Cystine transporter regulation of pentose phosphate pathway dependency and disulfide stress exposes a targetable metabolic vulnerability in cancer
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT SLC7A11-mediated cystine uptake is critical for maintaining redox balance and cell survival. Here we show that this comes at a significant cost for cancer cells with high levels of
SLC7A11. Actively importing cystine is potentially toxic due to its low solubility, forcing cancer cells with high levels of SLC7A11 (SLC7A11high) to constitutively reduce cystine to the
more soluble cysteine. This presents a significant drain on the cellular NADPH pool and renders such cells dependent on the pentose phosphate pathway. Limiting glucose supply to SLC7A11high
cancer cells results in marked accumulation of intracellular cystine, redox system collapse and rapid cell death, which can be rescued by treatments that prevent disulfide accumulation. We
further show that inhibitors of glucose transporters selectively kill SLC7A11high cancer cells and suppress SLC7A11high tumour growth. Our results identify a coupling between
SLC7A11-associated cystine metabolism and the pentose phosphate pathway, and uncover an accompanying metabolic vulnerability for therapeutic targeting in SLC7A11high cancers. Access through
your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Access Nature and 54 other Nature
Portfolio journals Get Nature+, our best-value online-access subscription $32.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12 print issues and online access
$209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which are
calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS
SLC7A11 EXPRESSION LEVEL DICTATES DIFFERENTIAL RESPONSES TO OXIDATIVE STRESS IN CANCER CELLS Article Open access 21 June 2023 INHIBITION OF THIOREDOXIN REDUCTASE 1 SENSITIZES GLUCOSE-STARVED
GLIOBLASTOMA CELLS TO DISULFIDPTOSIS Article 23 December 2024 MTORC1 COUPLES CYST(E)INE AVAILABILITY WITH GPX4 PROTEIN SYNTHESIS AND FERROPTOSIS REGULATION Article Open access 11 March 2021
DATA AVAILABILITY Source Data for Figs. 1–6 and Extended Data Figs. 1–7 are provided with the paper. The 33 cancer-type data were derived from the TCGA Research Network:
http://cancergenome.nih.gov/. The RNA-seq data from PDXs have been deposited in dbGAP under accession number phs001980.v1.p1. All data supporting the findings of this study are available
from the corresponding author on reasonable request. REFERENCES * Pavlova, N. N. & Thompson, C. B. The emerging hallmarks of cancer metabolism. _Cell Metab._ 23, 27–47 (2016). Article
CAS PubMed PubMed Central Google Scholar * Boroughs, L. K. & DeBerardinis, R. J. Metabolic pathways promoting cancer cell survival and growth. _Nat. Cell Biol._ 17, 351–359 (2015).
Article CAS PubMed PubMed Central Google Scholar * DeBerardinis, R. J. & Chandel, N. S. Fundamentals of cancer metabolism. _Sci. Adv._ 2, e1600200 (2016). Article PubMed PubMed
Central Google Scholar * Wolpaw, A. J. & Dang, C. V. Exploiting metabolic vulnerabilities of cancer with precision and accuracy. _Trends Cell Biol._ 28, 201–212 (2018). Article CAS
PubMed Google Scholar * Bi, J., Wu, S., Zhang, W. & Mischel, P. S. Targeting cancer’s metabolic co-dependencies: A landscape shaped by genotype and tissue context. _Biochim. Biophys.
Acta_ 1870, 76–87 (2018). CAS Google Scholar * Narta, U. K., Kanwar, S. S. & Azmi, W. Pharmacological and clinical evaluation of l-asparaginase in the treatment of leukemia. _Crit.
Rev. Oncol. Hematol._ 61, 208–221 (2007). Article PubMed Google Scholar * Stipanuk, M. H. Sulfur amino acid metabolism: pathways for production and removal of homocysteine and cysteine.
_Annu. Rev. Nutr_. 24, 539–577 (2004). Article CAS PubMed Google Scholar * Conrad, M. & Sato, H. The oxidative stress-inducible cystine/glutamate antiporter, system xc−: cystine
supplier and beyond. _Amino Acids_ 42, 231–246 (2012). Article CAS PubMed Google Scholar * Lewerenz, J. et al. The cystine/glutamate antiporter system xc− in health and disease: from
molecular mechanisms to novel therapeutic opportunities. _Antioxid. Redox Signal._ 18, 522–555 (2013). Article CAS PubMed PubMed Central Google Scholar * Sato, H., Tamba, M., Ishii, T.
& Bannai, S. Cloning and expression of a plasma membrane cystine/glutamate exchange transporter composed of two distinct proteins. _J. Biol. Chem._ 274, 11455–11458 (1999). Article CAS
PubMed Google Scholar * Stipanuk, M. H., Dominy, J. E. Jr., Lee, J. I. & Coloso, R. M. Mammalian cysteine metabolism: new insights into regulation of cysteine metabolism. _J. Nutr._
136, 1652S–1659S (2006). Article CAS PubMed Google Scholar * Dixon, S. J. et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. _Cell_ 149, 1060–1072 (2012). Article
CAS PubMed PubMed Central Google Scholar * Stockwell, B. R. et al. Ferroptosis: A regulated cell death nexus linking metabolism, redox biology, and disease. _Cell_ 171, 273–285 (2017).
Article CAS PubMed PubMed Central Google Scholar * Zhang, Y. et al. BAP1 links metabolic regulation of ferroptosis to tumour suppression. _Nat. Cell Biol._ 20, 1181–1192 (2018). Article
CAS PubMed PubMed Central Google Scholar * Bhutia, Y. D., Babu, E., Ramachandran, S. & Ganapathy, V. Amino acid transporters in cancer and their relevance to “glutamine addiction”:
novel targets for the design of a new class of anticancer drugs. _Cancer Res._ 75, 1782–1788 (2015). Article CAS PubMed Google Scholar * Lo, M., Wang, Y. Z. & Gout, P. W. The xc−
cystine/glutamate antiporter: a potential target for therapy of cancer and other diseases. _J. Cell. Physiol._ 215, 593–602 (2008). Article CAS PubMed Google Scholar * Koppula, P.,
Zhang, Y., Zhuang, L. & Gan, B. Amino acid transporter SLC7A11/xCT at the crossroads of regulating redox homeostasis and nutrient dependency of cancer. _Cancer Commun._ 38, 12 (2018).
Article Google Scholar * Lee, W. N. et al. Mass isotopomer study of the nonoxidative pathways of the pentose cycle with [1,2-13C2]glucose. _Am. J. Physiol._ 274, E843–E851 (1998). Article
CAS PubMed Google Scholar * Fan, J. et al. Quantitative flux analysis reveals folate-dependent NADPH production. _Nature_ 510, 298–302 (2014). Article CAS PubMed PubMed Central
Google Scholar * Lewis, C. A. et al. Tracing compartmentalized NADPH metabolism in the cytosol and mitochondria of mammalian cells. _Mol. Cell._ 55, 253–263 (2014). Article CAS PubMed
PubMed Central Google Scholar * Shin, C. S. et al. The glutamate/cystine xCT antiporter antagonizes glutamine metabolism and reduces nutrient flexibility. _Nat. Commun._ 8, 15074 (2017).
Article PubMed PubMed Central Google Scholar * Koppula, P., Zhang, Y., Shi, J., Li, W. & Gan, B. The glutamate/cystine antiporter SLC7A11/xCT enhances cancer cell dependency on
glucose by exporting glutamate. _J. Biol. Chem._ 292, 14240–14249 (2017). Article CAS PubMed PubMed Central Google Scholar * Goji, T., Takahara, K., Negishi, M. & Katoh, H. Cystine
uptake through the cystine/glutamate antiporter xCT triggers glioblastoma cell death under glucose deprivation. _J. Biol. Chem._ 292, 19721–19732 (2017). Article CAS PubMed PubMed Central
Google Scholar * Vander Heiden, M. G., Cantley, L. C. & Thompson, C. B. Understanding the Warburg effect: the metabolic requirements of cell proliferation. _Science_ 324, 1029–1033
(2009). Article CAS Google Scholar * Bak, D. W., Bechtel, T. J., Falco, J. A. & Weerapana, E. Cysteine reactivity across the subcellular universe. _Curr. Opin. Chem. Biol._ 48, 96–105
(2019). Article CAS PubMed Google Scholar * Hay, N. Reprogramming glucose metabolism in cancer: can it be exploited for cancer therapy? _Nat. Rev. Cancer_ 16, 635–649 (2016). Article
CAS PubMed PubMed Central Google Scholar * Zhang, D. et al. 2-Deoxy-d-glucose targeting of glucose metabolism in cancer cells as a potential therapy. _Cancer Lett._ 355, 176–183 (2014).
Article CAS PubMed Google Scholar * Pereira, D. J., Schoolwerth, A. C. & Pais, V. M. Cystinuria: current concepts and future directions. _Clin. Nephrol_. 83, 138–146 (2015). Article
CAS PubMed Google Scholar * Elmonem, M. A. et al. Cystinosis: a review. _Orphanet J. Rare Dis._ 11, 47 (2016). Article PubMed PubMed Central Google Scholar * Siebeneicher, H. et al.
Identification and optimization of the first highly selective GLUT1 inhibitor BAY-876. _Chem. Med. Chem._ 11, 2261–2271 (2016). Article CAS PubMed Google Scholar * Jozwiak, P.,
Krzeslak, A., Pomorski, L. & Lipinska, A. Expression of hypoxia-related glucose transporters GLUT1 and GLUT3 in benign, malignant and non-neoplastic thyroid lesions. _Mol. Med. Rep._ 6,
601–606 (2012). Article CAS PubMed Google Scholar * Krzeslak, A. et al. Expression of GLUT1 and GLUT3 glucose transporters in endometrial and breast cancers. _Pathol. Oncol. Res._ 18,
721–728 (2012). Article CAS PubMed Google Scholar * Ancey, P. B., Contat, C. & Meylan, E. Glucose transporters in cancer—from tumor cells to the tumor microenvironment. _FEBS J._
285, 2926–2943 (2018). Article CAS PubMed Google Scholar * Faubert, B. et al. Lactate metabolism in human lung tumors. _Cell_ 171, 358–371 (2017). Article CAS PubMed PubMed Central
Google Scholar * Hui, S. et al. Glucose feeds the TCA cycle via circulating lactate. _Nature_ 551, 115–118 (2017). Article PubMed PubMed Central CAS Google Scholar * Sabharwal, S. S.
& Schumacker, P. T. Mitochondrial ROS in cancer: initiators, amplifiers or an Achilles’ heel? _Nat. Rev. Cancer_ 14, 709–721 (2014). Article CAS PubMed PubMed Central Google Scholar
* Shimada, K., Hayano, M., Pagano, N. C. & Stockwell, B. R. Cell-line selectivity improves the predictive power of pharmacogenomic analyses and helps identify NADPH asbiomarker for
ferroptosis sensitivity. _Cell Chem. Biol._ 23, 225–235 (2016). Article CAS PubMed PubMed Central Google Scholar * Zhang, Y., Koppula, P. & Gan, B. Regulation of H2A ubiquitination
and SLC7A11 expression by BAP1 and PRC1. _Cell Cycle_ 18, 773–783 (2019). Article CAS PubMed PubMed Central Google Scholar * Zhang, Y., Zhuang, L. & Gan, B. BAP1 suppresses tumor
development by inducing ferroptosis upon SLC7A11 repression. _Mol. Cell. Oncol._ 6, 1536845 (2019). Article PubMed CAS Google Scholar * Sykiotis, G. P. & Bohmann, D. Stress-activated
cap’n’collar transcription factors in aging and human disease. _Sci. Signal._ 3, re3 (2010). Article PubMed PubMed Central CAS Google Scholar * Rojo de la Vega, M., Chapman, E. &
Zhang, D. NRF2 and the hallmarks of cancer. _Cancer Cell_ 34, 21–43 (2018). Article CAS PubMed Google Scholar * Liu, X. et al. LncRNA NBR2 engages a metabolic checkpoint by regulating
AMPK under energy stress. _Nat. Cell Biol._ 18, 431–442 (2016). Article CAS PubMed PubMed Central Google Scholar * Gu, Y. et al. mTORC2 regulates amino acid metabolism in cancer by
phosphorylation of the cystine–glutamate antiporter xCT. _Mol. Cell_ 67, 128–138 (2017). Article CAS PubMed PubMed Central Google Scholar * Lin, A. et al. FoxO transcription factors
promote AKT Ser473 phosphorylation and renal tumor growth in response to pharmacological inhibition of the PI3K–AKT pathway. _Cancer Res._ 74, 1682–1693 (2014). Article CAS PubMed PubMed
Central Google Scholar * Dai, F. et al. BAP1 inhibits the ER stress gene regulatory network and modulates metabolic stress response. _Proc. Natl Acad. Sci. USA_ 114, 3192–3197 (2017).
Article CAS PubMed PubMed Central Google Scholar * Lin, A. et al. The FoxO–BNIP3 axis exerts a unique regulation of mTORC1 and cell survival under energy stress. _Oncogene_ 33,
3183–3194 (2014). Article CAS PubMed Google Scholar * Liu, X. & Gan, B. lncRNA NBR2 modulates cancer cell sensitivity to phenformin through GLUT1. _Cell Cycle_ 15, 3471–3481 (2016).
Article CAS PubMed PubMed Central Google Scholar * Jeon, S. M., Chandel, N. S. & Hay, N. AMPK regulates NADPH homeostasis to promote tumour cell survival during energy stress.
_Nature_ 485, 661–665 (2012). Article CAS PubMed PubMed Central Google Scholar * Xiao, Z. D. et al. Energy stress-induced lncRNA FILNC1 represses c-Myc-mediated energy metabolism and
inhibits renal tumor development. _Nat. Commun._ 8, 783 (2017). Article PubMed PubMed Central CAS Google Scholar * Chauhan, A. S. et al. STIM2 interacts with AMPK and regulates
calcium-induced AMPK activation. _FASEB J._ 33, 2957–2970 (2019). Article CAS PubMed Google Scholar * Gan, B. et al. Lkb1 regulates quiescence and metabolic homeostasis of haematopoietic
stem cells. _Nature_ 468, 701–704 (2010). Article CAS PubMed PubMed Central Google Scholar * Gan, B. et al. FoxOs enforce a progression checkpoint to constrain mTORC1-activated renal
tumorigenesis. _Cancer Cell_ 18, 472–484 (2010). Article CAS PubMed PubMed Central Google Scholar * Gan, B. et al. mTORC1-dependent and -independent regulation of stem cell renewal,
differentiation, and mobilization. _Proc. Natl Acad. Sci. USA_ 105, 19384–19389 (2008). Article CAS PubMed PubMed Central Google Scholar * Lu, W. et al. Metabolomic analysis via
reversed-phase ion-pairing liquid chromatography coupled to a stand alone orbitrap mass spectrometer. _Anal. Chem._ 82, 3212–3221 (2010). Article CAS PubMed PubMed Central Google Scholar
* Melamud, E., Vastag, L. & Rabinowitz, J. D. Metabolomic analysis and visualization engine for LC–MS data. _Anal. Chem._ 82, 9818–9826 (2010). Article CAS PubMed PubMed Central
Google Scholar * Wallace, M. et al. Enzyme promiscuity drives branched-chain fatty acid synthesis in adipose tissues. _Nat. Chem. Biol._ 14, 1021–1031 (2018). Article CAS PubMed PubMed
Central Google Scholar * Young, J. D. INCA: a computational platform for isotopically non-stationary metabolic flux analysis. _Bioinformatics_ 30, 1333–1335 (2014). Article CAS PubMed
PubMed Central Google Scholar * Heinrich, P. et al. Correcting for natural isotope abundance and tracer impurity in MS-, MS/MS- and high-resolution-multiple-tracer-data from stable isotope
labeling experiments with IsoCorrectoR. _Sci. Rep._ 8, 17910 (2018). Article CAS PubMed PubMed Central Google Scholar * Badur, M. G. et al. Oncogenic R132 IDH1 mutations limit NADPH
for de novo lipogenesis through (D)2-hydroxyglutarate production in fibrosarcoma cells. _Cell Rep_. 25, 1018–1026 (2018). Article CAS PubMed PubMed Central Google Scholar * Lu, W.,
Wang, L., Chen, L., Hui, S. & Rabinowitz, J. D. Extraction andquantitation of nicotinamide adenine dinucleotide redox cofactors. _Antioxid. Redox Signal._ 28, 167–179 (2018). Article
CAS PubMed PubMed Central Google Scholar * Su, X., Lu, W. & Rabinowitz, J. D. Metabolite spectral accuracy on orbitraps. _Anal. Chem._ 89, 5940–5948 (2017). Article CAS PubMed
PubMed Central Google Scholar * Yan, X. et al. Inhibition of thioredoxin/thioredoxin reductase induces synthetic lethality in lung cancers with compromised glutathione homeostasis. _Cancer
Res_. 79, 125–132 (2019). Article CAS PubMed Google Scholar * Lee, H. et al. BAF180 regulates cellular senescence and hematopoietic stem cell homeostasis through p21. _Oncotarget_ 7,
19134–19146 (2016). Article PubMed PubMed Central Google Scholar * Gan, B. et al. Role of FIP200 in cardiac and liver development and its regulation of TNFα and TSC–mTOR signaling
pathways. _J. Cell Biol._ 175, 121–133 (2006). Article CAS PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS We thank R. DePinho for critical reading and
insightful comments. This research has been supported by the Andrew Sabin Family Fellow Award and Bridge Fund from The University of Texas MD Anderson Cancer Center, Career Enhancement Award
from University of Texas Specialized Program of Research Excellence in Lung Cancer National Institutes of Health/National Cancer Institute 5P50CA070907, KC180131 from Department of Defense
Kidney Cancer Research Program (to B.G.), grants from the National Institutes of Health (R01CA181196 to B.G. and R01CA188652 to C.M.M.). B.G. is an Andrew Sabin Family Fellow. Y.Z. and P.K.
were Scholars at the Center for Cancer Epigenetics at The University of Texas MD Anderson Cancer Center. P.K. is also supported by the CPRIT Research Training Grant (RP170067) and Dr. John
J. Kopchick Research Award from The MD Anderson UTHealth Graduate School of Biomedical Sciences. E.W.L. is supported by National Institutes of Health grant T32EB009380. PDX generation and
annotation were supported by the University of Texas MD Anderson Cancer Center Moon Shots Program, Specialized Program of Research Excellence grant CA070907 and University of Texas PDX
Development and Trial Center grant U54CA224065. This research was also supported by the National Institutes of Health Cancer Center Support Grant P30CA016672 to The University of Texas MD
Anderson Cancer Center. AUTHOR INFORMATION Author notes * These authors contributed equally: Xiaoguang Liu, Kellen Olszewski, Yilei Zhang. AUTHORS AND AFFILIATIONS * Department of
Experimental Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, TX, USA Xiaoguang Liu, Yilei Zhang, Jie Zhang, Hyemin Lee, Pranavi Koppula, Guang Lei, Li Zhuang
& Boyi Gan * Kadmon Corporation, New York, NY, USA Kellen Olszewski & Masha V. Poyurovsky * Department of Bioengineering, University of California, San Diego, La Jolla, CA, USA
Esther W. Lim & Christian M. Metallo * Division of Biostatistics, Dan L. Duncan Cancer Center and Department of Molecular and Cellular Biology, Baylor College of Medicine, Houston, TX,
USA Jiejun Shi & Wei Li * Department of Thoracic and Cardiovascular Surgery, The University of Texas MD Anderson Cancer Center, Houston, TX, USA Xiaoshan Zhang & Bingliang Fang * The
University of Texas MD Anderson UTHealth Graduate School of Biomedical Sciences, Houston, TX, USA Pranavi Koppula & Boyi Gan * Department of Hematopathology, The University of Texas MD
Anderson Cancer Center, Houston, TX, USA M. James You Authors * Xiaoguang Liu View author publications You can also search for this author inPubMed Google Scholar * Kellen Olszewski View
author publications You can also search for this author inPubMed Google Scholar * Yilei Zhang View author publications You can also search for this author inPubMed Google Scholar * Esther W.
Lim View author publications You can also search for this author inPubMed Google Scholar * Jiejun Shi View author publications You can also search for this author inPubMed Google Scholar *
Xiaoshan Zhang View author publications You can also search for this author inPubMed Google Scholar * Jie Zhang View author publications You can also search for this author inPubMed Google
Scholar * Hyemin Lee View author publications You can also search for this author inPubMed Google Scholar * Pranavi Koppula View author publications You can also search for this author
inPubMed Google Scholar * Guang Lei View author publications You can also search for this author inPubMed Google Scholar * Li Zhuang View author publications You can also search for this
author inPubMed Google Scholar * M. James You View author publications You can also search for this author inPubMed Google Scholar * Bingliang Fang View author publications You can also
search for this author inPubMed Google Scholar * Wei Li View author publications You can also search for this author inPubMed Google Scholar * Christian M. Metallo View author publications
You can also search for this author inPubMed Google Scholar * Masha V. Poyurovsky View author publications You can also search for this author inPubMed Google Scholar * Boyi Gan View author
publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS X.L. and Y.Z. performed most of the experiments with assistance from P.K., G.L, L.Z. and H.L. K.O.
conducted most metabolomic and isotope-tracing analyses except 3-[2H]glucose-tracing analyses. E.W.L. performed 3-[2H]glucose tracing analyses under the direction of C.M.M. J.S. conducted
bioinformatics analysis under the direction of W.L. X.Z. and B.F. provided PDXs. J.Z. processed tumour and tissue samples. M.J.Y. performed histopathological analysis. K.O. and M.V.P.
provided KL-11743 and designed and interpreted pharmacokinetic analysis. B.G. conceived and supervised the study and wrote most of the manuscript. All authors commented on the manuscript.
CORRESPONDING AUTHOR Correspondence to Boyi Gan. ETHICS DECLARATIONS COMPETING INTERESTS K.O. and M.V.P. are full-time employees of Kadmon Corporation. The other authors declare no competing
interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. EXTENDED DATA
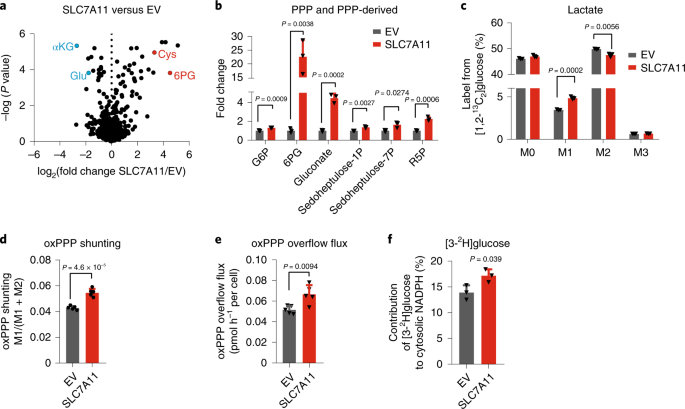
EXTENDED DATA FIG. 1 THE EFFECT OF SLC7A11 OVEREXPRESSION ON GLUTAMATE, TCA CYCLE AND GLYCOLYSIS METABOLITES, AND THE EXPRESSION LEVELS OF PPP ENZYMES. A, Western blotting showing Myc-tagged
SLC7A11 expression in 786-O cells. The experiment was repeated five times, independently, with similar results. B, Bar graph showing relative fold changes of glutamate and TCA cycle
metabolites in EV and SLC7A11-overexpressing 786-O cells. n=3 independent experiments. C, Western blotting showing indicated protein levels in EV and SLC7A11-overexpressing 786-O cells. The
experiment was repeated twice, independently, with similar results. D, Bar graph showing relative fold changes of glycolysis metabolites in EV and SLC7A11-overexpressing 786-O cells. n=3
independent experiments. E,F, Bar graph showing the fold changes of PPP and PPP-derived intermediates induced by SLC7A11 overexpression in RCC4 or ACHN cells. n=3 independent experiments. G,
Simplified schematic of glycolysis and the PPP, showing 13C labeling patterns resulting from 1,2-13C2 glucose. Red fills indicate 13C atoms. H, Glucose consumption rates in EV and
SLC7A11-overexpressing 786-O cells. n=5 independent experiments. I, Simplified schematic showing the sequential transfer of deuterium labels at position 3 of glucose to NADPH and then newly
synthesized palmitic acid. Red circles indicate positional deuterium labels. J, Newly synthesized deuterium labelled palmitate in EV and SLC7A11-overexpressing 786-O cells. n=3 independent
experiments. In (J), data are plotted as mean ±95% confidence interval (CI). Other error bars are mean ± s.d. All p values were calculated using two-tailed unpaired Student’s t-test.
Detailed statistical tests are described in the Methods. Scanned images of unprocessed blots are shown in Source Data Extended Data Fig. 1. Numeral data are provided in Statistics Source
Data Extended Data Fig. 1. Source data EXTENDED DATA FIG. 2 G6PD KNOCKDOWN SENSITIZES CANCER CELLS TO GLUCOSE LIMITATION AND SLC7A11 EXPRESSION CORRELATES WITH PPP GENE EXPRESSION IN HUMAN
CANCERS. A, C, G6PD protein levels in control shRNA (shCtrl) and _G6PD_ knockdown (shG6PD) UMRC6 (A) and A498 cells (C). The experiments were repeated twice, independently, with similar
results. Scanned images of unprocessed blots are shown in Source Data Extended Data Fig. 2. B, D, Cell death analysed by PI staining in indicated cells cultured in 25 or 1 mM glucose for 24
hours. Error bars are mean± s.d., n=3 independent experiments, p values were calculated using two-tailed unpaired Student’s t-test. E, Compared to other glucose metabolism genes, PPP genes
show significant positive correlations with _SLC7A11_ in LUAD(n=514), BLCA(n=407), HNSC(n=520), CHOL(n=36), ESCA(n=184), LUSC(n=502), and LIHC(n=371). F, Scatter plots showing the
correlations between _SLC7A11_ and 4 PPP genes (_G6PD_, _PGD_, _TALDO1_, and _TKT_) in KIRC(n=533), LUAD(n=514), and LUSC(n=502), respectively. G, Scatter plots showing the correlations
between _SLC7A11_ and _SLC2A1_ in KIRP(n=290).H, Kaplan–Meier plots of KIRP patients stratified by _SLC7A11_ and _SLC2A1_ expression levels, respectively (left 2 panels); Kaplan–Meier plots
of KIRP patients stratified by unsupervised clustering on _SLC7A11_ and _SLC2A1_ expression (right 2 panels). Group 1 has lower _SLC7A11_ and _SLC2A1_ expression, while Group 2 has higher
_SLC7A11_ and _SLC2A1_ expression. Detailed statistical tests of B, D and F-H are described in the Methods. Error bars are mean ± s.d, all bar graphs have 3 independent repeats. Numeral data
are provided in Statistics Source Data Extended Data Fig. 2. Source data EXTENDED DATA FIG. 3 HIGH EXPRESSION OF SLC7A11 PROMOTE DISULFIDE STRESS, DEPLETE NADPH AND CAUSES REDOX SYSTEM
COLLAPSE UNDER GLUCOSE DEPRIVATION. A, Simplified schematic of how SLC7A11 can be linked to NADPH and the PPP. B, C, Measurement of intracellular GSSG (B) and GSH (C) concentrations in EV
and SLC7A11-overexpressing 786-O cells cultured with (+Glc) or without glucose (-Glc). D, Diagrams illustrating the structures of γ-glutamylcysteine, γ-glutamyl-cystine, GSH, and
glutathionyl-cysteine. Glu: glutamate; Gly: glycine; Cys: cysteine. E, F, The relative levels of intracellular γ-glutamyl-cystine (E) and glutathionyl-cysteine (F) in EV and
SLC7A11-overexpressing 786-O cells cultured with (+Glc) or without glucose (-Glc). G, Representative phase-contrast images of indicated cells cultured with or without glucose.H, Western
blotting analysis of SLC7A11 protein levels in the control (sgCtrl) and _SLC7A11_ knockout (sgSLC-1/2) UMRC6 cells. I-L, Measurement of intracellular GSSG (I) and GSH (J) concentrations and
the relative levels of intracellular γ-glutamyl-cystine (K) and glutathionyl-cysteine (L) in control (sgCtrl) and _SLC7A11_ knockout (sgSLC-1/2) UMRC6 cells cultured with (+Glc) or without
glucose (-Glc). M, Representative phase-contrast images of indicated cells cultured with (+Glc) or without glucose (-Glc). N, O, Cystine uptake levels in EV and SLC7A11- overexpressing 786-O
cells (N) or UMRC6 cells (O) upon treatment with 1 mM sulfasalazine (SAS). P-U, Cell death with or without representative phase-contrast images (P, S), NADP+/NADPH ratios (Q, T), and ROS
levels (R, U) of EV and SLC7A11- overexpressing 786-O or UMRC6 cells cultured in glucose-containing or glucose free medium with or without treatment of 1 mM SAS. Error bars are mean ± s.d,
all bar graphs have 3 independent repeats. All scale bars=100 μm. The experiment (G, H, M, P) was repeated twice, independently, with similar results. All p values were calculated using
two-tailed unpaired Student’s t-test. Scanned images of unprocessed blots are shown in Source Data Extended Data Fig. 3. Numeral data are provided in Statistics Source Data Extended Data
Fig. 3. Source data EXTENDED DATA FIG. 4 CYSTINE DEPRIVATION OR 2DG REVERSES REDOX DEFECTS AND PREVENTS CELL DEATH UPON GLUCOSE STARVATION. A-D, Measurement of intracellular GSSG (A) and GSH
(B) concentrations, and the relative levels of intracellular γ-glutamyl-cystine (C) and glutathionyl-cysteine (D) in UMRC6 cells cultured with normal (+Glc), glucose free (-Glc),
glucose/cystine-double free (-Glc-Cystine), or cystine free (-Cystine) medium. E, F, Measurement of NADP+/NADPH ratios (E), and ROS levels (F) in EV and SLC7A11-overexpressing 786-O cells
cultured with indicated medium. G-I, Representative phase-contrast images and cell death of indicated cells cultured with indicated medium. J, K, Diagrams illustrating the structure (J) and
metabolism (K) of glucose and 2DG. L-N, The relative levels of intracellular 2-deoxyglucose-6-phosphate (L), 2-deoxy-6-phosphogluconolactone (M) and 2-deoxy-6-phosphogluconate (N) in UMRC6
cells cultured in glucose-containing or glucose free medium with or without treatment of 2 mM 2DG. O-R, Measurement of intracellular GSSG (O) and GSH (P) concentrations, and the relative
levels of intracellular γ-glutamyl-cystine (Q) and glutathionyl-cysteine (R) in UMRC6 cells cultured in glucose-containing or glucose free medium with or without treatment of 2 mM 2DG. S,
Representative phase-contrast images of UMRC6 cells cultured in glucose-containing or glucose free medium with or without treatment of 2 mM 2DG.T-W, Measurement of NADP+/NADPH ratios (T),
ROS levels (U), cell death (V) and the representative phase-contrast images (W) of EV and SLC7A11-overexpressing 786-O cells cultured in glucose-containing or glucose-free medium with or
without treatment of 2 mM 2DG. The experiments (G, H, I, S, W) were repeated twice, independently, with similar results. All error bars are mean± s.d., n=3 independent experiments. All scale
bars=100 μm. All p values were calculated using two-tailed unpaired Student’s t-test. Numeral data are provided in Statistics Source Data Extended Data Fig. 4. Source data EXTENDED DATA
FIG. 5 PREVENTING DISULFIDE BUT NOT ROS ACCUMULATION RESCUES REDOX DEFECTS AND CELL DEATH IN SLC7A11-OVEREXPRESSING CELLS UNDER GLUCOSE STARVATION. A, B, Measurement of cell death of UMRC6
or 786-O cells cultured in glucose-containing, glucose-free medium or cystine-free medium with or without treatment of 100 μM DFO or 10 μM Ferrostatin-1. C–H, Measurement intracellular
levels of cysteine (C), the relative levels of intracellular γ-glutamyl-cystine (D), glutathionyl-cysteine (E), NAC-cysteine (F), GSSG/GSH ratio (G) and ROS levels (H) of UMRC6 cells
cultured in glucose-containing or glucose-free medium with or without treatment of 2 mM NAC. I, The solubility of different amino acids. J–O, Measurement intracellular levels of cysteine
(J), the relative levels of intracellular γ-glutamyl-cystine (K), glutathionyl-cysteine (L), GSSG/GSH ratio (M), ROS levels (N) and Cysteine-penicillamine (O) of UMRC6 cells cultured in
glucose-containing or glucose-free medium with or without treatment of 2 mM D-Penicillamine or L-Penicillamine. P–T, Measurement intracellular levels of cysteine (P), the relative levels of
intracellular γ-glutamyl-cystine (Q), glutathionyl-cysteine (R), GSSG/GSH ratio (S) and ROS levels (T) of UMRC6 cells cultured in glucose-containing or glucose-free medium with or without
treatment of TCEP. U-Y, Measurement intracellular levels of cysteine (U), the relative levels of intracellular γ-glutamyl-cystine (V), glutathionyl-cysteine (W), GSSG/GSH ratio (X) and ROS
levels (Y) of UMRC6 cells cultured in glucose-containing or glucose-free medium with or without treatment of 1 mM 2ME. Except I, all other error bars are mean± s.d., n=3 independent
experiments. All p values were calculated using two-tailed unpaired Student’s t-test. Detailed statistical tests are described in the Methods. Numeral data are provided in Statistics Source
Data Extended Data Fig. 5. Source data EXTENDED DATA FIG. 6 CANCER CELLS WITH HIGH SLC7A11 EXPRESSION ARE SENSITIVE TO GLUT INHIBITION. A, Cell death of EV and SLC7A11- overexpressing 786-O
cells treated with 0.125-0.5 mM 6-AN. B, Cell death of EV and SLC7A11- overexpressing 786-O cells treated with 0.1 mM epiandrosterone (EA). C, Quantification of NADP+/NADPH ratios in EV and
_SLC7A11_- overexpressing 786-O cells treated with normal (+Glc), glucose free (-Glc) medium, or normal medium containing 0.1 mM EA. D, Quantification of NADP+/NADPH ratios in UMRC6 cells
treated with normal (+Glc), glucose free (-Glc), glucose/cystine double free medium (-Glc-Cystine), or normal medium containing 0.1 mM EA. E, SLC7A11 protein levels in control (sgCtrl) and
_SLC7A11_ knockout (sgSLC7A11) NCI-H226 cells were measured by western blotting. The experiment was repeated twice, independently, with similar results. F, Measurement of GSSG/GSH ratios in
EV and SLC7A11-overexpressing 786-O cells treated with KL-11743, BAY-876 or cultured in glucose free medium. G, Western blotting analysis of indicated proteins in ACHN cells with SLC7A11
and/or G6PD overexpression. The experiment was repeated twice, independently, with similar results. All error bars are mean± s.d., n=3 independent experiments. All p values were calculated
using two-tailed unpaired Student’s t-test. Detailed statistical tests are described in the Methods. Scanned images of unprocessed blots are shown in Source Data Extended Data Fig. 6.
Numeral data are provided in Statistics Source Data Extended Data Fig. 6. Source data EXTENDED DATA FIG. 7 SLC7A11-HIGH TUMORS ARE SENSITIVE TO GLUT INHIBITOR. A, Plasma levels of GLUT
inhibitor KL-11743 were measured in mice at different time points after intraperitoneal injection. Error bars are mean ± s.d, n=4 independent repeats. B, End-point weights of NCI-H226
xenograft tumors with indicated genotypes treated with KL-11743 or vehicle. Error bars are mean ± s.d., n=9 independent repeats. C, End-point weights of ACHN xenograft tumors with indicated
genotypes treated with BAY-876, KL-11743, or vehicle. Error bars are mean ± s.d., n=8 independent repeats. D-H, End-point weights of PDX xenograft tumors with indicated genotypes treated
with KL-11743 or vehicle. . Error bars are mean ± s.d., n=6 (D: KL-11743, F-H) or7 (D: vehicle, E) independent repeats. I, Representative hematoxylin and eosin staining of major organs from
mice treated with vehicle or GLUT inhibitors. The experiment was repeated twice, independently, with similar results. Scale bars=50 μm. J-P, Mice weights of indicated cell line-xenografts or
PDXs at different time points treated with KL-11743 or vehicle. Error bars are mean ± s.d., n=6 (L: KL-11743, N-P), 7 (L: vehicle, M), 8 (K) or 9 (J) independent repeats. All p values were
calculated using two-tailed unpaired Student’s t-test. Detailed statistical tests are described in the Methods. Numeral data are provided in Statistics Source Data Extended Data Fig. 7.
Source data EXTENDED DATA FIG. 8 THE WORKING MODEL DEPICTING HOW SLC7A11 REGULATES PENTOSE PHOSPHATE PATHWAY DEPENDENCY AND GLUCOSE-DEPRIVATION-INDUCED CELL DEATH. See discussion for
detailed description. PPP: pentose phosphate pathway; GLUT: glucose transporter. EXTENDED DATA FIG. 9 AN EXAMPLE FOR THE GATING STRATEGY OF FLOW CYTOMETRY. Initial cell population gating
(FSC-Area VS FSC-Height) was adopted to make sure only single cells were used for analysis. SUPPLEMENTARY INFORMATION REPORTING SUMMARY SUPPLEMENTARY INFORMATION Supplementary Table 1:
glucose metabolism related genes. Supplementary Table 2: summary of various approaches on rescuing redox defects and cell death in SLC7A11-high cancer cells under glucose starvation.
Supplementary Table 3: oligos and shRNA sequences. Supplementary Table 4: information on human research participants (age, gender, genotypic information, diagnosis and treatment categories)
of PDXs in this study. SOURCE DATA SOURCE DATA FIG. 1 Statistical source data SOURCE DATA FIG. 2 Statistical source data SOURCE DATA FIG. 2 Unprocessed western blots SOURCE DATA FIG. 3
Statistical source data SOURCE DATA FIG. 4 Statistical source data SOURCE DATA FIG. 5 Statistical source data SOURCE DATA FIG. 6 Statistical source data SOURCE DATA FIG. 6 Unprocessed
western blots SOURCE DATA EXTENDED DATA FIG. 1 Statistical source data SOURCE DATA EXTENDED DATA FIG. 1 Unprocessed western blots SOURCE DATA EXTENDED DATA FIG. 2 Statistical source data
SOURCE DATA EXTENDED DATA FIG. 2 Unprocessed western blots SOURCE DATA EXTENDED DATA FIG. 3 Statistical source data SOURCE DATA EXTENDED DATA FIG. 3 Unprocessed western blots SOURCE DATA
EXTENDED DATA FIG. 4 Statistical source data SOURCE DATA EXTENDED DATA FIG. 5 Statistical source data SOURCE DATA EXTENDED DATA FIG. 6 Statistical source data SOURCE DATA EXTENDED DATA FIG.
6 Unprocessed western blots SOURCE DATA EXTENDED DATA FIG. 7 Statistical source data RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Liu, X., Olszewski,
K., Zhang, Y. _et al._ Cystine transporter regulation of pentose phosphate pathway dependency and disulfide stress exposes a targetable metabolic vulnerability in cancer. _Nat Cell Biol_ 22,
476–486 (2020). https://doi.org/10.1038/s41556-020-0496-x Download citation * Received: 21 August 2019 * Accepted: 28 February 2020 * Published: 30 March 2020 * Issue Date: April 2020 *
DOI: https://doi.org/10.1038/s41556-020-0496-x SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is
not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
