Blockade of vegf-c signaling inhibits lymphatic malformations driven by oncogenic pik3ca mutation
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT Lymphatic malformations (LMs) are debilitating vascular anomalies presenting with large cysts (macrocystic) or lesions that infiltrate tissues (microcystic). Cellular mechanisms
underlying LM pathology are poorly understood. Here we show that the somatic _PIK3CA__H1047R_ mutation, resulting in constitutive activation of the p110α PI3K, underlies both macrocystic and
microcystic LMs in human. Using a mouse model of _PIK3CA__H1047R_-driven LM, we demonstrate that both types of malformations arise due to lymphatic endothelial cell (LEC)-autonomous
defects, with the developmental timing of p110α activation determining the LM subtype. In the postnatal vasculature, _PIK3CA__H1047R_ promotes LEC migration and lymphatic hypersprouting,
leading to microcystic LMs that grow progressively in a vascular endothelial growth factor C (VEGF-C)-dependent manner. Combined inhibition of VEGF-C and the PI3K downstream target mTOR
using Rapamycin, but neither treatment alone, promotes regression of lesions. The best therapeutic outcome for LM is thus achieved by co-inhibition of the upstream VEGF-C/VEGFR3 and the
downstream PI3K/mTOR pathways. SIMILAR CONTENT BEING VIEWED BY OTHERS AUTOPHAGY INHIBITION PREVENTS LYMPHATIC MALFORMATION PROGRESSION TO LYMPHANGIOSARCOMA BY DECREASING OSTEOPONTIN AND
STAT3 SIGNALING Article Open access 22 February 2023 THE RNA HELICASE DDX21 CONTROLS VEGFC-DRIVEN DEVELOPMENTAL LYMPHANGIOGENESIS BY BALANCING ENDOTHELIAL CELL RIBOSOME BIOGENESIS AND P53
FUNCTION Article 08 November 2021 ANGIOPOIETIN–TIE2 FEEDFORWARD CIRCUIT PROMOTES PIK3CA-DRIVEN VENOUS MALFORMATIONS Article Open access 23 May 2025 INTRODUCTION Vascular malformations are
chronic, often congenital pathologies that can manifest in different types of blood and lymphatic vessels. These diseases commonly arise from abnormalities in the endothelial cells (ECs) of
the affected vessel type(s) that lead to structural and functional vascular defects causing deformation, pain, morbidity, and organ dysfunction1. Genome sequencing efforts have identified
causative mutations for different types of malformations and opened up possibilities for therapeutic intervention specifically targeting the aberrant signal transduction pathways2,3. Somatic
activating mutations in the _PIK3CA_ gene, encoding the p110α catalytic subunit of phosphatidylinositol 3-kinase (PI3K), were identified as causative of ~20% of venous malformations
(VM)4,5,6, and the majority of lymphatic malformations (LM)7,8. The most common VM/LM mutations affecting the helical domain (E542K, E545K) or the kinase domain (H1047R, H1047L) of p110α are
identical to those previously found in cancer and other genetic syndromes characterized by tissue overgrowth9. Both types of mutations result in basal activation of the PI3K pathway by
enhancing dynamic events in the natural activation of p110α that lead to increased lipid binding10. The PI3K lipid kinases control a variety of cellular functions and developmental and
homeostatic processes in response to extracellular signals by regulating the plasma membrane phorphatidylinositol (3,4,5)-triphosphate (PIP3) levels11. Of the four p110 isoforms, the
ubiquitously expressed p110α has emerged as the key downstream effector of growth factor receptor signaling in most cell types and in particular in the endothelium. Genetic loss-of-function
studies in mice demonstrated an important role of p110α in the development of both blood and lymphatic vessels12,13,14. Conversely, conditional expression of the _PIK3CA_-activating mutation
in endothelial cells led to vascular overgrowth and malformations in mice4,5,15,16. Identification of _PIK3CA_ mutations as drivers of vascular malformations has opened up a possibility for
the therapeutic use of PI3K inhibitors in these diseases. Rapamycin and its analogues (sirolimus, everolimus) that target the PI3K downstream effector mTOR can stop the progression of
vascular malformations in mice and human, and improve the patients’ quality of life3,5,15,16,17,18,19. However, regression of lesions is observed only in a minority of patients3, which calls
for a need to develop new more effective therapies. Compared with the malformations affecting the blood vasculature, LMs have received less attention despite often severe complications for
patients. LMs are characterized by large fluid-filled cysts (macrocystic LM), or diffuse, infiltrative lesions sometimes consisting of small vesicles containing lymph or blood (microcystic
LM)19,20. Many patients show a mixed phenotype with a combination of large and small cysts. Lesion growth may be progressive and, depending on the location, result in severe complications
such as infections and impairment of breathing or swallowing. Macrocystic LM can be usually effectively treated with sclerotherapy or surgical resection. By contrast, the treatment of
microcystic LM is challenging due to their infiltrative growth, and curative therapies are currently lacking. Here we studied the pathophysiological mechanisms of _PIK3CA_-driven LM. We show
that both macrocystic LM and microcystic LM are driven by the activating _PIK3CA__H1047R_ mutation, with the developmental timing of activation of the p110α PI3K signaling in lymphatic
endothelia determining the LM subtype. We further show that the growth of _PIK3CA__H1047R_-driven microcystic LM in mice is dependent on the upstream lymphangiogenic vascular endothelial
growth factor C (VEGF-C)/VEGFR3 signaling. Combined inhibition of VEGF-C signaling and the PI3K downstream target mTOR using Rapamycin, but neither treatment alone, promotes the regression
of experimental LM in mice. Our findings provide important implications for the treatment of microcystic LM in human and suggest that therapies targeting the key upstream pathway in
combination with PI3K pathway inhibition may be relevant for other _PIK3CA_-driven pathologies. RESULTS _PIK3CA_ _H1047R_ MUTATION UNDERLIES MICRO- AND MACROCYSTIC LMS To address whether the
two subtypes of LM require different _PIK3CA_ mutations, potentially driving different cellular responses, or if the same mutation can underlie both microcystic and macrocystic LMs, we
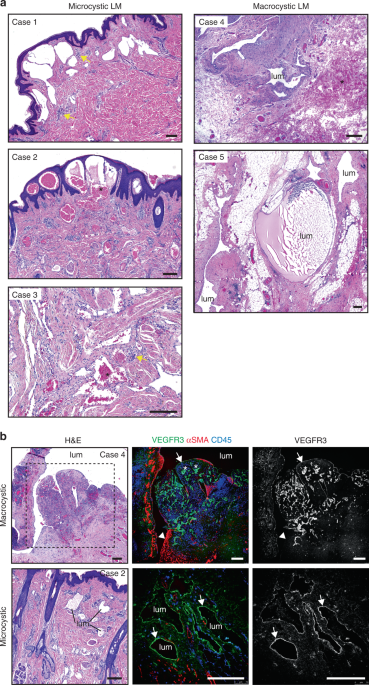
focused on patients with a somatic _PIK3CA__H1047R_ mutation. Clinical features of five patients selected for the study are summarized in Table 1. Histologic features of the lesions were
investigated using tissue sections from the patients to confirm lymphatic identity of the lesions and the LM subtype (Fig. 1a, b, Supplementary Fig. 1a). Lesions from two patients with
macrocystic LM were characterized by convoluted structures with large lumens, which in some cases contained lymph, lymphocytes and/or red blood cells (RBCs) (Fig. 1a). The endothelium lining
the cystic lumens was positive for PDPN and PROX1 (Supplementary Fig. 1a), confirming lymphatic endothelial identity. LYVE1 (Supplementary Fig. 1a) and VEGFR3 (Fig. 1b, Supplementary Fig.
1b) staining was weak or lacking in the largest cysts, in particular in areas surrounded by αSMA+ smooth muscle cells. High VEGFR3 expression was instead observed in small-caliber lymphatic
vessels in areas within the cyst wall containing infiltrated CD45+ cells (Fig. 1b). Microcystic LMs were characterized by smaller cysts and vessels with irregular lumens and no smooth muscle
cell layer (Fig. 1b). The endothelium of microcystic LMs was positive for VEGFR3 (Fig. 1b), PDPN and PROX1 (Supplementary Fig. 1a). LYVE1 staining was patchy, similarly as in macrocystic
LMs (Supplementary Fig. 1a). Similar to the macrocystic LM, and in agreement with previous reports21, a large number of CD45+ cells (Fig. 1b) and presence of lymphoid aggregates
(Supplementary Fig. 1c) were also observed in all three microcystic LMs. These data show that the two distinct LM subtypes showing different morphological and molecular features result from
the same somatic mutation in _PIK3CA_. DEVELOPMENTAL TIMING OF PI3K ACTIVATION DETERMINES LM SUBTYPE To investigate if both macrocystic and microcystic _PIK3CA_-driven LMs are caused by
lymphatic endothelial cell (LEC)-autonomous defects, we generated a mouse model that allows inducible LEC-specific activation of the causative mutation _PIK3CA__H1047R_. Mice carrying a
knock-in _PIK3CA__H1047R_ allele in the _Rosa26_ locus, silenced by a lox-stop-lox cassette until Cre exposure22, were crossed with the _Vegfr3_-_CreER__T2_ mice expressing
tamoxifen-inducible Cre recombinase specifically in lymphatic endothelia23 (Fig. 2a). Since LMs are often present at birth, we first induced activation of _PIK3CA__H1047R_ expression at the
early stage of lymphatic development by administering 4-hydroxytamoxifen (4-OHT) to pregnant females at embryonic day (E)11 (Fig. 2a). Whole-mount immunofluorescence of the skin of embryos
at E17 revealed two types of lesions in the lymphatic vasculature. The majority of lesions appeared as large isolated cysts that were localized mainly to the cervical, and less frequently to
the sacral region of the skin (Fig. 2b, c, Supplementary Fig. 2a, b). In addition, areas of lymphatic vessel hypersprouting were observed in the thoracic region of the skin (Fig. 2b).
Lymphatic endothelium showed normal identity and expression of LEC markers including PROX1 (Fig. 2b, Supplementary Fig. 2b). Histological examination of the skin revealed that the cysts
consisted of a single lumen (Fig. 2d) that frequently contained RBCs (Supplementary Fig. 2b, c). The morphological features of the lesions and their predominant localization to the neck
region of the skin were thus reminiscent of human macrocystic LM. Next, we induced activation of _PIK3CA__H1047R_ expression in LECs during late embryonic (Supplementary Fig. 2a) or early
postnatal development (Fig. 2a). Administration of 4-OHT to pregnant females at E14 led to increased lymphatic vessel branching in all regions of the dorsal skin of E17
_PIK3CA__H1047R_;_Vegfr3_-_CreER__T2_ embryos, but no macrocystic lesions were observed (_n_ = 6 embryos) (Supplementary Fig. 2d, e). Similarly, analysis of the vasculature in the ear skin
of neonatally induced mice revealed well-defined malformations that were characterized by a dense network of hyperbranched lymphatic vessels (Fig. 2e). These lesions further developed into
large sheet-like vascular structures that frequently showed bleeding in the lesion area (Fig. 2e). A similar lymphatic hypersprouting phenotype was observed using another LEC-specific Cre
line, the _Prox1_-_CreER__T2_24 (Supplementary Fig. 3a–c). Histological examination of the lesions in the _PIK3CA__H1047R_;_Prox1_-_CreER__T2_ ear showed multiple lumens (Fig. 2f) and
presence of RBCs both inside and outside of the lymphatic vessels (Supplementary Fig. 3d), reminiscent of microcystic LMs in human patients (Fig. 1b). In summary, these results demonstrate
that developmental timing of activation of the p110α signaling in LECs determines the LM subtype. Early embryonic activation leads predominantly to formation of lesions that recapitulate
features of human macrocystic LM, whereas activation during late embryonic or neonatal development results in microcystic LM (Supplementary Table 1). Our data further suggest that the
physical location of the lesion also impacts on their characteristics, with most macrocystic lesions developing in the cervical region of the skin. _PIK3CA_ _H1047R_ EXPRESSION CONFERS
MIGRATORY PHENOTYPE IN LECS We focused our investigation on microcystic LMs that are difficult to treat due to their infiltrative pattern of growth. To allow analysis of the early steps of
microcystic LM development, we analyzed the acute response of postnatal ear vasculature of _PIK3CA__H1047R__;Vegfr3-CreER__T2_ mice 10 days after neonatal 4-OHT administration (Fig. 3a). We
observed formation of new vessels showing a typical ‘spiky’ appearance of active vessel sprouts (Fig. 3b). Quantification of vessel ends and their morphology demonstrated blunted morphology
of most lymphatic capillaries and only a few active sprouts in the ear skin of 3-week-old mice (Fig. 3b), in agreement with previous observations25. _PIK3CA_ mutant vasculature showed an
increase in the number of vessel ends, the majority of which had the spiky morphology of active sprouts (Fig. 3b). Staining for phosho-S6 as a readout of PI3K activity26 revealed signal
selectively in active lymphatic sprouts in the mutant vasculature, similar to lymphangiogenic sprouts of embryonic vessels (Fig. 3c). LECs within the active sprouts also displayed straight
zipper-like cell-cell junctions, a hallmark of lymphangiogenic vessels27, as opposed to oak-leaf shaped LECs of normal capillaries that possess button-like junctions (Fig. 3d). To study more
advanced lesions, we utilized models permitting robust and reproducible induction of localized vs. generalized _PIK3CA__H1047R_-driven response in the postnatal ear skin using the
_Prox1_-_CreER__T2_ and _Vegfr3_-_CreER__T2_ models. Topical application of a low dose of 4-OHT (0.5-2 µg) into one ear of a _PIK3CA__H1047R_;_Prox1_-_CreER__T2_ mouse induced locally
restricted Cre recombination and lesions in the treated ear (Supplementary Fig. 3a, b). A similar sprouting response and progression of lesions was observed as previously seen in the
_Vegfr3_-_CreER__T2_ model (Supplementary Fig. 3c, d). In contrast, topical administration of a higher dose of 4-OHT (100 µg) into one ear of a _Vegfr3-CreER__T2_ mouse led to systemic
Cre-mediated recombination (Supplementary Fig. 4a, b), resulting in a generalized _PIK3CA__H1047R_-driven sprouting response of the entire dermal lymphatic vasculature (Supplementary Fig.
4c, d). Progressive increase in lymphatic vessel hyperbranching (Supplementary Fig. 4e) was associated with increase in the number of active sprouts (Supplementary Fig. 4f), as well as in
LEC proliferation (Supplementary Fig. 4g) and numbers (Supplementary Fig. 4h). To characterize the LEC phenotype associated with p110α activation, we isolated primary dermal LECs from the
_PIK3CA__H1047R__;Vegfr3-CreER__T2_ mice by sequential selection of PECAM1+ ECs and LYVE1+ LECs, as previously described23. Staining for VE-cadherin and PROX1 demonstrated high purity of the
isolated LEC population (Supplementary Fig. 5a). _PIK3CA__H1047R_ -expressing LECs, treated in vitro with 4-OHT, showed reorganization of cell-cell junctions and cytoskeleton characterized
by increase in serrated junctions with VE-cadherin fingers, and increased actin stress fiber formation compared with untreated controls (Fig. 3e). Such changes in junctional morphology have
previously been linked to active EC migration and vessel sprouting28,29,30. To test if the observed morphological changes correlated with increased migratory behavior, we exposed
_PIK3CA__H1047R_ -expressing and control LECs to scratch wound assay. Live imaging of scratch wounded cell monolayers showed enhanced wound closure of 4-OHT-treated LECs expressing the
constitutive active p110α compared with vehicle-treated control LECs (Fig. 3f). No further increase in the speed of wound closure in the _PIK3CA__H1047R_-expressing primary LECs was observed
in the presence of the specific lymphangiogenic growth factor VEGF-C (Supplementary Fig. 5b), suggesting that the change in the cellular phenotype represents a cell-autonomous effect of
oncogenic PI3K activity on the LEC. Together, these results demonstrate that p110α activation confers a migratory LEC phenotype and induces lymphatic vessel sprouting that leads to the
hyperbranched network of vessels defining LM lesions. VEGF-C INDUCES HYPERACTIVATION OF AKT IN _PIK3CA_ _H1047R_-LECS Next, we studied the effect of p110α activation on downstream signaling
in LECs. 4-OHT-induced expression of the constitutive active p110α in primary LECs isolated from the _PIK3CA__H1047R__;Vegfr3-CreER__T2_ mice led to increased Akt activation under basal
growth conditions in both sparse and confluent cells (Fig. 3g). To assess the response to growth factor activation, serum starved LECs were stimulated with VEGF-C, the major regulator of LEC
migration31. As expected, serum starved 4-OHT treated _PIK3CA__H1047R_ -expressing LECs showed again increased Akt phosphorylation compared with vehicle-treated cells in the absence of
growth factor simulation (Fig. 3h, i). VEGF-C stimulation induced a comparable increase in Akt phosphorylation in control LECs. _PIK3CA__H1047R_ -expressing LECs however showed a further
increase in Akt activity in response to VEGF-C (Fig. 3h, i). Taken together, VEGF-C stimulation induces hyperactivation of Akt in _PIK3CA__H1047R_ -expressing LECs. This is in agreement with
previous studies in cancer cells showing that the _H1047R_ mutation residing in the kinase domain of p110α relies on upstream receptor tyrosine kinase (RTK) stimulation to reach a critical
threshold of membrane binding and activity needed for transformation32. _PIK3CA_ _H1047R_-DRIVEN LM IS DEPENDENT ON VEGF-C SIGNALING To investigate the potential involvement of VEGF-C
signaling in LM pathology in vivo, we analyzed expression of the pathway components in mouse LM lesions in comparison to normal vasculature. The VEGF-C receptors VEGFR3 and NRP2, but not
VEGFR2, were strongly upregulated in the abnormal sprouts in the _PIK3CA__H1047R__;Vegfr3-CreER__T2_ ears (Fig. 4a, b, Supplementary Fig. 6a). Increase in VEGFR3, which correlated with
increase in lymphatic vessel branching, was also observed in a knock-in mouse model33, where _Pik3ca__H1047R_ expression is driven by the endogenous promoter after Cre recombination
(Supplementary Fig. 6a–c), as well as in the localized lesions in the _PIK3CA__H1047R__;Prox1-CreER__T2_ mice (Supplementary Fig. 6d). We could not, however, detect a significant increase in
VEGFR3 mRNA or protein levels in primary _PIK3CA__H1047R_ -expressing LECs (Supplementary Fig. 6e, f), suggesting that upregulation observed in vivo is not due to direct regulation by PI3K.
As seen in human patients, we observed an accumulation of immune cells around advanced lesions in the _PIK3CA__H1047R__;Prox1-CreER__T2_ mice (Fig. 4c). In agreement with this, analysis of
ears in the model of progressive microcystic LM showed a modest increase in the number of macrophages (Fig. 4d), that are the major source of VEGF-C34,35. These results suggest increased
VEGF-C signaling in LM, which may critically contribute to driving pathological vessel growth. Next, we analyzed the response of _PIK3CA_-driven vascular malformations to inhibition of
VEGF-C signaling in vivo. For this purpose, we used the model of progressive microcystic LM in postnatal mice (Supplementary Fig. 4e). To achieve continuous inhibition of the VEGF-C pathway,
we used adeno-associated vectors (AAVs) encoding the soluble VEGF-C-trap (AAV-VEGFR3[1-4]-Ig36). Control mice were treated either with PBS or AAVs encoding the non-ligand binding region of
the VEGFR3 extracellular domain (AAV-VEGFR3[4-7]-Ig). Soluble VEGFR31-4-Ig protein was detected in the serum 3 weeks after intraperitoneal AAV administration at a concentration of 121 ± 30
ng µl−1 (_n_ = 5) (Supplementary Fig. 7a). In agreement with previous studies37, this was sufficient to block VEGF-C-induced lymphangiogenesis in the ear skin (Supplementary Fig. 7b).
Administration of AAVs to _PIK3CA__H1047R__;Vegfr3-CreER__T2_ mice one week after induction of lymphatic overgrowth (Supplementary Fig. 4e, Fig. 4e) led to an efficient inhibition of the
growth of LM (Fig. 4f, g). As previously reported38, VEGF-C inhibition did not affect mature vasculature in control mice (Fig. 4f). VEGF-C inhibition specifically affected the growth of
lymphatic lesions, as it did not have an effect on the growth of lesions within the blood vasculature in _PIK3CA__H1047R__;Cdh5-CreER__T2_ mice that express the constitutive active p110α in
all ECs (Supplementary Fig. 8a–d). CO-INHIBITION OF VEGF-C AND MTOR PROMOTES LM REGRESSION Rapamycin (also known as sirolimus) is an allosteric inhibitor of the PI3K downstream target mTOR
that has been used in the treatment of patients with vascular malformations including both VM and LM3. To avoid body weight loss associated with treatment with a high dose of Rapamycin39,
mice were administered with daily intraperitoneal injections of 10 mg kg−1 of Rapamycin during 5 consecutive days. As expected, Rapamycin inhibited the overgrowth of both blood and lymphatic
vessels in the _PIK3CA__H1047R__;Cdh5-CreER__T2_ mice when administered at the time of 4-OHT-mediated induction of _PIK3CA__H1047R_ expression (Supplementary Fig. 9a–c). In addition, it
significantly reduced vessel growth and hyperbranching when administered one week after induction of vascular overgrowth (Supplementary Fig. 9d–f). To test the therapeutic effect on more
advanced lesions, we initiated Rapamycin treatment two weeks after induction of vascular overgrowth in the _PIK3CA__H1047R__;Vegfr3-CreER__T2_ model of progressive microcystic LM (Fig. 5a).
Analysis of the vasculature after 1.5 weeks of Rapamycin treatment, administered every second day, showed only a modest inhibition of vascular growth during the treatment period, and no
regression (Fig. 5b, c). Treatment with the VEGF-C trap also inhibited the growth but did not promote regression of the lymphatic vasculature (Fig. 5b, c). However, combined treatment with
the VEGF-C trap and Rapamycin showed an additive effect and promoted regression of the vasculature (Fig. 5b, c), and effectively blocked LEC proliferation (Fig. 5d). Remaining areas of
hyperbranched vasculature in mice treated with both the VEGF-C trap and Rapamycin frequently showed blunted morphology of vessel sprouts, compared with spiky appearance characteristic of
active sprouting process in vehicle-treated mice (Fig. 5e, f). DISCUSSION LM are vascular anomalies presenting with large fluid-filled cysts (macrocystic) or lesions that infiltrate tissues
(microcystic) and cause morbidity, pain and organ dysfunction. Using a mouse model of LM driven by an activating _PIK3CA_ mutation, we here characterize molecular and cellular mechanisms of
lymphatic lesion formation and therapy response. Notably, we show that the progressive growth of _PIK3CA__H1047R_-driven microcystic LM is dependent on the upstream lymphangiogenic
VEGF-C/VEGFR3 signaling, which permits a novel effective therapeutic intervention to treat LM. Here we focused on the common activating _PIK3CA_ mutation _H1047R_ causative of both VM and
LM5,6,7, but also cancer and overgrowth syndromes9. We found that the H1047R mutation is causative of both macrocystic and microcystic LM in a LEC-autonomous manner, with the developmental
timing of _PIK3CA_ activation determining the LM subtype. In mouse skin, embryonic LEC-specific activation of _PIK3CA_ led to macrocystic lesions characterized by large cysts localized
predominantly to the neck region of the skin, similarly as in human LM patients. In contrast, late embryonic or early postnatal activation caused microcystic malformations with hyperbranched
lymphatic lesions. Why activation of the same signaling pathway can cause different LEC responses leading to morphologically different types of malformations remains to be studied. It is
possible that the cellular response may differ depending on the developmental origin and differentiation status40 (progenitor vs. lining a lumenized vessel) as well as the cellular state
(proliferating vs. quiescent). Differences in the tissue environment may also play a role. For example, tissue stiffness and composition of the immune cells that are both known to regulate
LEC responses and lymphangiogenesis34,41,42 differ between embryonic and postnatal skin. The development of several types of vascular malformations, including cerebral cavernous
malformations (CCM) and arteriovenous malformations (AVM) require active angiogenesis. The formation of these vascular lesions can be efficiently induced experimentally in mice during
developmental vascular growth, but require reactivation of quiescent endothelium at adult stages43,44,45,46,47. The congenital nature of LM in human suggests that lymphatic endothelium is
similarly sensitive to activation of p110α signaling during the active growth of the vasculature, yet lesions may also appear later in life and show progressive growth. Using the mouse model
of _PIK3CA__H1047R_-driven LM, we found that, as expected, both embryonic and early postnatal lymphatic vasculature is responsive to p110α activation, leading to formation of localized
vascular lesions. However, LEC-specific activation of _PIK3CA__H1047R_ expression at 3 weeks of age led to a generalized, rather than localized response characterized by progressive
lymphatic vascular hyperplasia. This is in agreement with a previous study modeling generalized lymphatic anomaly (GLA) in mice upon LEC-specific induction of _PIK3CA__H1047R_ at 4 weeks of
age16. The exquisite sensitivity of quiescent lymphatic endothelium to p110α activation may be related to the requirement of inhibition of the pathway for the maintenance of endothelial
quiescence48. This finding raises the question of why _PIK3CA_-driven lymphatic vascular overgrowth is not a frequent manifestation in adult vasculature. It is possible that a critical
threshold of mutant cells needed to cause vascular overgrowth is efficiently induced in our experimental model, but is not achieved in quiescent endothelium hit by a single somatic mutation.
It is also possible that endothelial cells that acquire _PIK3CA_ mutation require a permissive local environment to engage in signaling with normal neighbors that allow them to collectively
drive pathological vascular growth. Clonal co-operation in vascular malformations, a concept that is well-established in cancer49, may be supported by the observation that only a small
proportion of endothelial cells forming CCM lesions in human carry a mutation50,51. In addition, in a mouse model of CCM, initial clonal expansion of _Ccm3_ deficient cells was followed by
incorporation and phenotypic change of normal cells driving further growth of the lesion52,53. Of interest, heterogeneity between neighboring LECs in the level of VEGFR3, which is regulated
by PI3K/mTOR signaling (our study and39,54), was shown to non-cell-autonomously drive pathological vessel hyperplasia through cell contact-dependent regulation of Notch signaling55.
Longitudinal magnetic resonance imaging of the LM lesions could provide important insights into the mechanisms of LM growth. Macrocystic LM can be generally effectively treated with
sclerotherapy or surgical resection. The treatment of microcystic LM is more challenging due to the infiltrative growth of the lesions. Ongoing clinical trials assessing the efficacy of
Sirolimus (mTOR inhibitor Rapamycin) for the treatment of _PIK3CA_-driven vascular malformations have shown promising results. Sirolimus efficiently stops the growth of vascular
malformations in mice and human, and improves the patients’ quality of life3,5,15,16,17,18,19. However, regression of the lesion is achieved only in rare cases3. It is also currently unclear
if patients need life-long treatment, which is associated with a risk of side effects of the drug. Consistent with the clinical data and previous studies on a mouse model of _PIK3CA_-driven
generalized lymphatic anomaly16, we found that Rapamycin inhibited lymphatic vascular growth in the experimental model of _PIK3CA__H1047R_-driven microcystic LM. The treatment resulted in
an efficient inhibition of the initial growth and expansion of early lesions, but only a modest inhibition, and no regression, could be observed in more advanced lesions. Interestingly, in a
mouse model of VEGF-C induced pulmonary lymphangiectasia, which persisted even after normalization of VEGF-C levels, Rapamycin treatment effectively promoted regression of abnormal
lymphatic vessels without affecting normal vessels39. However, a significant reversal of lymphangiectasia required a high dose (20 mg kg−1 daily) of Rapamycin that was associated with body
weight loss39. Although compatible with survival of adult mice39, high dose of Rapamycin could not be tolerated during neonatal period of growth. It may thus not be feasible to use a high
enough dose of Rapamycin required for induction of lymphatic vessel regression in children and young adolescents. Interestingly, Alpelisib (BYL719), a specific _PIK3CA_ inhibitor, has shown
a higher efficacy than Rapamycin in the treatment of _PIK3CA_-related overgrowth syndromes (PROS) in mice and humans56. Alpelisib improved organ abnormalities and dysfunction, also in the
vasculature, with minimal side effects. Future studies should address the efficacy of Alpelisib in patients with LM. In addition to the cell-autonomous migration-promoting effect of p110α on
LECs observed in vitro, lymphangiogenic VEGF-C/VEGFR3 signaling in the LM lesion was found to significantly contribute to the further vascular growth of the lesions in vivo. Strong
upregulation of the VEGF-C receptors VEGFR3 and NRP2 was observed in the lymphangiogenic sprouts, consistent with previous observations in LM patients57,58. In addition, we observed
increased infiltration of immune cells, including macrophages, which are an important source of pro-lymphangiogenic growth factors such as VEGF-C34,35. Although LECs expressing the oncogenic
p110α showed increased Akt activity already under basal conditions, VEGF-C stimulation led to hyperactivation of the pathway. These findings suggest a positive feedback reinforcing the
upstream pathway that subsequently promotes abnormally high activity of the downstream signaling, making the pathway a potential target for therapeutic intervention. Indeed, we found that
inhibition of VEGF-C/VEGFR3 signaling using the soluble VEGF-C trap inhibited LM lesion growth in vivo. Notably, treatment with the soluble VEGF-C trap was more effective than Rapamycin in
inhibiting LM growth, and when administered in combination with Rapamycin it was able to promote lymphatic vessel regression. Our results suggest that, like in cancer, optimal therapeutic
benefit may require targeting both the endothelial cell-autonomous _PIK3CA_-driven signaling and the microenvironment-derived paracrine signaling that contribute to driving pathological
vessel growth. The relative contributions of the two mechanisms may be different at different stages of lesion formation, which can affect response to therapy. It is possible that the
beneficial effect of Rapamycin is partly due to its immunosuppressive functions, although this should be addressed in future studies. In conclusion, we show that the progressive growth of
_PIK3CA__H1047R_-driven microcystic LM is dependent on the upstream lymphangiogenic VEGF-C/VEGFR3 signaling. Combined inhibition of VEGF-C signaling using the soluble VEGF-C trap and the
PI3K downstream target mTOR using Rapamycin, but neither treatment alone, promotes the regression of experimental LM in mice. These results suggest that the best therapeutic outcome for
_PIK3CA__H1047R_-driven microcystic LM is achieved by co-inhibition of the VEGF-C/VEGFR3 and the downstream (mTOR) pathways. Therapies targeting the key upstream pathway in combination with
PI3K pathway inhibition may be relevant also for other _PIK3CA_-driven pathologies. METHODS PATIENTS Residual tissue of macrocystic and microcystic LMs were collected from patients
undergoing therapeutical surgery. All participants gave their informed consent, as approved by the ethical committee of the Medical Faculty of the University of Louvain, Brussels, Belgium.
All protocols were compliant with the Belgian laws governing research on human subjects. The phenotypes of the patients were evaluated as accurately as possible by the referring clinicians.
DNAs were extracted from crunched (powderized) snap-frozen tissues, using Wizard genomic DNA purification kit (Promega). DNAs were screened by Ion Torrent technology with a custom Ampliseq
panel (www.ampliseq.com) designed to cover the coding exons of _PIK3CA_. Genetic variants were analyzed using Highlander software (http://sites.uclouvain.be/highlander/). Histology was
examined by a pathologist expert in vascular anomalies. MOUSE LINES AND TREATMENTS _R26-LSL-PIK3CA__H1047R_ 22, knock-in _LSL-Pik3ca__H1047R_ 33, _Cdh5-CreER__T2_ 59, _Vegfr3-CreER__T2_ 23,
_Prox1-CreER__T2_ 24, and _R26-mTmG_60 mice were analyzed on a C57BL/6J background. Both female and male mice were used for analyses and no differences in the phenotype between the genders
were observed. The morning of vaginal plug detection was considered as embryonic day 0 (E0). For inducing recombination during embryonic development 4-hydroxytamoxifen (4-OHT, H7904, Sigma)
dissolved in peanut oil (10 mg ml−1) was administered intraperitoneally to pregnant females. For postnatal induction, 4-OHT dissolved in acetone (10 mg ml−1), was applied topically to the
dorsal side of the right ear of each mouse. The 4-OHT doses and days of administration are indicated in the figures and/or figure legends and summarized in Supplementary Table 1. Additional
information on the routes of administration and the effect are provided in Supplementary Table 1. For inhibition of VEGF-C signaling, we used adeno-associated viral (AAV)-derived VEGF-C trap
encoding the ligand binding domains 1–4 of VEGFR3, fused to the IgG Fc domain (AAV9-mVEGFR31–4-Ig) and control AAVs that encoded the inactive domains four to seven of VEGFR3-Ig
(AAV9-mVEGFR34-7-Ig)36. Mice received a single intraperitoneal injection of 1 × 1010 virus particles diluted in PBS at a total volume of 100 µl at the indicated time point. PBS or
AAV9-mVEGFR34-7-Ig were used as control treatments. Rapamycin (R-5000 Rapamycin, >99% LC Labs) was dissolved in DMSO at 10 mg ml−1 and injected intraperitoneally either once per day
(Supplementary Fig. 9) or every second day (Fig. 5) at the dose of 10 mg kg−1. DMSO was used as a control. A single dose (2.5 × 1010 viral particles per ear in 10 µl) of AAVs encoding
VEGF-C61,62 was injected intradermally into both ears of 5 weeks old adult mice. All experimental procedures were approved by the Uppsala Animal Experiment Ethics Board and performed in
compliance with all relevant Swedish regulations, or the Catalan Departament d’ Agricultura, Ramaderia i Pesca, following protocols approved by the local Ethics Committees of IDIBELL-CEEA.
ANTIBODIES The details of primary antibodies used for immunofluorescence of whole mount tissues, cells and paraffin-embedded sections are provided in Supplementary Table 2. Secondary
antibodies conjugated to Cy3, Alexa Fluor 405, 488 or 647 were obtained from Jackson ImmunoResearch. IMMUNOFLUORESCENCE Whole-mount tissue was fixed in 4% paraformaldehyde at room
temperature for 2 h followed by permeabilization in 0.3% Triton X-100 in PBS (PBST) for 10 min and blocking in PBST plus 3% milk for 2 h. Primary antibodies were incubated at 4 °C overnight
in blocking buffer and washed in PBST before incubating them with fluorescence-conjugated secondary antibodies in blocking buffer for 2 h at room temperature. Stained samples were then
washed and mounted in Mowiol. Cells were fixed with 4% paraformaldehyde at room temperature for 20 min, washed twice with PBS and permeabilized in 0.5% Triton X-100 in PBS for 5 min, and
blocked in PBST plus 2% BSA for 1 h. Cells were incubated with primary antibodies diluted in the blocking buffer at room temperature for 1 h. After washing three times with PBS plus 0.2%
BSA, the cells were incubated with fluorescence-conjugated secondary antibodies at room temperature for 45 min, followed by staining with DAPI (D9542, Sigma, 1:1000) for 5 min, and fixing
with 4% paraformaldehyde for 4 min before further washing and mounting in Mowiol. IMMUNOSTAINING OF PARAFFIN SECTIONS Tissue was fixed in 10% neutral buffered formalin (human) or 4%
paraformaldehyde (mouse) and embedded in paraffin. Deparaffinization and rehydration steps were performed manually on 4 μm (human) or 5–6 μm (mouse) paraffin sections. Heat-induced antigen
retrieval was performed using Sodium Citrate buffer (10 mM, pH 6) at 95 °C. Immunohistochemistry with antibodies against PROX1 and PDPN (Supplementary Table 1) were performed on an automatic
immunostainer, Ventana Benchmark Ultra. For immunofluorescence, paraffin sections were blocked with TNB (Tris-NaCl-blocking buffer, prepared according to the Tyramide Signal Amplification
kit (TSATM, NENTM Life Science Products) and washed with TNT buffer (0.1 M Tris pH 7.5, 0.15 M NaCl, 0.05% Tween 20). The TSATM kit was used to enhance and detect the signal of goat
anti-mouse VEGFR3 (AF743, R&D Systems) and rat anti-mouse CD45 antibody (ab25386, Abcam) in the mouse paraffin sections and mouse anti-human VEGFR3 (clone 9D9F9, Millipore) antibody in
the human paraffin sections. All other primary antibodies (see Supplementary Table 1) were used at 4 °C overnight and visualized with fluorescence-conjugated secondary antibodies after the
TSA kit. The majority of the slides were mounted in Mowiol except the ones with CD45 primary antibody, where Autofluorescence Quenching kit (Vector® TrueVIEWTM) together with VECTASHIELD®
HardSetTM Antifade Mounting Media was used to decrease autofluorescence. PRIMARY LEC CULTURE Murine primary dermal LECs were isolated from the tail skin of 6-13 weeks old
_LSL-PIK3CA__H1047R_;_Vegfr3-CreER__T2_ mice by sequential selection with PECAM1 (Mec13.3, Pharmingen) and LYVE1 (Aly7, Abnova) antibodies bound to Dynabeads, as described previously23.
Mouse LECs were cultured on 0.5% gelatin (G1393, Sigma)-coated dishes in complete DMEM medium. To induce Cre-mediated recombination, 4-OHT was dissolved in absolute ethanol and added to the
culture medium at the final concentration of 5 µM for 48 h. Cell were then reseeded in 12-wells at (low) density of 3 × 104 cells per cm2 for western blot analysis and qRT-PCR analysis. For
serum starvation, cells were reseeded after 4-OHT treatment at the low density and starved overnight in 0.5% fetal bovine serum (FBS) containing medium and stimulated with VEGF-C (R&D
Systems, 200 ng ml−1) for time periods indicated in the figures. To assess cell migration in vitro, wound-healing assays were performed with IncuCyte ZOOMTM according to the manufacturer’s
instructions. Cells were reseeded in 96-well ImageLock plate (Essen BioScience) at density of 6.25 × 104 cells per cm2 after 4-OHT treatment. WoundMakerTM (Essen BioScience) was used to
create homogeneous scratch wounds, and the cells were then washed twice with fresh medium to remove any debris, followed by adding 100 µl fresh complete DMEM medium supplemented with or
without VEGF-C (25 ng ml−1) to each well. The plate was placed into the IncuCyte ZOOMTM apparatus and images of cells were acquired automatically every 1 h for a total duration of 72 h. All
cells were cultured at 37 °C in a humidified atmosphere with 5% CO2. WESTERN BLOT ANALYSIS Total protein extract was obtained by lysing cells in lysis buffer [150 mM NaCl, 1% Triton X-100,
0.5% Sodium deoxycholate, 0.1% SDS, 50 mM Tris-HCl (pH 7.6) supplemented with 25 mM NaF, 1 mM Na3VO4 and protein inhibitor cocktail (11873580001, Roche)]. Cell lysates were spinned for 10
min at 13200 r.p.m. at 4 °C and supernatants were collected. Protein concentration was determined using a BCA™ Protein Assay Kit (23227, Thermo Fisher Scientific) according to manufacturer’s
instructions and measured using Gen5 All-In-One microplate reader. Equal amounts of proteins were loaded and separated in 4-20% gradient polyacrylamide gels (Invitrogen), transferred to a
polyvinylidene difluoride membrane (PVDF; 88520, Thermo Fisher Scientific) and blocked for 1 h at room temperature in 1× tris buffered saline tween (TBST) [150 mM NaCl, 10 mM Tris-HCl (pH
7.4) and 0.1% Tween] containing 5% (w/v) bovine serum albumin (BSA). The membranes were subjected to overnight incubation at 4 °C with primary antibodies diluted in 1× TBST plus 5% BSA.
Following this incubation, membranes were rinsed three times with 1× TBST for 5 min each and incubated for 1 h at room temperature with HRP-conjugated secondary antibodies (diluted in 1×
TBST plus 5% BSA). Membranes were rinsed three times with TBST for 5 min each and specific binding was detected using the enhanced chemiluminescence (ECL) system (WP20005, Invitrogen) and
the ChemiDoc XRS + System (Biorad). All images were collected using Image Lab software. Protein molecular masses were estimated relatively to the electrophoretic mobility of co-transferred
prestained protein marker (26634, Thermo Fisher Scientific). The following antibodies were used: rabbit anti-mouse phospho-Akt (Ser473) (#4060), phospho-Akt (Thr308) (#2965), Akt (#9272),
VEGFR2 (#2479), GAPDH (#2118, all from CST and 1:2000), goat anti-mouse VEGFR3 (AF743, R&D Systems, 1:1000). VEGFR31–4-Ig and VEGFR34–7-Ig proteins in serum were detected by western
blotting of 0.5 µl serum samples collected at the indicated time points as described63. 50, 100, and 200 ng of recombinant mouse VEGFR3 chimera protein (743-R3-100, R&D Systems) were
used as a standard for calculating the concentration of VEGFR31–4-Ig and VEGFR34–7-Ig proteins. Mouse VEGFR3 domains 1–4 and 4–7 were detected with polyclonal goat anti–mouse VEGFR3 antibody
(AF743, R&D Systems, 1:1000) against the extracellular domain of VEGFR3. The blots were quantified using ImageJ software. Full blots are shown in source data. QRT-PCR ANALYSIS Total RNA
was isolated from dermal mouse LECs using RNeasy Mini kit (Qiagen). Complementary DNA (cDNA) was synthesized using Superscript VILO Master Mix (Invitrogen). cDNA was analyzed by real-time
quantitative PCR (qRT-PCR) (StepOne Plus system, Applied Biosystems) using TaqMan gene expression assays and TaqMan gene expression Master Mix (Applied Biosystems). Relative quantifications
of gene expression were performed using the comparative cycle threshold method (ΔCT) with _Gapdh_ as the reference gene. TaqMan Assays used for mouse LECs were as followed: _Vegfr2_
(Mm01222421_m1), _Vegfr3_ (Mm01292604_m1), _Gapdh_ (Mm99999915_g1). The values represent average relative gene expression. FLOW CYTOMETRY For FACS analysis of proliferating cells ear skin of
adult mice were dissected, cut into small pieces and digested in Collagenase IV (Life Technologies) 10 mg ml−1, DNase I (Roche) 0.1 mg ml−1 and FBS 0.5 % (Life Technologies) in PBS at 37 °C
for about 30 min with vigorous shaking every 5 min. Collagenase activity was quenched by dilution with FACS buffer (PBS, 0.5% FBS, 2 mM EDTA) and digestion products were filtered twice
through 70 µm nylon filters (BD Biosciences). Cells were again washed with FACS buffer and immediately processed for immunostaining first by blocking Fc receptor binding with rat anti-mouse
CD16/CD32 (eBiosciences) followed by incubation with antibodies targeting PDPN, CD31/PECAM1, CD45 and CD11b (all obtained from eBioscience, see Supplementary Table 2). Two different panels
of antibodies were used depending on if samples were taken from mice with _R26-mTmG_ reporter or not. After staining, cells were washed with PBS and then stained for dead cells using the
blue LIVE/DEAD® fixable dead cell stain kit (Life Technologies), followed by fixation and permeabilization using the Foxp3/Transcription factor staining kit (eBioscience) according to the
manufacturer’s instructions. Finally cells were incubated with rat serum and KI67 antibody (eBioscience). Cells were analyzed on a BD LSR Fortessa cell analyzer equipped with 5 lasers (355,
405, 488, 561, and 643 nm). Compensation was performed using the anti-rat/hamster compensation bead kit and the ArC amine reactive compensation bead kit (Life Technologies). Single viable
cells were gated from FSC-A/SSC-A, FSC-H/FSC-W and SSC-H/SSC-W plots followed by exclusion of dead cells in the UV dump channel. FMO controls were used to set up the subsequent gating scheme
to obtain cell populations and quantification of proliferating cells (Supplementary Fig. 10). For FACS analysis of immune cells the ear skin was dissected into dorsal and ventral parts, cut
into pieces and digested in Liberase TL (Roche) 100 µg ml−1, DNase I (Roche) 0.5 mg ml−1 in PBS with 0.2% FBS at 37 °C for 1.5 h at 500 r.p.m. Liberase TL activity was quenched by adding 2
mM EDTA and the product was filtered through 50 µm filters (CellTricks). The cells were washed with FACS buffer (PBS, 0.5% FBS, 2 mM EDTA) and incubated first with rat anti-mouse CD16/32
antibody (eBioscience) for blocking of the Fc receptor binding and then with CD45, CD11b and F4/80 targeting antibodies (Supplementary Table 2). Cell death was analyzed by adding SYTOX Blue
dead stain (Life Technologies). The cell suspension was filtered again immediately before analysis. The analysis was obtained on CytoFLEX Flow Cytometer (Beckman Coulter). Single cells were
gated from SSC-H/FSC-H and FSC-Width/FSC-H plots followed by gating for CD45+ viable cells and CD11b+F4/80+ cells (Supplementary Fig. 9). All flow data was processed using FlowJo software
version 10.5.0 (TreeStar). IMAGE ACQUISITION AND QUANTIFICATION All confocal images represent maximum intensity projections of Z-stacks of single tiles or multiple tile scan images. Images
were acquired using Leica SP8 confocal microscope or Leica DMi8 fluorescence microscope with Leica LAS X software. Quantification of lymphatic vessel branching was done with Angiotool plugin
of ImageJ (version 2.0.0-rc-65/1.5lu) using tile scan images of adult ear skin (xy = 3260 μm × 2200 μm, tip region) or dorsal skin of E17 embryos (xy = 2322 μm × 4644 μm, cervical/thoracic
region). Quantification of VEGFR3 staining intensity was done by measuring corrected total cell fluorescence (CTCF) = integrated density – (area of selected cell × mean fluorescence of
background readings) using ImageJ, and the vessel area was determined by combined staining of LYVE1 and VEGFR3. Vessel ends with blunt or spiky morphology were marked with Photoshop CS6
software and counted manually using tile scan images of adult ear skin (xy = 3260 μm × 2200 μm at the tip of the ear excluding the region 34 μm from the edge of the ear) and presented as
number of ends per ear. All quantifications include littermate controls; for _Cdh5-CreER__T2_ model Cre- littermates treated with 4-OHT were used (Supplementary Figs. 8, 9),
_Vegfr3-CreER__T2_ model Cre+ untreated (Figs. 4, 5) or vehicle-treated (Figs. 4, 5) mice were used. At least two different litters of mice were analyzed. For validation of the purity of
isolated primary LEC populations, % of VE-cadherin+ cells and % of PROX1+ cells were quantified using maximum intensity projection images based on staining of DAPI, VE-cadherin and PROX1
(_n_ = 1386 cells in total from 15 experimental conditions and 2 batches of cells). The cells were marked using Photoshop CS6 software and counted manually. The images acquired by IncuCyte
ZOOMTM were processed and analyzed using IncuCyteTM scratch wound cell migration software module. Cell density in the wound area expressed relative to the cell density outside of the wound
area over time (relative wound density%) was quantified. The quantification of images from western blots was done using ImageJ software. STATISTICS AND REPRODUCIBILITY Graphpad Prism was
used for graphic representation and statistical analysis of the data. Data between two groups were compared with One-sample _t_-test (Fig. 3i), or paired (Supplementary Fig. 4d) or unpaired
(all others) two-tailed Student’s _t_-test, assuming equal variance. Differences were considered statistically significant when _P_ < 0.05. The experiments were not randomized, and no
blinding was done in the analysis and quantifications. No statistical methods were used to predetermine the sample size. All microscopy images of mouse tissues are representative of a
minimum _n_ = 3 mice except for Fig. 3c, wild-type embryonic back skin _n_ = 1. REPORTING SUMMARY Further information on research design is available in the Nature Research Reporting Summary
linked to this article. DATA AVAILABILITY The next-generation sequencing data that support the findings of this study are available on request from MV. The data are not publicly available
due to them containing information that could compromise research participant consent. All other data supporting the findings of this study are available from the corresponding author (TM)
upon request. The source data underlying Figs. 2c, 3b, f–i, 4b, d, g, 5c, d, f and Supplementary Figs. 2e, 4d–h, 5a, b, 6b, c, e, f, 7a, b, 8c, d, 9c, f are provided as a Source Data file.
REFERENCES * Limaye, N., Boon, L. M. & Vikkula, M. From germline towards somatic mutations in the pathophysiology of vascular anomalies. _Hum. Mol. Genet._ 18, R65–R74 (2009). Article
CAS PubMed PubMed Central Google Scholar * Castillo, S. D., Baselga, E. & Graupera, M. PIK3CA mutations in vascular malformations. _Curr. Opin. Hematol._
https://doi.org/10.1097/MOH.0000000000000496 (2019). Article PubMed Google Scholar * Seront, E., Van Damme, A., Boon, L. M. & Vikkula, M. Rapamycin and treatment of venous
malformations. _Curr. Opin. Hematol._ https://doi.org/10.1097/MOH.0000000000000498 (2019). Article PubMed Google Scholar * Castel, P. et al. Somatic PIK3CA mutations as a driver of
sporadic venous malformations. _Sci. Transl. Med._ 8, 332ra42 (2016). Article PubMed PubMed Central CAS Google Scholar * Castillo, S. D. et al. Somatic activating mutations in Pik3ca
cause sporadic venous malformations in mice and humans. _Sci. Transl. Med._ 8, 332ra43 (2016). Article PubMed PubMed Central CAS Google Scholar * Limaye, N. et al. Somatic activating
PIK3CA mutations cause venous malformation. _Am. J. Hum. Genet._ 97, 914–921 (2015). Article CAS PubMed PubMed Central Google Scholar * Luks, V. L. et al. Lymphatic and other vascular
malformative/overgrowth disorders are caused by somatic mutations in PIK3CA. _J. Pediatr._ 166, 1048–1054.e1–5 (2015). Article CAS PubMed PubMed Central Google Scholar * Osborn, A. J.
et al. Activating PIK3CA alleles and lymphangiogenic phenotype of lymphatic endothelial cells isolated from lymphatic malformations. _Hum. Mol. Genet_. 24, 926–938 (2015). Article CAS
PubMed Google Scholar * Madsen, R. R., Vanhaesebroeck, B. & Semple, R. K. Cancer-associated PIK3CA mutations in overgrowth disorders. _Trends Mol. Med._ 24, 856–870 (2018). Article
CAS PubMed PubMed Central Google Scholar * Burke, J. E., Perisic, O., Masson, G. R., Vadas, O. & Williams, R. L. Oncogenic mutations mimic and enhance dynamic events in the natural
activation of phosphoinositide 3-kinase p110α (PIK3CA). _Proc. Natl Acad. Sci. USA_ 109, 15259–15264 (2012). Article ADS CAS PubMed PubMed Central Google Scholar * Vanhaesebroeck, B.,
Stephens, L. & Hawkins, P. PI3K signalling: the path to discovery and understanding. _Nat. Rev. Mol. Cell Biol._ 13, 195–203 (2012). Article CAS PubMed Google Scholar * Graupera, M.
et al. Angiogenesis selectively requires the p110alpha isoform of PI3K to control endothelial cell migration. _Nature_ 453, 662–666 (2008). Article ADS CAS PubMed Google Scholar *
Gupta, S. et al. Binding of ras to phosphoinositide 3-kinase p110alpha is required for ras-driven tumorigenesis in mice. _Cell_ 129, 957–968 (2007). Article CAS PubMed Google Scholar *
Stanczuk, L. et al. cKit lineage hemogenic endothelium-derived cells contribute to mesenteric lymphatic vessels. _Cell Rep._ https://doi.org/10.1016/j.celrep.2015.02.026 (2015). Article
PubMed Google Scholar * di Blasio, L. et al. PI3K/mTOR inhibition promotes the regression of experimental vascular malformations driven by PIK3CA-activating mutations. _Cell Death Dis._ 9,
45 (2018). Article PubMed PubMed Central CAS Google Scholar * Rodriguez-Laguna, L. et al. Somatic activating mutations in PIK3CA cause generalized lymphatic anomaly. _J. Exp. Med_.
216, 407–418 (2019). Article CAS PubMed PubMed Central Google Scholar * Boscolo, E. et al. Rapamycin improves TIE2-mutated venous malformation in murine model and human subjects. _J.
Clin. Invest_. 125, 3491–3504 (2015). Article PubMed PubMed Central Google Scholar * Hammer, J. et al. Sirolimus is efficacious in treatment for extensive and/or complex slow-flow
vascular malformations: a monocentric prospective phase II study. _Orphanet J. Rare Dis._ 13, 191 (2018). Article PubMed PubMed Central Google Scholar * Wiegand, S., Wichmann, G. &
Dietz, A. Treatment of lymphatic malformations with the mTOR inhibitor sirolimus: a systematic review. _Lymphat. Res. Biol._ 16, 330–339 (2018). Article CAS PubMed Google Scholar *
Uebelhoer, M., Boon, L. M. & Vikkula, M. Vascular anomalies: from genetics toward models for therapeutic trials. _Cold Spring Harb. Perspect. Med_. 2, a009688 (2012). * Kirsh, A. L.,
Cushing, S. L., Chen, E. Y., Schwartz, S. M. & Perkins, J. A. Tertiary lymphoid organs in lymphatic malformations. _Lymphat. Res. Biol._ 9, 85–92 (2011). Article CAS PubMed PubMed
Central Google Scholar * Eser, S. et al. Selective requirement of PI3K/PDK1 signaling for Kras oncogene-driven pancreatic cell plasticity and cancer. _Cancer Cell_ 23, 406–420 (2013).
Article CAS PubMed Google Scholar * Martinez-Corral, I. et al. Vegfr3-CreER (T2) mouse, a new genetic tool for targeting the lymphatic system. _Angiogenesis_ 19, 433–445 (2016). *
Bazigou, E. et al. Genes regulating lymphangiogenesis control venous valve formation and maintenance in mice. _J. Clin. Invest._ 121, 2984–2992 (2011). Article CAS PubMed PubMed Central
Google Scholar * Bernier-Latmani, J. et al. DLL4 promotes continuous adult intestinal lacteal regeneration and dietary fat transport. _J. Clin. Invest_. 125, 4572–4586 (2015). Article
PubMed PubMed Central Google Scholar * Angulo-Urarte, A. et al. Endothelial cell rearrangements during vascular patterning require PI3-kinase-mediated inhibition of actomyosin
contractility. _Nat. Commun._ 9, 4826 (2018). Article ADS PubMed PubMed Central CAS Google Scholar * Baluk, P. et al. Functionally specialized junctions between endothelial cells of
lymphatic vessels. _J. Exp. Med._ 204, 2349–2362 (2007). Article CAS PubMed PubMed Central Google Scholar * Bentley, K. et al. The role of differential VE-cadherin dynamics in cell
rearrangement during angiogenesis. _Nat. Cell Biol._ 16, 309–321 (2014). Article CAS PubMed Google Scholar * Hayer, A. et al. Engulfed cadherin fingers are polarized junctional
structures between collectively migrating endothelial cells. _Nat. Cell Biol._ 18, 1311–1323 (2016). Article CAS PubMed PubMed Central Google Scholar * Neto, F. et al. YAP and TAZ
regulate adherens junction dynamics and endothelial cell distribution during vascular development. _eLife_ 7, e31037 (2018). * Vaahtomeri, K., Karaman, S., Mäkinen, T. & Alitalo, K.
Lymphangiogenesis guidance by paracrine and pericellular factors. _Genes Dev._ 31, 1615–1634 (2017). Article CAS PubMed PubMed Central Google Scholar * Hon, W.-C., Berndt, A. &
Williams, R. L. Regulation of lipid binding underlies the activation mechanism of class IA PI3-kinases. _Oncogene_ 31, 3655–3666 (2012). Article CAS PubMed Google Scholar * Kinross, K.
M. et al. An activating Pik3ca mutation coupled with Pten loss is sufficient to initiate ovarian tumorigenesis in mice. _J. Clin. Invest._ 122, 553–557 (2012). Article CAS PubMed PubMed
Central Google Scholar * Harvey, N. L. & Gordon, E. J. Deciphering the roles of macrophages in developmental and inflammation stimulated lymphangiogenesis. _Vasc. Cell_ 4, 15 (2012).
Article CAS PubMed PubMed Central Google Scholar * Schoppmann, S. F. et al. Tumor-associated macrophages express lymphatic endothelial growth factors and are related to peritumoral
lymphangiogenesis. _Am. J. Pathol._ 161, 947–956 (2002). Article CAS PubMed PubMed Central Google Scholar * Fang, S. et al. Critical requirement of VEGF-C in transition to fetal
erythropoiesis. _Blood_ 128, 710–720 (2016). Article CAS PubMed Google Scholar * Mäkinen, T. et al. Inhibition of lymphangiogenesis with resulting lymphedema in transgenic mice
expressing soluble VEGF receptor-3. _Nat. Med._ 7, 199–205 (2001). Article PubMed Google Scholar * Karpanen, T. et al. Lymphangiogenic growth factor responsiveness is modulated by
postnatal lymphatic vessel maturation. _Am. J. Pathol._ 169, 708–718 (2006). Article CAS PubMed PubMed Central Google Scholar * Baluk, P. et al. Rapamycin reversal of VEGF-C-driven
lymphatic anomalies in the respiratory tract. _JCI Insight_ 2, e90103 (2017). * Ulvmar, M. H. & Mäkinen, T. Heterogeneity in the lymphatic vascular system and its origin. _Cardiovasc.
Res._ 111, 310–321 (2016). Article CAS PubMed PubMed Central Google Scholar * Frye, M. et al. Matrix stiffness controls lymphatic vessel formation through regulation of a
GATA2-dependent transcriptional program. _Nat. Commun._ 9, 1511 (2018). Article ADS PubMed PubMed Central CAS Google Scholar * Bosisio, D., Ronca, R., Salvi, V., Presta, M. &
Sozzani, S. Dendritic cells in inflammatory angiogenesis and lymphangiogenesis. _Curr. Opin. Immunol._ 53, 180–186 (2018). Article CAS PubMed Google Scholar * Mahmoud, M. et al.
Pathogenesis of arteriovenous malformations in the absence of endoglin. _Circ. Res._ 106, 1425–1433 (2010). Article CAS PubMed Google Scholar * Ola, R. et al. PI3 kinase inhibition
improves vascular malformations in mouse models of hereditary haemorrhagic telangiectasia. _Nat. Commun._ 7, 13650 (2016). Article ADS CAS PubMed PubMed Central Google Scholar * Park,
S. O. et al. Real-time imaging of de novo arteriovenous malformation in a mouse model of hereditary hemorrhagic telangiectasia. _J. Clin. Invest._ 119, 3487–3496 (2009). CAS PubMed PubMed
Central Google Scholar * Boulday, G. et al. Developmental timing of CCM2 loss influences cerebral cavernous malformations in mice. _J. Exp. Med_. 208, 1835–1847 (2011). Article CAS
PubMed PubMed Central Google Scholar * Bravi, L. et al. Sulindac metabolites decrease cerebrovascular malformations in CCM3-knockout mice. _Proc. Natl Acad. Sci. USA_ 112, 8421–8426
(2015). Article ADS CAS PubMed PubMed Central Google Scholar * Potente, M. & Mäkinen, T. Vascular heterogeneity and specialization in development and disease. _Nat. Rev. Mol. Cell
Biol._ 18, 477–494 (2017). Article CAS PubMed Google Scholar * McGranahan, N. & Swanton, C. Clonal heterogeneity and tumor evolution: past, present, and the future. _Cell_ 168,
613–628 (2017). Article CAS PubMed Google Scholar * Pagenstecher, A., Stahl, S., Sure, U. & Felbor, U. A two-hit mechanism causes cerebral cavernous malformations: complete
inactivation of CCM1, CCM2 or CCM3 in affected endothelial cells. _Hum. Mol. Genet_. 18, 911–918 (2009). Article CAS PubMed Google Scholar * Akers, A. L., Johnson, E., Steinberg, G. K.,
Zabramski, J. M. & Marchuk, D. A. Biallelic somatic and germline mutations in cerebral cavernous malformations (CCMs): evidence for a two-hit mechanism of CCM pathogenesis. _Hum. Mol.
Genet_. 18, 919–930 (2009). Article CAS PubMed Google Scholar * Malinverno, M. et al. Endothelial cell clonal expansion in the development of cerebral cavernous malformations. _Nat.
Commun._ 10, 2761 (2019). Article ADS PubMed PubMed Central CAS Google Scholar * Detter, M. R., Snellings, D. A. & Marchuk, D. A. Cerebral cavernous malformations develop through
clonal expansion of mutant endothelial cells. _Circ. Res._ 123, 1143–1151 (2018). Article CAS PubMed PubMed Central Google Scholar * Luo, Y. et al. Rapamycin inhibits lymphatic
endothelial cell tube formation by downregulating vascular endothelial growth factor receptor 3 protein expression. _Neoplasia N. Y. N._ 14, 228–237 (2012). Article CAS Google Scholar *
Zhang, Y. et al. Heterogeneity in VEGFR3 levels drives lymphatic vessel hyperplasia through cell-autonomous and non-cell-autonomous mechanisms. _Nat. Commun._ 9, 1296 (2018). Article ADS
PubMed PubMed Central CAS Google Scholar * Venot, Q. et al. Targeted therapy in patients with PIK3CA-related overgrowth syndrome. _Nature_ 558, 540–546 (2018). Article ADS CAS PubMed
PubMed Central Google Scholar * Boscolo, E. et al. AKT hyper-phosphorylation associated with PI3K mutations in lymphatic endothelial cells from a patient with lymphatic malformation.
_Angiogenesis_ 18, 151–162 (2015). Article CAS PubMed Google Scholar * Partanen, T. A. et al. Neuropilin-2 and vascular endothelial growth factor receptor-3 are up-regulated in human
vascular malformations. _Angiogenesis_ 16, 137–146 (2013). Article CAS PubMed Google Scholar * Wang, Y. et al. Ephrin-B2 controls VEGF-induced angiogenesis and lymphangiogenesis.
_Nature_ 465, 483–486 (2010). Article ADS CAS PubMed Google Scholar * Muzumdar, M. D., Tasic, B., Miyamichi, K., Li, L. & Luo, L. A global double-fluorescent Cre reporter mouse.
_Genesis_ 45, 593–605 (2007). Article CAS PubMed Google Scholar * Alitalo, A. K. et al. VEGF-C and VEGF-D blockade inhibits inflammatory skin carcinogenesis. _Cancer Res._ 73, 4212–4221
(2013). Article CAS PubMed Google Scholar * Antila, S. et al. Development and plasticity of meningeal lymphatic vessels. _J. Exp. Med._ 214, 3645–3667 (2017). Article CAS PubMed
PubMed Central Google Scholar * Karaman, S., Nurmi, H., Antila, S. & Alitalo, K. Stimulation and inhibition of lymphangiogenesis via adeno-associated viral gene delivery. _Methods Mol.
Biol. Clifton NJ_ 1846, 291–300 (2018). Article CAS Google Scholar Download references ACKNOWLEDGEMENTS We thank Sagrario Ortega (CNIO, Madrid) for the _Vegfr3_-_CreER__T2_ mice and Ralf
Adams (Max Planck Institute for Molecular Biomedicine, Münster) for the _Cdh5_-_CreER__T2_ mice. We also thank the BioVis facility (Uppsala University, Sweden) for flow cytometer usage and
support, and Simon Stritt for help with flow cytometry and Sofie Lunell-Sergerqvist for technical assistance. This work was supported by the Swedish Cancer Society (CAN 2016/535), the
European Research Council (ERC-2014-CoG-646849), Knut and Alice Wallenberg Foundation (2015.0030) and the Swedish Research Council (542-2014-3535) to T.M.; the F.R.S.-FNRS (Fonds de la
Recherche Scientifique, Belgium), grant [T.0026.14] to M.V. and [T.0146.16] to L.B., and the Walloon Excellence in Lifesciences & BIOtechnology (FNRS-WELBIO) grant [WELBIO-CR-2010-15R]
and the Fund Generet managed by the King Baudouin Foundation to M.V.; and Academy of Finland (grants 314498, 320249) to K.A. Laboratories of M.V. and T.M. are part of V.A.Cure, and thus
received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No 814316. P.B. is a Senior Platform Manager of the
University of Louvain. MG lab is supported by Ministerio de Ciencia, Innovación y Universidades, which is part of Agencia Estatal de Investigación (AEI, Spain) through the projects
SAF2017-89116-R co-funded by European Regional Developmental Fund (ERDF), a Way to Build Europe; by la Fundació Bancària “La Caixa”; by the CERCA program of la Generalitat de Catalunya.
S.D.C. is a recipient of a fellowship from the European Union’s Horizon 2020 Research and Innovation Programme under the Marie Sklodowska-Curie grant agreement No. 749731. Open access
funding provided by Uppsala University. AUTHOR INFORMATION Author notes * These authors contributed equally: Ines Martinez-Corral, Yan Zhang. AUTHORS AND AFFILIATIONS * Uppsala University,
Department of Immunology, Genetics and Pathology, Dag Hammarskjölds väg 20, 751 85, Uppsala, Sweden Ines Martinez-Corral, Yan Zhang, Milena Petkova, Henrik Ortsäter, Sofie Sjöberg &
Taija Mäkinen * Vascular Signaling Laboratory, Institut d´Investigació Biomèdica de Bellvitge (IDIBELL), 08908L´Hospitalet de Llobregat, Barcelona, Spain Sandra D. Castillo & Mariona
Graupera * Human Molecular Genetics, de Duve Institute, University of Louvain, Brussels, Belgium Pascal Brouillard, Laurence Boon & Miikka Vikkula * Center for Vascular Anomalies,
Division of Pathology, Cliniques universitaires Saint Luc, University of Louvain, 10 avenue Hippocrate, B-1200, Brussels, Belgium Louis Libbrecht * Department of Internal Medicine 2,
Klinikum rechts der Isar, Technische Universität München, Ismaningerstr. 22, 81675, München, Germany Dieter Saur * Wihuri Research Institute and Translational Cancer Biology Program,
Biomedicum Helsinki, FIN-00014 University of Helsinki, Helsinki, Finland Kari Alitalo * Center for Vascular Anomalies, Division of Plastic Surgery, Cliniques universitaires Saint Luc,
University of Louvain, 10 avenue Hippocrate, B-1200, Brussels, Belgium Laurence Boon * Walloon Excellence in Lifesciences and Biotechnology (WELBIO), University of Louvain, Brussels, Belgium
Miikka Vikkula Authors * Ines Martinez-Corral View author publications You can also search for this author inPubMed Google Scholar * Yan Zhang View author publications You can also search
for this author inPubMed Google Scholar * Milena Petkova View author publications You can also search for this author inPubMed Google Scholar * Henrik Ortsäter View author publications You
can also search for this author inPubMed Google Scholar * Sofie Sjöberg View author publications You can also search for this author inPubMed Google Scholar * Sandra D. Castillo View author
publications You can also search for this author inPubMed Google Scholar * Pascal Brouillard View author publications You can also search for this author inPubMed Google Scholar * Louis
Libbrecht View author publications You can also search for this author inPubMed Google Scholar * Dieter Saur View author publications You can also search for this author inPubMed Google
Scholar * Mariona Graupera View author publications You can also search for this author inPubMed Google Scholar * Kari Alitalo View author publications You can also search for this author
inPubMed Google Scholar * Laurence Boon View author publications You can also search for this author inPubMed Google Scholar * Miikka Vikkula View author publications You can also search for
this author inPubMed Google Scholar * Taija Mäkinen View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS I.M.C., Y.Z., M.P., H.O., S.D.C.,
M.G., M.V., and T.M. designed experiments and analyzed data; I.M.C., Y.Z., M.P., H.O., S.S., and S.D.C. performed experiments; P.B., L.L., L.B., and M.V. provided clinical patient data and
material; D.S. and K.A. provided essential tools and advice; T.M. supervised the project and wrote the manuscript with input from other authors. All authors discussed the results and
commented on the manuscript. CORRESPONDING AUTHOR Correspondence to Taija Mäkinen. ETHICS DECLARATIONS COMPETING INTERESTS K.A. and T.M. have filed a patent application related to the
manuscript as inventors. Other authors declare no competing interests. ADDITIONAL INFORMATION PEER REVIEW INFORMATION _Nature Communications_ thanks the anonymous reviewer(s) for their
contribution to the peer review of this work. Peer reviewer reports are available. PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and
institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION PEER REVIEW FILE REPORTING SUMMARY SOURCE DATA SOURCE DATA RIGHTS AND PERMISSIONS OPEN ACCESS This article is
licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give
appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in
this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative
Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a
copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Martinez-Corral, I., Zhang, Y., Petkova, M. _et al._
Blockade of VEGF-C signaling inhibits lymphatic malformations driven by oncogenic _PIK3CA_ mutation. _Nat Commun_ 11, 2869 (2020). https://doi.org/10.1038/s41467-020-16496-y Download
citation * Received: 13 July 2019 * Accepted: 30 April 2020 * Published: 08 June 2020 * DOI: https://doi.org/10.1038/s41467-020-16496-y SHARE THIS ARTICLE Anyone you share the following link
with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt
content-sharing initiative
