Combined effect of renal function and serum potassium level in sudden cardiac death in aging hypertensive subjects
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT In patients with chronic kidney disease, serum potassium level is a factor influencing sudden cardiac death (SCD). The aim of our analysis was to study the combined effect of serum
potassium level and renal function on the onset of SCD in elderly hypertensive subjects. Data from the 3620 hypertensive patients aged over 70 years were extracted from three randomized
clinical trials included in the INDANA database. During a mean follow up of 4.5 years, 81 patients (2.24%) died from SCD. Mean serum potassium levels and prevalence of chronic kidney disease
were not different in patients who died from SCD. In addition to serum potassium and creatinine levels, 14 clinical and biological variables linked to cardiovascular diseases recorded at
baseline were analyzed using a Bayesian network. The area under the receiver operating characteristic curve of the Bayesian model reached 0.91. Bayesian inference was used to simulate the
combined effects of serum potassium and creatinine levels on SCD. Our analysis, using simulated data from Bayesian model, showed that the estimated probabilities of SCD was significantly
increased in case of hyperkalemia (>5.0 mmol/l) and in case of hypokalemia (<3.5 mmol/l) and in case of chronic kidney disease. Combined effects of serum potassium level and renal
function revealed that chronic kidney disease increased the probability of SCD whatever the serum potassium level. Our results using a Bayesian model confirm the deleterious effects of
hypokalemia, hyperkalemia and chronic kidney disease on SCD in elderly hypertensive patients. You have full access to this article via your institution. Download PDF SIMILAR CONTENT BEING
VIEWED BY OTHERS ASSOCIATION OF POTASSIUM DISORDERS WITH THE MODE OF DEATH AND ETIOLOGY IN PATIENTS WITH CHRONIC HEART FAILURE: THE INCOR-HF STUDY Article Open access 04 December 2024
ALKALINE PHOSPHATASE AFFECTS RENAL FUNCTION IN NEVER-TREATED HYPERTENSIVE PATIENTS: EFFECT MODIFICATION BY AGE Article Open access 17 June 2020 J-SHAPED ASSOCIATION BETWEEN SERUM GLUCOSE
POTASSIUM RATIO AND PROGNOSIS IN HEART FAILURE WITH PRESERVED EJECTION FRACTION WITH STRONGER PREDICTIVE VALUE IN NON-DIABETIC PATIENTS Article Open access 02 December 2024 INTRODUCTION
Sudden cardiac death (SCD) refers to an unexpected death of cardiovascular origin in a patient suffering, or not, from an existing cardiac disorder [1]. In prospective trials, the incidence
of SCD varies between 50 and 100 per 100,000 individuals. Variations in the estimations may be related to the different definitions of SCD used in the trials. Elderly subjects are
particularly at risk since the incidence of SCD reaches 800 per 100,000 individuals [2]. Among the factors related to SCD, some are considered to be contributory factors and others are
considered to be triggering factors [3]. The contributory factors described are: age, male sex, African origin, long QT interval, history of ischemic heart disease, heart failure, excessive
alcohol consumption, sedentary life style and psychosocial factors (anxiety, depression, isolation) [4]. Other factors are considered to be triggers: mornings, Mondays, high temperatures and
intense physical activity. From a pathophysiological viewpoint, intense sympathetic stimulation might be the common triggering factor [5]. In the DUKE’s predictive score of SCD,
specifically established in secondary prevention in patients with documented coronary disease, seven variables that were independently linked to SCD (depressed left ventricular ejection
fraction, number of diseased coronary arteries, diabetes mellitus, hypertension, heart failure, cerebrovascular disease, and tobacco use) are used [6]. Chronic kidney disease (CKD) is a
well-known risk factor of cardiovascular mortality [7] and SCD in the community [8] and in populations with other pathologic conditions [9,10,11,12,13,14,15]. Serum potassium abnormalities
that promote cardiac arrhythmias are also considered risk factors for sudden death [16]. Serum potassium level is controlled by renal function. In patients with CKD, serum potassium level is
a factor influencing SCD even before the dialysis stage. A U-shaped curve has been described and it would appear that hypokalemia is more dangerous than hyperkalemia in renal patients
[17,18,19,20,21]. Thus, the aim of our analysis was to study the combined effect of serum potassium level and renal function on the onset of SCD in elderly subjects whose renal function is
often impaired and among whom there is a higher incidence of SCD. We performed a Bayesian inference analysis using a Bayesian model adjusted to the data extracted from the INdividual Data
ANalysis of Antihypertensive drug intervention trials (INDANA) database, which contains the individual data of hypertensive subjects included in controlled clinical trials. SUBJECTS AND
METHODS SELECTION OF PARTICIPANTS The INDANA database contains the individual data of hypertensive patients, aged 26–96 years with an average follow-up of 4.5 years [22, 23]. None of the
subject was on dialysis. Of the seven studies recorded in the INDANA database, three (SHEP; _n_ = 4736; 4.4 years of follow-up; EWPHE _n_ = 840; 4.7 years of follow-up and COOPE _n_ = 883;
4.5 years of follow-up) recorded baseline serum potassium and creatinine levels. The data of 3620 subjects aged 70 years or more were extracted. The COOPE study compared the effect of atenol
plus bendrofluazide to control, the EWPHE study compared the effects of hydrochlorothiazide plus triamterene to placebo and the SHEP study compared the effects of chlortalidone plus
atenolol or reserpine to placebo in hypertensive patients. VARIABLES OF INTEREST The covariables measured at inclusion in all studies were: age, sex, smoking status (current smoker,
non-smoker), BMI, history of myocardial infarction, history of stroke, history of hypertension, systolic and diastolic blood pressure, heart rate, blood glucose, cholesterolemia, creatinine
level, serum potassium level and plasma uric acid. Serum potassium level was divided into three classes: hypokalemia (_K_ < 3.5 mmol/l), normal serum potassium level (3.5 ≤ _K_ ≤ 5.0
mmol/l), and hyperkalemia (_K_ ≥ 5.0 mmol/l). Renal function was considered to be impaired if creatinine levels were >137 µmol/l in men and >104 µmol/l in women. These cut-off values
were reported to estimate an inulin clearance of less than 60 ml/min/1.73 m²) [24]. As needed to compute probabilities for Bayesian models, continuous variables (age, BMI, systolic and
diastolic blood pressure, heart rate, blood glucose, cholesterolemia, and plasma uric acid) were discretized into five classes of equal frequencies (20% of the sample). In these studies, the
definitions used for sudden death (i.e., death within 1 h of the onset of severe cardiac symptoms, unrelated to other known causes for the SHEP study) were not as precise as those recently
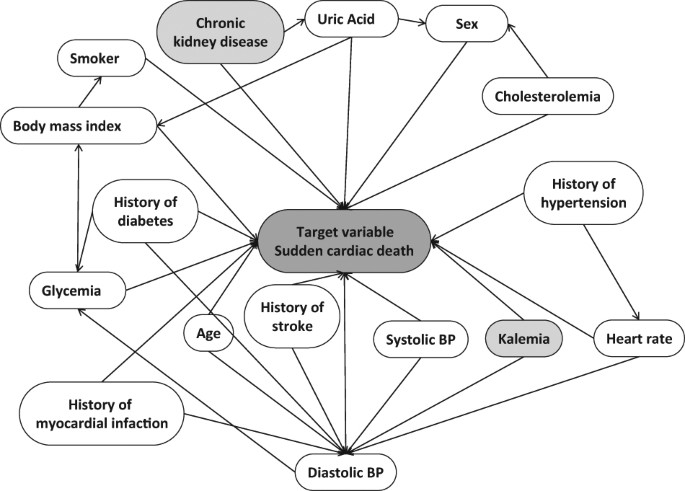
published in the Journal of the American college of cardiology [25]. MODEL STRUCTURE A Bayesian network is a directed graph of a probabilistic structure. It consists of nodes and directed
arrows. Each node is used to represent a variable (and its modalities), and each arrow represents a dependence between variables. Each arrow points from one “parent node” to a “child node”.
The probabilistic dependencies between variables are calculated using the conditional probability as defined by Bayes’ theorem. The tree augmented naïve (TAN) algorithm was used to build the
structure of the Bayesian network. The TAN algorithm uses three rules: (i) each variable is independently linked to the target variable (i.e., CV event); (ii) each variable is also linked
to a unique parent node; (iii) among all possible structures, the structure that maximizes the global mutual information between variables is selected. Thus, conditional probabilities tables
are estimated using the expectation maximization algorithm. The expectation maximization algorithm is an efficient iterative procedure to compute the maximum likelihood estimation in the
presence of missing or hidden data. Network learning was performed on all data files. The software used to create the model was Netica® 5.19; Norsys corporation®. STATISTICS Mean values
between groups (SCD and No SCD) were compared using an analysis of variance (ANOVA) and percentages using _χ_2 tests. The goodness of fit of the model was assessed using the area under the
receiver operating characteristic (ROC) curve. The mutual information of two variables measures their degree of dependence. This mutual information is null when the variables are
independent, and grows when dependence increases. Bayesian inference was performed by superimposing 100% likelihood for each of the three classes of serum potassium level and each of the two
classes of renal function. The probabilities of SCD were obtained for each of the six possible combinations of serum potassium level and renal function. Comparisons of probabilities were
carried out using a _χ_2 test. Interaction of the study treatment on SCD was also analyzed using the Bayesian network. Percentages were compared sing a _χ_2 test. Statistics were performed
using the MedCalc® software version 11.5.1.0. RESULTS During the 4.5 years of follow-up, 81 patients (2.24%) died of SCD. Incidence rate of SCD were similar between cohorts (2.23% for SHEP,
2.0% for EWPHE, and 2.52% for COOPE). The main characteristics of the patients who died from SCD are described in Table 1. Mean serum potassium and prevalence of CKD were not different in
patients who died from SCD (Table 1). The graph in Fig. 1 represents the structure of the model obtained by the TAN algorithm. Figure 2 shows the simplified model obtained using the INDANA
database showing the distribution of modalities of the variables of interest (inputs: serum potassium level and renal function, and output: SCD). The area under the ROC curve of the Bayesian
model for describing SCD was 0.91. In the population, the five variables that were the most linked to SCD are, in descending order: age, history of myocardial infarction, history of
diabetes mellitus, serum potassium level and blood glucose (Table 2). Analyses with simulated data revealed that renal failure increases the probability of SCD (2.83% vs. 2.07%; _p_ <
0.05), that hypokalemia increases the probability of SCD (4.93% vs. 2.16%; _p_ < 0.001) and that hyperkalemia increases the probability of SCD (2.66% vs. 2.16%; _p_ < 0.05). Combined
effects of serum potassium levels and renal function were simulated as shown in Fig. 3. Compared to the probability of SCD with normal serum potassium and normal renal function,
probabilities of SCD were significantly higher in case of hypokalemia and normal renal function (4.54% vs. 2.00%; _p_ < 0.001), hypokalemia and CKD (6.25% vs. 2.00%; _p_ < 0.001),
normal potassium level and CKD (2.73% vs. 2.00%; _p_ < 0.05), and in case of hyperkalemia and CKD (3.35% vs. 2.00%; _p_ < 0.001). Results are presented in Fig. 4. Study treatment did
not influence the incidence of SCD that was 2.10% in the treatment group and 2.37% (NS) in the control group. In the COOPE, EWPHE and SHEP study incidences of SCD were 2.53% vs. 2.52%, 2.17%
vs. 1.82% and 2.03% vs. 2.44% in the treatment and control groups, respectively. DISCUSSION For a long time, serum potassium level has been known to have an effect on cardiac rhythm
disorders and is considered a risk factor of SCD. Serum potassium level is controlled by renal function which is often impaired in elderly subjects. CKD is also a well-known risk factor of
SCD in the community [8] and in populations with coronary artery disease [11,12,13], heart failure [9, 10, 12], end-stage renal disease [14] and in elderly [15]. The originality of our study
is to have analyzed the combined effects of renal function and serum potassium in elderly hypertensive subjects. Our analysis showed that in hypertensive subjects aged over 70 years, serum
potassium level did have an effect on the risk of SCD. Hypokalemia seems to be more harmful than hyperkalemia. CKD tended to increase the risk of SCD irrespective of serum potassium levels
(Fig. 4). These results were obtained by Bayesian inference analysis of data extracted from the INDANA database [23, 24]. The INDANA contains data obtained from well-performed clinical
trials. Nevertheless, only three trials in the INDANA database recorded data for baseline serum potassium and creatinine levels. Given the age of the data in the INDANA database, we did not
calculate glomerular filtration rate (GFR) using a formula (Cockcroft, MDRD or CKD-EPI) to detect the presence of any CKD. CKD (GFR < 60 ml/min/1.73 m²) was estimated however using the
creatinine level thresholds proposed at the time and validated using inulin renal clearances as gold standard [25]. The data being relatively old, we only used baseline data that we have
linked to SCD thus eliminating the effect of treatment (which has never been found connected to SCD in the INDANA database). The goodness of fit of the Bayesian model was confirmed by the
area under the ROC curve of 0.91. We used the TAN Bayes algorithm maximizing the area under the ROC curve and confirming its relevance for modeling biomedical data [26, 27]. In comparison
with a naive architecture where all the variables are considered to be independent of each other when predicting SCD, the TAN algorithm establishes relationships between variables (Fig. 1),
which is much more relevant for biomedical statistics. Our non-parametric approach using Bayesian inference is justified by the complexity of the relationships between variable modalities
and the target variable: SCD. Unlike other statistical methods, Bayesian networks make no hypothesis as to the nature of the relationships between variables. Moreover, in clinical practice,
the measurement of information is “noisy”, even in the best of trials, like those found in the INDANA database, even more so when the observed phenomenon is rare. Indeed, the incidence of
SCD in the population of hypertensive subjects over 70 years of age in the INDANA database is low and is only 2.24% in our study. The definition of SCD in the used studies (death within 1 h
of the onset of severe cardiac symptoms, unrelated to other known causes) that is different from the recently recommended one [25] is a limitation to the interpretation of our results. The
principal limitation of our study is the absence of external validation of our model. However the results of our analysis found the same main risk factors of SCD as described in the
literature. The computation of mutual information on individual data is in accordance with the descriptive statistical analysis (Table 1). Even for subjects over 70 years, age remains the
principal risk factor of SCD. History of myocardial infarction and of type 2 diabetes are the two other principal risk factors of SCD, as well as serum potassium level. In patients with CKD,
serum potassium level is also a risk factor of SCD before the dialysis stage [20]. We found that serum potassium level affects the risk of SCD in elderly hypertensive subjects, and that
hypokalemia tends to be more harmful than hyperkalemia. In the INADANA database, hypokalemia is rarely associated with renal falure and may be due to iatrogenesis (diuretics or potassium
binders). CKD also exacerbated the risk of SCD, irrespective of the serum potassium levels. REFERENCES * Papakadis M, Sharma S. Sudden cardiac death. Card Genet. 2010;38:502–6. Google
Scholar * ACC/AHA/ESC. 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death—executive summary: a report of the American College
of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of
Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) developed in collaboration with the European Heart Rhythm Association and the Heart RhythmSociety.
Circulation. 2006;114:1088–132. Article Google Scholar * Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation. 2012;125:620–37. Article PubMed PubMed Central
Google Scholar * Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res. 2015;116:1887–906. Article PubMed PubMed Central CAS Google
Scholar * Fukuda K, Kanazawa H, Aizawa Y, Ardell JL, Shivkumar K. Cardiac innervation and sudden cardiac death. Circ Res. 2015;116:2005–19. Article PubMed PubMed Central CAS Google
Scholar * Atwater BD, Thompson VP, Vest RN 3rd, Shaw LK, Mazzei WR Jr, Al-Khatib SM, Hranitzky PM, Bahnson TD, Velazquez EJ, Califf RM, Lee KL, Roe MT. Usefulness of the Duke Sudden Cardiac
Death risk score for predicting sudden cardiac death in patients with angiographic (75% narrowing) coronary artery disease. Am J Cardiol. 2009;104:1624–30. Article PubMed Google Scholar
* Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT. Association of estimated glomerular filtration rate and albuminuria with all-cause and
cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–81. Article PubMed PubMed Central Google Scholar * Suzuki T, Agarwal SK, Deo
R, Sotoodehnia N, Grams ME, Selvin E, Calkins H, Rosamond W, Tomaselli G, Coresh J, Matsushita K. Kidney function and sudden cardiac death in the community: The Atherosclerosis Risk in
Communities (ARIC) Study. Am Heart J. 2016;180:46–53. Article PubMed PubMed Central Google Scholar * Hreybe H, Ezzeddine R, Bedi M, Barrington W, Bazaz R, Ganz LI, Jain S, Ngwu O, London
B, Saba S. Renal insufficiency predicts the time to first appropriate defibrillator shock. Am Heart J. 2006;151:852–6. Article PubMed Google Scholar * Goldenberg I, Moss AJ, McNitt S,
Zareba W, Andrews ML, Hall WJ, Greenberg H, Case RB. Relations among renal function, risk of sudden cardiac death, and benefit of the implanted cardiac defibrillator in patients with
ischemic left ventricular dysfunction. Am J Cardiol. 2006;98:485–90. Article PubMed Google Scholar * Deo R, Lin F, Vittinghoff E, Tseng ZH, Hulley SB, Shlipak MG. Kidney dysfunction and
sudden cardiac death among women with coronary heart disease. Hypertension. 2008;51:1578–82. Article PubMed CAS Google Scholar * Saxon LA, Bristow MR, Boehmer J, Krueger S, Kass DA, De
Marco T, Carson P, DiCarlo L, Feldman AM, Galle E, Ecklund F. Predictors of sudden cardiac death and appropriate shock in the Comparison of Medical Therapy, Pacing, and Defibrillation in
Heart Failure (COMPANION) Trial. Circulation. 2006;114:2766–72. Article PubMed Google Scholar * Pun PH, Smarz TR, Honeycutt EF, Shaw LK, Al-Khatib SM, Middleton JP. Chronic kidney disease
is associated with increased risk of sudden cardiac death among patients with coronary artery disease. Kidney Int. 2009;76:652–8. Article PubMed PubMed Central Google Scholar * Green D,
Roberts PR, New DI, Kalra PA. Sudden cardiac death in hemodialysis patients: an in-depth review. Am J Kidney Dis Off J Natl Kidney Found. 2011;57:921–9. Article Google Scholar * Deo R,
Sotoodehnia N, Katz R, Sarnak MJ, Fried LF, Chonchol M, Kestenbaum B, Psaty BM, Siscovick DS, Shlipak MG. Cystatin C and sudden cardiac death risk in the elderly. Circ Cardiovasc Qual
Outcomes. 2010;3:159–64. Article PubMed PubMed Central Google Scholar * Helfant RH. Short- and long-term mechanisms of sudden cardiac death in congestive heart failure. Am J Cardiol.
1990;65:41K–43K. Article PubMed CAS Google Scholar * Korgaonkar S, Tilea A, Gillespie BW, Kiser M, Eisele G, Finkelstein F, Kotanko P, Pitt B, Saran R. Serum potassium and outcomes in
CKD: insights from the RRI-CKD cohort study. Clin J Am Soc Nephrol. 2010;5:762–9. Article PubMed PubMed Central CAS Google Scholar * Hayes J, Kalantar-Zadeh K, Lu JL, Turban S, Anderson
JE, Kovesdy CP. Association of hypo- and hyperkalemia with disease progression and mortality in males with chronic kidney disease: the role of race. Nephron Clin Pract. 2012;120:c8–16.
Article PubMed CAS Google Scholar * Lafrance JP, Nolin L, Senécal L, Leblanc M. Predictors and outcome of cardiopulmonary resuscitation calls in a large haemodialysis unit over a
seven-year period. Nephrol Dial Transplant. 2006;21:1006–12. Article PubMed Google Scholar * Luo J, Brunelli SM, Jensen DE, Yang A. Association between serum potassium and outcomes in
patients with reduced kidney function. Clin J Am Soc Nephrol. 2016;11:90–100. Article PubMed CAS Google Scholar * Bowling CB, Pitt B, Ahmed MI, Aban IB, Sanders PW, Mujib M, Campbell RC,
Love TE, Aronow WS, Allman RM, Bakris GL, Ahmed A. Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: Findings from propensity-matched studies. Circ
Heart Fail. 2010;3:253–60. Article PubMed PubMed Central Google Scholar * Kassaï B, Boissel JP, Cucherat M, Boutitie F, Gueyffier F. Treatment of high blood pressure and gain in
event-free life expectancy. Vasc Health Risk Manag. 2005;1:163–9. Article PubMed PubMed Central Google Scholar * Gueyffier F, Boutitie F, Boissel JP, Coope J, Cutler J, Ekbom T, Fagard
R, Friedman L, Perry HM, Pocock S. INDANA: a meta-analysis on individual patient data in hypertension. Protocol and preliminary results. Therapie. 1995;50:353–62. PubMed CAS Google Scholar
* Couchoud C, Pozet N, Labeeuw M, Pouteil-Noble C. Screening early renal failure: cut-off values for serum creatinine as an indicator of renal impairment. Kidney Int. 1999;55:1878–84.
Article PubMed CAS Google Scholar * Hicks KA, Tcheng JE, Bozkurt B, Chaitman BR, Cutlip DE, Farb A, Fonarow GC, Jacobs JP, Jaff MR, Lichtman JH, Limacher MC, Mahaffey KW, Mehran R,
Nissen SE, Smith EE, Targum SL. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American
Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol. 2015;66:403–69. Article PubMed Google
Scholar * Friedman N, Geiger D, Goldszmidt M. Bayesian network classifiers. Mach Learn. 1997;29:131–63. Article Google Scholar * Sansot C, Kalbacher E, Lemoine S, Bourguignon L, Fauvel
JP, Ducher M. A Bayesian Model to describe factors influencing trough levels of vancomycin in hemodialysis patients. Nephron. 2015;131:131–7. Article PubMed CAS Google Scholar Download
references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Hospices Civils de Lyon-Université C Bernard Lyon 1, Lyon, France Jean-Pierre Fauvel * Service de pharmacologie clinique et essais
thérapeutiques Hospices Civils de Lyon, UMR5558 - Evaluation et Modélisation des Effets des Médicaments, Lyon, France Francois Gueyffier * Studies Coordinating Centre, Research Unit
Hypertension and Cardiovascular Epidemiology, KU Leuven Department of Cardiovascular Sciences, University of Leuven, Leuven, Belgium Lutgarde Thijs * Pharmacie, Hospices Civils de Lyon-
EMR3738 Ciblage thérapeutique en oncologie, Université C Bernard Lyon 1, Lyon, France Michel Ducher Authors * Jean-Pierre Fauvel View author publications You can also search for this author
inPubMed Google Scholar * Francois Gueyffier View author publications You can also search for this author inPubMed Google Scholar * Lutgarde Thijs View author publications You can also
search for this author inPubMed Google Scholar * Michel Ducher View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to
Jean-Pierre Fauvel. ETHICS DECLARATIONS CONFLICT OF INTEREST The authors declare that they have no conflict of interest. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE
CITE THIS ARTICLE Fauvel, JP., Gueyffier, F., Thijs, L. _et al._ Combined effect of renal function and serum potassium level in sudden cardiac death in aging hypertensive subjects.
_Hypertens Res_ 41, 469–474 (2018). https://doi.org/10.1038/s41440-018-0035-3 Download citation * Received: 12 April 2017 * Revised: 15 November 2017 * Accepted: 27 November 2017 *
Published: 09 April 2018 * Issue Date: June 2018 * DOI: https://doi.org/10.1038/s41440-018-0035-3 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this
content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
