Orphanet J. Rare. Dis_. 7,
https://doi.org/10.1186/1750-1172-7-79 (2012). Article PubMed PubMed Central Google Scholar * Steele, M. P. et al. Clinical and pathologic features of familial interstitial pneumonia.
_Am. J. Respir. Crit. Care. Med._ 172, 1146–1152 (2005). Article PubMed PubMed Central Google Scholar * Lee, H. L. et al. Familial idiopathic pulmonary fibrosis: clinical features and
outcome. _Chest_ 127, 2034–2041 (2005). Article PubMed Google Scholar * Armanious, M. Y. et al. Telomerase mutations in families with idiopathic pulmonary fibrosis. _N. Engl. J. Med._
356, 1317–1326 (2007). Article Google Scholar * Tsakiri, K. D. et al. Adult – onset pulmonary fibrosis cause by mutations in telomerase. _Proc. . Natl Acad. Sci. USA_ 104, 7552–7557
(2007). Article CAS PubMed PubMed Central Google Scholar * Kropsi, J. A. et al. A novel dyskeratin (DKC1) mutation is associated with familial interstitial pneumonia. _Chest_ 146, e1–e7
(2014). Article Google Scholar * Alder, J. K. et al. Exome sequencing idetifies mutant TINF2 in family with pulmonary fibrosis. _Chest_ 147, 1361–1368 (2015). Article PubMed Google
Scholar * Cogan, J. D. et al. Rare variants in RTEL1 are associated with familial interstitial pneumonia. _Am. J. Respir. Crit. Care. Med._ 191, 646–655 (2015). Article CAS PubMed PubMed
Central Google Scholar * Stuart, B. D. et al. Exome sequencing links mutations in PARN and RTEL1 with familial pulmonary fibrosis and telomere shortening. _Nat. Genet._ 47, 512–517
(2015). Article CAS PubMed PubMed Central Google Scholar * Moorsel, C. H. et al. Surfactant protein C mutations are the basis of a significant portion of adult familial pulmonary
fibrosis in a dutch cohort. _Am. J. Respir. Crit. Care. Med._ 182, 1419–1425 (2010). Article PubMed CAS Google Scholar * Campo, I., _et_ _al_. A large kindred of pulmonary fibrosis
associated with a novel ABCA3 gene variant. _Respir. Res_. 15, https://doi.org/10.1186/1465-9921-15-43 (2014). Article PubMed PubMed Central CAS Google Scholar * Wang, Y. et al. Genetic
defects in surfactant protein A2 are associated with pulmonary fibrosis and lung cancer. _Am. J. Hum. Genet._ 84, 52–59 (2009). Article CAS PubMed PubMed Central Google Scholar *
Nathan, N. et al. Germline SFTPA1 mutation in familial idiopathic interstitial pneumonia and lung cancer. _Hum. Mol. Genet._ 25, 1457–1467 (2016). Article CAS PubMed Google Scholar *
Lawson, W. E., Loyd, J. E. & Degryse, A. L. Genetics in pulmonary fibrosis – familial cases provide clues to the pathogenesis of idiopathic pulmonary fibrosis. _Am. J. Med. Sci._ 341,
439–443 (2011). Article PubMed PubMed Central Google Scholar * Doan, M. L. et al. Clinical, radiological and pathological features of ABCA3 mutations in children. _Thorax_ 63, 366–373
(2008). Article CAS PubMed Google Scholar * Fingerlin, T. E. et al. Genome-wide association study identifies multiple susceptibility loci for pulmonary fibrosis. _Nat. Genet._ 45,
613–620 (2013). Article CAS PubMed PubMed Central Google Scholar * Roy, M. G. et al. Muc5b is required for airway defence. _Nature_ 505, 412–416 (2014). Article CAS PubMed Google
Scholar * Stenson, P. D. et al. The Human Gene Mutation Database: towards a comprehensive repository of inherited mutation data for medical research, genetic diagnosis and next-generation
sequencing studies. _Hum. Genet._ 136, 665–677 (2017). Article CAS PubMed PubMed Central Google Scholar * Lek, M. et al. Analysis of protein-coding genetic variation in 60,706 humans.
_Nature_ 536, 285–291 (2016). Article CAS PubMed PubMed Central Google Scholar * Kircher, M. et al. A general framework for estimating the relative pathogenicity of human genetic
variants. _Nat. Genet._ 46, 310–315 (2014). Article CAS PubMed PubMed Central Google Scholar * Zamyatnin, A. A. Protein volume in solution. _Prog. Biophys. Mol. Biol._ 24, 107–123
(1972). Article CAS PubMed Google Scholar * Hodgson, U., Laitinen, T. & Tukiainen, P. Nationwide prevalence of sporadic and familial idiopathic pulmonary fibrosis: evidence of
founder effect among multiplex families in Finland. _Thorax_ 57, 338–342 (2002). Article CAS PubMed PubMed Central Google Scholar * Musk, A. W., Zilko, P. J., Manners, P., Kay, P. H.
& Kamboh, M. I. Genetic studies in familial fibrosing alveolitis. Possible linkage with immunoglobulin allotypes (Gm). _Chest_ 89, 206–210 (1986). Article CAS PubMed Google Scholar *
Marney, A., Lane, K. B., Phillips, J. A., Riley, D. J. & Loyd, J. E. Idiopathic pulmonary fibrosis can be an autosomal dominant trait in some families. _Chest_ 120((Suppl.1), 56S
(2001). Article CAS PubMed Google Scholar * Marshall, R. P., Puddicombe, A., Cookson, W. O. & Laurent, G. J. Adult familial cryptogenic fibrosing alveolitis in the United Kingdom.
_Thorax_ 5, 143–146 (2000). Article Google Scholar * Rosas, I. O. et al. Early interstitial lung disease in familial pulmonary fibrosis. _Am. J. Respir. Crit. Care. Med._ 176, 698–705
(2007). Article PubMed PubMed Central Google Scholar * Kaur, A., Mathai, S. K. & Schwartz, D. A. Genetics in idiopathic pulmonary fibrosis. Pathogenesis, prognosis, and treatment.
_Front. Med._ 4, https://doi.org/10.3389/fmed.2017.00154 (2017). * Nogee, L. M. et al. A mutation in the surfactant protein C gene associated with familial interstitial lung disease. _N.
Engl. J. Med._ 344, 573–579 (2001). Article CAS PubMed Google Scholar * Tanjore, H. et al. Alveolar epithelial cells undergo epithelial-to-mesenchymal transition in response to
endoplasmic reticulum stress. _J. Biol. Chem._ 286, 30972–30980 (2011). Article CAS PubMed PubMed Central Google Scholar * Crossno, P. F. et al. Identification of early interstitial
lung disease in an individual with genetic variations in ABCA3 and SFTPC. _Chest_ 137, 969–973 (2010). Article CAS PubMed PubMed Central Google Scholar * Kannegiesser, C. et al.
Heterozygous RTEL1 mutations are associated with familial pulmonary fibrosis. _Eur. Respir. J._ 46, 474–485 (2015). Article CAS Google Scholar * Seibold, M. A. et al. A common MUC5B
promoter polymorphism and pulmonary fibrosis. _N. Engl. J. Med._ 364, 1503–1512 (2011). Article CAS PubMed PubMed Central Google Scholar * Borrie, R. et al. Management of suspected
monogenic lung fibrosis in a specialised centre. _Eur. Respir. Rev._ 26, 160122 (2017). pii. Article Google Scholar * Whitsett, J. A. Genetic basis of familial interstitial lung disease:
misfolding or function of surfactant protein C? _Am. J. Respir. Crit. Care. Med._ 165, 1201–1202 (2002). Article PubMed Google Scholar * Han, S. & Mallampalli, R. K. The role of
surfactant in lung disease and host defense against pulmonary infections. _Ann. Am. Thorac. Soc._ 12, 765–774 (2015). Article PubMed PubMed Central Google Scholar * Kolble, K., Lu, J.,
Mole, S. E., Kaluz, S. & Reid, K. B. Assignment of the human pulmonary surfactant protein D gene (SFTP4) to 10q22-q23 close to the surfactant protein A gene cluster. _Genomics_ 17,
294–298 (1993). Article CAS PubMed Google Scholar * Lawson, W. E. et al. Endoplasmic reticulum stress in alveolar epithelial cells is prominent in IPF: association with altered
surfactant protein processing and herpesvirus infection. _Am. J. Physiol. Lung Cell. Mol. Physiol._ 249, L1119–L1126 (2008). Article CAS Google Scholar * Whitsett, J. A., Wert, S. E.
& Weaver, T. E. Diseases of pulmonary surfactant homeostasis. _Annu. Rev. Pathol._ 10, 371–393 (2015). Article CAS PubMed PubMed Central Google Scholar * Selman, M. et al.
Surfactant protein A and B genetic variants predispose to indiopathic pulmonary fibrosis. _Hum. Genet._ 113, 542–550 (2003). Article CAS PubMed Google Scholar * Raghu, G. et al. An
official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-gased guidelines for diagnosis and management. _Am. J. Respir. Crit. Care. Med._ 183, 788–824 (2011). Article
PubMed PubMed Central Google Scholar * Raghu, G. et al. An Official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis. an update of the 2011
clinical practice guideline. _Am. J. Respir. Crit. Care. Med._ 192, e3–e19 (2015). Article PubMed Google Scholar * Travis, W. D. et al. An official American Thoracic Society/European
Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. _Am. J. Respir. Crit. Care. Med._ 188, 733–748 (2013).
Article PubMed PubMed Central Google Scholar * Kropski, J. A. et al. Genetic evaluation and testing of patients and families with idiopathic pulmonary fibrosis. _Am. J. Respir. Crit.
Care. Med._ 195, 1423–1428 (2017). Article CAS PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS This work was supported by Research Grant AZV 16–29447 A of
Ministry of Health, Czech Republic and CEITEC 2020 (LQ1601) of Ministry of Education, Youth and Sports. We also acknowledge the CF Genomics CEITEC MU supported by the NCMG research
infrastructure (LM2015091 funded by MEYS CR) for their support in obtaining the scientific data presented in this paper. AUTHOR CONTRIBUTIONS All authors were involved in the data analysis
and interpretation. Moreover, MD, JT, ZV and MD2 were involved in clinical data acquisition and manuscript preparation. All authors reviewed the manuscript and approved the final version for
submission. AUTHOR INFORMATION Author notes * These authors contributed equally: Martina Doubková and Kateřina Staňo Kozubík. AUTHORS AND AFFILIATIONS * Department of Pneumology and
Phtiseology, University Hospital and Faculty of Medicine, Brno, Czech Republic Martina Doubková * Central European Institute of Technology, Masaryk University, Brno, Czech Republic Kateřina
Staňo Kozubík, Lenka Radová, Michaela Pešová, Jakub Trizuljak, Karol Pál, Klára Svobodová, Kamila Réblová, Hana Svozilová, Zuzana Vrzalová, Šárka Pospíšilová & Michael Doubek *
Department of Internal Medicine, Hematology and Oncology, University Hospital and Faculty of Medicine, Brno, Czech Republic Kateřina Staňo Kozubík, Jakub Trizuljak, Hana Svozilová, Zuzana
Vrzalová, Šárka Pospíšilová & Michael Doubek Authors * Martina Doubková View author publications You can also search for this author inPubMed Google Scholar * Kateřina Staňo Kozubík View
author publications You can also search for this author inPubMed Google Scholar * Lenka Radová View author publications You can also search for this author inPubMed Google Scholar *
Michaela Pešová View author publications You can also search for this author inPubMed Google Scholar * Jakub Trizuljak View author publications You can also search for this author inPubMed
Google Scholar * Karol Pál View author publications You can also search for this author inPubMed Google Scholar * Klára Svobodová View author publications You can also search for this author
inPubMed Google Scholar * Kamila Réblová View author publications You can also search for this author inPubMed Google Scholar * Hana Svozilová View author publications You can also search
for this author inPubMed Google Scholar * Zuzana Vrzalová View author publications You can also search for this author inPubMed Google Scholar * Šárka Pospíšilová View author publications
You can also search for this author inPubMed Google Scholar * Michael Doubek View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR
Correspondence to Michael Doubek. ETHICS DECLARATIONS CONFLICT OF INTEREST The authors have received reimbursement from the pharmaceutical industry to cover the costs of participating in
several scientific meetings. ADDITIONAL INFORMATION PUBLISHER’S NOTE: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
SUPPLEMENTARY INFORMATION SUPPLEMENTAL FIGURE LEGEND AND SUPPLEMENTAL TABLE SUPPLEMENTAL FIGURE RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons
Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original
author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the
article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use
is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Doubková, M., Staňo Kozubík, K., Radová, L. _et al._ A novel germline mutation of
the _SFTPA1_ gene in familial interstitial pneumonia. _Hum Genome Var_ 6, 12 (2019). https://doi.org/10.1038/s41439-019-0044-z Download citation * Received: 10 November 2018 * Revised: 03
February 2019 * Accepted: 03 February 2019 * Published: 05 March 2019 * DOI: https://doi.org/10.1038/s41439-019-0044-z SHARE THIS ARTICLE Anyone you share the following link with will be
able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative
