Platelet biology and functions: new concepts and clinical perspectives
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

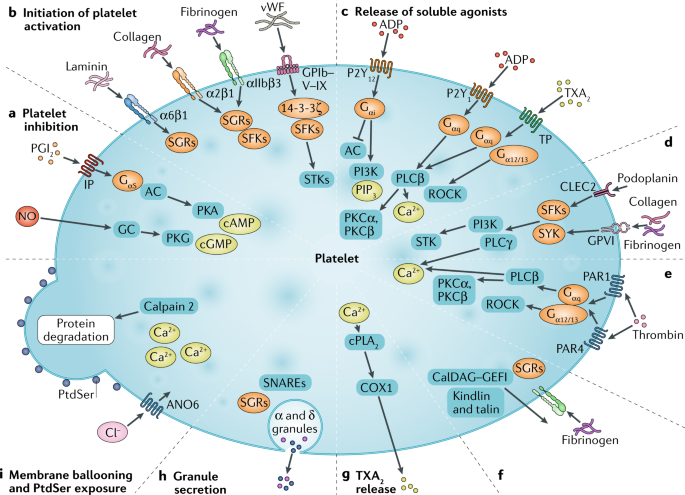
ABSTRACT Platelets — blood cells continuously produced from megakaryocytes mainly in the bone marrow — are implicated not only in haemostasis and arterial thrombosis, but also in other
physiological and pathophysiological processes. This Review describes current evidence for the heterogeneity in platelet structure, age, and activation properties, with consequences for a
diversity of platelet functions. Signalling processes of platelet populations involved in thrombus formation with ongoing coagulation are well understood. Genetic approaches have provided
information on multiple genes related to normal haemostasis, such as those encoding receptors and signalling or secretory proteins, that determine platelet count and/or responsiveness. As
highly responsive and secretory cells, platelets can alter the environment through the release of growth factors, chemokines, coagulant factors, RNA species, and extracellular vesicles.
Conversely, platelets will also adapt to their environment. In disease states, platelets can be positively primed to reach a pre-activated condition. At the inflamed vessel wall, platelets
interact with leukocytes and the coagulation system, interactions mediating thromboinflammation. With current antiplatelet therapies invariably causing bleeding as an undesired adverse
effect, novel therapies can be more beneficial if directed against specific platelet responses, populations, interactions, or priming conditions. On the basis of these novel concepts and
processes, we discuss several initiatives to target platelets therapeutically. KEY POINTS * Multiomic approaches combined with functional testing of platelets have greatly advanced the
understanding of genetic factors of platelet-related haemorrhagic disorders, but to a lesser extent the understanding of the causes of platelet hyper-reactivity. * Negative and positive
platelet priming alter the threshold for platelet activation in the circulation, with consequences for diagnostic assays. * The diverse pathways of information transfer by platelets through
release of bioactive molecules and extracellular vesicles are still incompletely understood. * Platelets contribute to thromboinflammatory processes by their capacity to interact
functionally with the activated endothelium, leukocytes, and coagulation proteins; the mechanisms are multivariate. * Platelet populations and specific platelet responses are promising
targets for new antithrombotic treatment of patients with cardiovascular disease. Access through your institution Buy or subscribe This is a preview of subscription content, access via your
institution ACCESS OPTIONS Access through your institution Access Nature and 54 other Nature Portfolio journals Get Nature+, our best-value online-access subscription $29.99 / 30 days cancel
any time Learn more Subscribe to this journal Receive 12 print issues and online access $209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink *
Instant access to full article PDF Buy now Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional
subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS PLATELETS AND DISEASES: SIGNAL TRANSDUCTION AND ADVANCES IN TARGETED THERAPY Article Open
access 16 May 2025 A GUIDE TO MOLECULAR AND FUNCTIONAL INVESTIGATIONS OF PLATELETS TO BRIDGE BASIC AND CLINICAL SCIENCES Article 03 March 2022 PLATELET-PRIMED INTERACTIONS OF COAGULATION AND
ANTICOAGULATION PATHWAYS IN FLOW-DEPENDENT THROMBUS FORMATION Article Open access 17 July 2020 REFERENCES * Quach, M. E., Chen, W. & Li, R. Mechanisms of platelet clearance and
translation to improve platelet storage. _Blood_ 131, 1512–1521 (2018). CAS PubMed PubMed Central Google Scholar * Lefrancais, E. et al. The lung is a site of platelet biogenesis and a
reservoir for haematopoietic progenitors. _Nature_ 544, 105–109 (2017). CAS PubMed PubMed Central Google Scholar * Stegner, D. et al. Thrombopoiesis is spatially regulated by the bone
marrow vasculature. _Nat. Commun._ 8, 127 (2017). PubMed PubMed Central Google Scholar * Grozovsky, R., Giannini, S., Falet, H. & Hoffmeister, K. M. Regulating billions of blood
platelets: glycans and beyond. _Blood_ 126, 1877–1884 (2015). CAS PubMed PubMed Central Google Scholar * Kaser, A. et al. Interleukin-6 stimulates thrombopoiesis through thrombopoietin:
role in inflammatory thrombocytosis. _Blood_ 98, 2720–2725 (2001). CAS PubMed Google Scholar * den Dekker, E. et al. Cell-to-cell variability in the differentiation program of human
megakaryocytes. _Biochim. Biophys. Acta_ 1643, 85–94 (2003). Google Scholar * Moreau, T. et al. Large-scale production of megakaryocytes from human pluripotent stem cells by chemically
defined forward programming. _Nat. Commun._ 7, 11208 (2016). CAS PubMed PubMed Central Google Scholar * Machlus, K. R. & Italiano, J. E. Jr. The incredible journey: From
megakaryocyte development to platelet formation. _J. Cell Biol._ 201, 785–796 (2013). CAS PubMed PubMed Central Google Scholar * Bender, M. et al. Microtubule sliding drives proplatelet
elongation and is dependent on cytoplasmic dynein. _Blood_ 125, 860–868 (2015). CAS PubMed PubMed Central Google Scholar * Josefsson, E. C. et al. Platelet production proceeds
independently of the intrinsic and extrinsic apoptosis pathways. _Nat. Commun._ 5, 3455 (2014). PubMed Google Scholar * Semeniak, D. et al. Proplatelet formation is selectively inhibited
by collagen type I through Syk-independent GPVI signaling. _J. Cell Sci._ 129, 3473–3484 (2016). CAS PubMed Google Scholar * Abbonante, V. et al. A new path to platelet production through
matrix sensing. _Haematologica_ 102, 1150–1160 (2017). CAS PubMed PubMed Central Google Scholar * Shi, D. S. et al. Proteasome function is required for platelet production. _J. Clin.
Invest._ 124, 3757–3766 (2014). CAS PubMed PubMed Central Google Scholar * McArthur, K., Chappaz, S. & Kile, B. T. Apoptosis in megakaryocytes and platelets: the life and death of a
lineage. _Blood_ 131, 605–610 (2018). CAS PubMed Google Scholar * Mason, K. D. et al. Programmed anuclear cell death delimits platelet life span. _Cell_ 128, 1173–1186 (2007). CAS PubMed
Google Scholar * Alhasan, A. A. et al. Circular RNA enrichment in platelets is a signature of transcriptome degradation. _Blood_ 127, e1–e11 (2016). CAS PubMed PubMed Central Google
Scholar * Male, R., Moon, D. G., Garvey, J. S., Vannier, W. E. & Baldeschwieler, J. D. Organ distributions of liposome-loaded rat platelets. _Biochem. Biophys. Res. Commun._ 195,
276–281 (1993). CAS PubMed Google Scholar * Karpatkin, S. Heterogeneity of human platelets. I. Metabolic and kinetic evidence suggestive of young and old platelets. _J. Clin. Invest._ 48,
1073–1082 (1969). CAS PubMed PubMed Central Google Scholar * Vicic, W. J. & Weiss, H. J. Evidence that platelet α-granules are a major determinant of platelet density: studies in
storage pool deficiency. _Thromb. Haemost._ 50, 878–880 (1983). CAS PubMed Google Scholar * Savage, B., McFadden, P. R., Hanson, S. R. & Harker, L. A. The relation of platelet density
to platelet age: survival of low- and high-density 111indium-labeled platelets in baboons. _Blood_ 68, 386–393 (1986). CAS PubMed Google Scholar * Freson, K. et al. Platelet
characteristics in patients with X-linked macrothrombocytopenia because of a novel GATA1 mutation. _Blood_ 98, 85–92 (2001). CAS PubMed Google Scholar * Baaten, C. C. F. M. J., Ten Cate,
H., van der Meijden, P. E. J. & Heemskerk, J. W. M. Platelet populations and priming in hematological diseases. _Blood Rev._ 31, 389–399 (2017). PubMed Google Scholar * Heemskerk, J.
W. M., Mattheij, N. & Cosemans, J. M. E. M. Platelet-based coagulation: different populations, different functions. _J. Thromb. Haemost._ 11, 2–11 (2013). CAS PubMed Google Scholar *
Jackson, S. P. & Schoenwaelder, S. M. Procoagulant platelets — are they necrotic? _Blood_ 116, 2011–2018 (2010). CAS PubMed Google Scholar * Mattheij, N. J. et al. Coated platelets
function in platelet-dependent fibrin formation via integrin αIIbβ3 and transglutaminase factor XIII. _Haematologica_ 101, 427–436 (2016). CAS PubMed PubMed Central Google Scholar *
Agbani, E. O. et al. Coordinated membrane ballooning and procoagulant spreading in human platelets. _Circulation_ 132, 1414–1424 (2015). CAS PubMed Google Scholar * Vogler, M. et al.
BCL2/BCL-XL inhibition induces apoptosis, disrupts cellular calcium homeostasis and prevents platelet activation. _Blood_ 117, 7145–7154 (2011). CAS PubMed Google Scholar * Schubert, S.,
Weyrich, A. S. & Rowley, J. W. A tour through the transcriptional landscape of platelets. _Blood_ 124, 493–502 (2014). CAS PubMed PubMed Central Google Scholar * Pleines, I. et al.
Extended platelet in vivo survival results in exhausted platelets. _Blood_ 126, 416 (2015). Google Scholar * Pleines, I. et al. Intrinsic apoptosis circumvents the functional decline of
circulating platelets but does not cause the storage lesion. _Blood_ 132, 197–209 (2018). CAS PubMed Google Scholar * McManus, D. D. & Freedman, J. E. MicroRNAs in platelet function
and cardiovascular disease. _Nat. Rev. Cardiol._ 12, 711–717 (2015). CAS PubMed Google Scholar * Rowley, J. W. et al. Dicer1-mediated miRNA processing shapes the mRNA profile and function
of murine platelets. _Blood_ 127, 1743–1751 (2016). CAS PubMed PubMed Central Google Scholar * Clancy, L., Beaulieu, L. M., Tanriverdi, K. & Freedman, J. E. The role of RNA uptake
in platelet heterogeneity. _Thromb. Haemost._ 117, 948–961 (2017). PubMed Google Scholar * Burkhart, J. M. et al. The first comprehensive and quantitative analysis of human platelet
protein composition allows the comparative analysis of structural and functional pathways. _Blood_ 120, e73–82 (2012). CAS PubMed Google Scholar * Zeiler, M., Moser, M. & Mann, M.
Copy number analysis of the murine platelet proteome spanning the complete abundance range. _Mol. Cell. Proteom._ 13, 3435–3445 (2014). CAS Google Scholar * Solari, F. A. et al. Combined
quantification of the global proteome, phosphoproteome and protein cleavage to characterize altered platelet functions in the human Scott syndrome. _Mol. Cell. Proteom._ 15, 3154–3169
(2016). CAS Google Scholar * Schoenwaelder, S. M. et al. 14-3-3ζ regulates the mitochondrial respiratory reserve linked to platelet phosphatidylserine exposure and procoagulant function.
_Nat. Commun._ 7, 12862 (2016). CAS PubMed PubMed Central Google Scholar * Versteeg, H. H., Heemskerk, J. W. M., Levi, M. & Reitsma, P. S. New fundamentals in hemostasis. _Physiol.
Rev._ 93, 327–358 (2013). CAS PubMed Google Scholar * Jackson, S. P. Arterial thrombosis: insidious, unpredictable and deadly. _Nat. Med._ 17, 1423–1436 (2011). CAS PubMed Google
Scholar * Mastenbroek, T. G., van Geffen, J. P., Heemskerk, J. W. M. & Cosemans, J. M. E. M. Acute and persistent platelet and coagulant activities in atherothrombosis. _J. Thromb.
Haemost._ 13 (Suppl. 1), S272–S280 (2015). CAS PubMed Google Scholar * Shekhonin, B. V., Domogatsky, S. P., Muzykantov, V. R., Idelson, G. L. & Rukosuev, V. S. Distribution of type I,
III, IV and V collagen in normal and atherosclerotic human arterial wall: immunomorphological characteristics. _Coll. Relat. Res._ 5, 355–368 (1985). CAS PubMed Google Scholar * De Witt,
S. M. et al. Identification of platelet function defects by multi-parameter assessment of thrombus formation. _Nat. Commun._ 5, 4257 (2014). PubMed Google Scholar * Swieringa, F., Spronk,
H. M. H., Heemskerk, J. W. M. & van der Meijden, P. E. J. Integrating platelet and coagulation activation in fibrin clot formation. _Res. Pract. Thromb. Haemost._ 2, 450–460 (2018). CAS
PubMed PubMed Central Google Scholar * Dubois, C., Panicot-Dubois, L., Merrill-Skoloff, G., Furie, B. & Furie, B. C. Glycoprotein VI-dependent and -independent pathways of thrombus
formation in vivo. _Blood_ 107, 3902–3906 (2006). CAS PubMed PubMed Central Google Scholar * Zhu, S., Lu, Y., Sinno, T. & Diamond, S. L. Dynamics of thrombin generation and flux from
clots during whole human blood flow over collagen/tissue factor surfaces. _J. Biol. Chem._ 291, 23027–23035 (2016). CAS PubMed PubMed Central Google Scholar * Zilberman-Rudensko, J. et
al. Coagulation factor XI promotes distal platelet activation and single platelet consumption in the bloom stream under shear flow. _Arterioscler. Thromb. Vasc. Biol._ 36, 510–517 (2016).
Google Scholar * Morowski, M. et al. Only severe thrombocytopenia results in bleeding and defective thrombus formation in mice. _Blood_ 121, 4938–4947 (2013). CAS PubMed Google Scholar *
Boulaftali, Y., Hess, P. R., Kahn, M. L. & Bergmeier, W. Platelet immunoreceptor tyrosine-based activation motif (ITAM) signaling and vascular integrity. _Circ. Res._ 114, 1174–1184
(2014). CAS PubMed PubMed Central Google Scholar * Van Gestel, M. et al. Real-time detection of activation patterns in individual platelets during thromboembolism in vivo: differences
between thrombus growth and embolus formation. _J. Vasc. Res._ 39, 534–543 (2002). PubMed Google Scholar * Stalker, T. J. et al. A systems approach to hemostasis: 3. Thrombus consolidation
regulates intrathrombus transport and local thrombin activity. _Blood_ 124, 1824–1831 (2014). CAS PubMed PubMed Central Google Scholar * Brass, L. F. & Stalker, T. J. Minding the
gaps—and the junctions, too. _Circulation_ 125, 2414–2416 (2012). PubMed PubMed Central Google Scholar * Vaiyapuri, S. et al. Gap junctions and connexin hemichannels underpin hemostasis
and thrombosis. _Circulation_ 125, 2479–2491 (2012). CAS PubMed PubMed Central Google Scholar * Swieringa, F., Kuijpers, M. J., Lamers, M. M., van der Meijden, P. E. J. & Heemskerk,
J. W. M. Rate-limiting roles of the tenase complex of factors VIII and IX in platelet procoagulant activity and formation of platelet-fibrin thrombi under flow. _Haematologica_ 100, 748–756
(2015). CAS PubMed PubMed Central Google Scholar * Mammadova-Bach, E. et al. Platelet glycoprotein VI binds to polymerized fibrin and promotes thrombin generation. _Blood_ 126, 683–691
(2015). CAS PubMed Google Scholar * Van der Meijden, P. E. J. et al. Dual role of collagen in factor XII-dependent thrombus and clot formation. _Blood_ 114, 881–890 (2009). PubMed Google
Scholar * Verhoef, J. J. et al. Polyphosphate nanoparticles on the platelet surface trigger contact system activation. _Blood_ 129, 1707–1717 (2017). CAS PubMed PubMed Central Google
Scholar * Payne, H., Ponomaryov, T., Watson, S. P. & Brill, A. Mice with a deficiency in CLEC-2 are protected against deep vein thrombosis. _Blood_ 129, 2013–2020 (2017). CAS PubMed
PubMed Central Google Scholar * Stefanini, L. et al. RASA3 s a critical inhibitor of RAP1-dependent platelet activation. _J. Clin. Invest._ 125, 1419–1432 (2015). PubMed PubMed Central
Google Scholar * Golebiewska, E. M. et al. Syntaxin 8 regulates platelet dense granule secretion, aggregation, and thrombus stability. _J. Biol. Chem._ 290, 1536–1545 (2015). PubMed Google
Scholar * Mattheij, N. J. A. et al. Survival protein anoctamin-6 controls multiple platelet responses including phospholipid scrambling, swelling and protein cleavage. _FASEB. J._ 30,
727–737 (2016). CAS PubMed Google Scholar * Schaff, M. et al. Integrin α6β1 is the main receptor for vascular laminins and plays a role in platelet adhesion, activation, and arterial
thrombosis. _Circulation_ 128, 541–552 (2013). CAS PubMed Google Scholar * Bunimov, N., Fuller, N. & Hayward, C. P. Genetic loci associated with platelet traits and platelet
disorders. _Semin. Thromb. Hemost._ 39, 291–305 (2013). CAS PubMed Google Scholar * Nurden, A. T. & Nurden, P. Inherited disorders of platelet function: selected updates. _J. Thromb.
Haemost._ 13, S2–S9 (2015). CAS PubMed Google Scholar * Bianchi, E., Norfo, R., Pennucci, V., Zini, R. & Manfredini, R. Genomic landscape of megakaryopoiesis and platelet function
defects. _Blood_ 127, 1249–1259 (2016). CAS PubMed PubMed Central Google Scholar * Tijssen, M. R. et al. Genome-wide analysis of simultaneous GATA1/2, RUNX1, FLI1, and SCL binding in
megakaryocytes identifies hematopoietic regulators. _Dev. Cell_ 20, 597–609 (2011). CAS PubMed PubMed Central Google Scholar * Freson, K. & Turro, E. High-throughput sequencing
approaches for diagnosing hereditary bleeding and platelet disorders. _J. Thromb. Haemost._ 15, 1262–1272 (2017). CAS PubMed Google Scholar * Simeoni, L. et al. A comprehensive
high-throughput sequencing test for the diagnosis of inherited bleeding, thrombotic and platelet disorders. _Blood_ 127, 2791–2803 (2016). CAS PubMed PubMed Central Google Scholar *
Bastida, J. M. et al. Introducing high-throughput sequencing into mainstream genetic diagnosis practice in inherited platelet disorders. _Haematologica_ 103, 148–162 (2018). CAS PubMed
PubMed Central Google Scholar * Lentaigne, C. et al. Inherited platelet disorders: toward DNA-based diagnosis. _Blood_ 127, 2814–2823 (2016). CAS PubMed PubMed Central Google Scholar *
Astle, W. J. et al. The allelic landscape of human blood cell trait variation and links to common complex disease. _Cell_ 167, 1415–1429 (2016). CAS PubMed PubMed Central Google Scholar
* Gieger, C. et al. New gene functions in megakaryopoiesis and platelet formation. _Nature_ 480, 201–207 (2011). CAS PubMed PubMed Central Google Scholar * Petersen, R. et al. Platelet
function is modified by common sequence variation in megakaryocyte super enhancer. _Nat. Commun._ 8, 16058 (2017). CAS PubMed PubMed Central Google Scholar * Nagy, M. et al. Variable
impairment of platelet functions in patients with severe, genetically linked immune deficiencies. _Haematologica_ 103, 540–549 (2018). CAS PubMed PubMed Central Google Scholar * Snoep,
J. D. et al. The minor alleleof GP6 T13254C is associated with decreased platelet activation and a reduced risk of recurrent cardiovascular events and mortality: results from the
SMILE-Platelets project. _J. Thromb. Haemost._ 8, 2377–2384 (2010). CAS PubMed Google Scholar * Williams, M. S. et al. Genetic regulation of platelet receptor expression and function:
application in clinical practice and drug development._ Arterioscler. Thromb. Vasc. Biol._ 30, 2372–2384 (2010). CAS Google Scholar * Joshi, S. & Whiteheart, S. W. The nuts and bolts
of the platelet release reaction. _Platelets_ 28, 129–137 (2017). CAS PubMed Google Scholar * Golebiewska, E. M. & Poole, A. W. Platelet secretion: from haemostasis to wound healing
and beyond. _Blood Rev._ 29, 153–162 (2015). CAS PubMed PubMed Central Google Scholar * Adam, F. et al. Kinesin-1 is a new actor involved in platelet secretion and thrombus stability.
_Arterioscler. Thromb. Vasc. Biol._ 38, 1037–1051 (2018). CAS PubMed Google Scholar * Meng, R. et al. Defective release of α granule and lysosome contents from platelets in mouse
Hermansky-Pudlak syndrome models. _Blood_ 125, 1623–1632 (2015). CAS PubMed PubMed Central Google Scholar * Sharda, A. et al. Defective PDI release from platelets and endothelial cells
impairs thrombus formation in Hermansky-Pudlak syndrome. _Blood_ 125, 1633–1642 (2015). CAS PubMed PubMed Central Google Scholar * Battinelli, E. M., Markens, B. A. & Italiano, J. E.
Jr. Release of angiogenesis regulatory proteins from platelet α granules: modulation of physiologic and pathologic angiogenesis. _Blood_ 118, 1359–1369 (2011). CAS PubMed PubMed Central
Google Scholar * Sobota, J. A., Ferraro, F., Back, N., Eipper, B. A. & Mains, R. E. Not all secretory granules are created equal: partitioning of soluble content proteins. _Mol. Biol.
Cell_ 17, 5038–5052 (2006). CAS PubMed PubMed Central Google Scholar * Eckly, A. et al. Respective contributions of single and compound granule fusion to secretion by activated
platelets. _Blood_ 128, 2538–2549 (2016). CAS PubMed PubMed Central Google Scholar * King, S. M. et al. Platelet dense-granule secretion plays a critical role in thrombosis and
subsequent vascular remodeling in atherosclerotic mice. _Circulation_ 120, 785–791 (2009). CAS PubMed PubMed Central Google Scholar * Deppermann, C. et al. Gray platelet syndrome and
defective thrombo-inflammation in Nbeal2-deficient mice. _J. Clin. Invest._ 123, 3331–3342 (2013). CAS PubMed Central Google Scholar * O’Donnell, V. B., Murphy, R. C. & Watson, S. P.
Platelet lipidomics: modern day perspective on lipid discovery and characterization in platelets. _Circ. Res._ 114, 1185–1203 (2014). PubMed PubMed Central Google Scholar * Edelstein, L.
C. The role of platelet microvesicles in intercellular communication. _Platelets_ 28, 222–227 (2017). CAS PubMed Google Scholar * Melki, I., Tessandier, N., Zufferey, A. & Boilard, E.
Platelet microvesicles in health and disease. _Platelets_ 28, 214–221 (2017). CAS PubMed Google Scholar * Dinkla, S. et al. Platelet microparticles inhibit IL-17 production by regulatory
T cells through P-selectin. _Blood_ 127, 1976–1986 (2016). CAS PubMed Google Scholar * Duchez, A. C. et al. Platelet microparticles are internalized in neutrophils via the concerted
activity of 12-lipoxygenase and secreted phospholipase A2-IIA. _Proc. Natl Acad. Sci. USA_ 112, E3564–E3573 (2015). CAS PubMed PubMed Central Google Scholar * Vasina, E. M. et al. Aging-
and activation-induced platelet microparticles suppress apoptosis in monocytic cells and differentially signal to proinflammatory mediator release. _Am. J. Blood Res._ 3, 107–123 (2013).
CAS PubMed PubMed Central Google Scholar * Boilard, E. et al. Platelets amplify inflammation in arthritis via collagen-dependent microparticle production. _Science_ 327, 580–583 (2010).
CAS PubMed PubMed Central Google Scholar * Best, M. G. et al. RNA-seq of tumor-educated platelets enables blood-based pan-cancer, multiclass, and molecular pathway cancer diagnostics.
_Cancer Cell_ 28, 666–676 (2015). CAS PubMed PubMed Central Google Scholar * Gidlof, O. et al. Platelets activated during myocardial infarction release functional miRNA, which can be
taken up by endothelial cells and regulate ICAM1 expression. _Blood_ 121, 3908–3917 (2013). PubMed Google Scholar * Michael, J. V. et al. Platelet microparticles infiltrating solid tumors
transfer mi-RNAs that suppress tumor growth. _Blood_ 130, 567–580 (2017). CAS PubMed PubMed Central Google Scholar * Keularts, I. M., van Gorp, R. M., Feijge, M. A., Vuist, W. M. &
Heemskerk, J. W. α2A-adrenergic receptor stimulation potentiates calcium release in platelets by modulating cAMP levels. _J. Biol. Chem._ 275, 1763–1772 (2000). CAS PubMed Google Scholar
* Blair, T. A. et al. Phosphoinositide 3-kinases p110α and p110β have differential roles in insulin-like growth factor-1-mediated Akt phosphorylation and platelet priming. _Arterioscler.
Thromb. Vasc. Biol._ 34, 1681–1688 (2014). CAS PubMed Google Scholar * Cosemans, J. M. E. M. et al. Potentiating roles for Gas6 and Tyro, Axl and Mer (TAM) receptors in human and murine
platelet activation and thrombus stabilization. _J. Thromb. Haemost._ 8, 1797–1808 (2010). CAS PubMed Google Scholar * Kuijpers, M. J. et al. Platelet CD40L modulates thrombus growth via
phosphatidylinositol 3-kinase β, and not via CD40 and IκB kinase α. _Arterioscler. Thromb. Vasc. Biol._ 35, 1374–1381 (2015). CAS PubMed Google Scholar * Westein, E. et al.
Atherosclerotic geometries spatially confine and exacerbate pathological thrombus formation poststenosis in a von Willebrand factor-dependent manner. _Proc. Natl Acad. Sci. USA_ 110,
1357–1362 (2013). CAS PubMed PubMed Central Google Scholar * Blair, T. A., Moore, S. F. & Hers, I. Circulating primers enhance platelet function and induce resistance to antiplatelet
therapy. _J. Thromb. Haemost._ 13, 1479–1493 (2015). CAS PubMed PubMed Central Google Scholar * Swieringa, F., Kuijpers, M. J. E., Heemskerk, J. W. M. & van der Meijden, P. E. J.
Targeting platelet receptor function in thrombus formation: the risk of bleeding. _Blood Rev._ 28, 9–21 (2014). CAS PubMed Google Scholar * Naseem, K. M. & Roberts, W. Nitric oxide at
a glance. _Platelets_ 22, 148–152 (2011). CAS PubMed Google Scholar * Tourdot, B. E. et al. 12-HETrE inhibits platelet reactivity and thrombosis in part through the prostacyclin
receptor. _Blood Adv._ 1, 1124–1131 (2017). CAS PubMed PubMed Central Google Scholar * Kraakman, M. J. et al. Neutrophil-derived S100 calcium-binding proteins A8/A9 promote reticulated
thrombocytosis and atherogenesis in diabetes. _J. Clin. Invest._ 127, 2133–2147 (2017). PubMed PubMed Central Google Scholar * Von Hundelshausen, P. et al. Chemokine interactome mapping
enables tailored intervention in acute and chronic inflammation. _Sci. Transl Med._ 9, 384 (2017). Google Scholar * Ferroni, P. et al. Biomarkers of platelet activation in acute coronary
syndromes. _Thromb. Haemost._ 108, 1109–1123 (2012). PubMed Google Scholar * Ho-Tin-Noe, B., Demers, M. & Wagner, D. D. How platelets safeguard vascular integrity. _J. Thromb.
Haemost._ 9 (Suppl. 1), 56–65 (2011). PubMed PubMed Central Google Scholar * Chatterjee, M. & Gawaz, M. Platelet-derived CXCL12 (SDF-1α): basic mechanisms and clinical implications.
_J. Thromb. Haemost._ 11, 1954–1967 (2013). CAS PubMed Google Scholar * Ho-Tin-Noe, B., Boulaftali, Y. & Camerer, E. Platelets and vascular integrity: how platelets prevent bleeding
in inflammation. _Blood_ 131, 277–288 (2018). CAS PubMed Google Scholar * Croce, K. & Libby, P. Intertwining of thrombosis and inflammation in atherosclerosis. _Curr. Opin. Hematol._
14, 55–61 (2007). CAS PubMed Google Scholar * Nieswandt, B., Kleinschnitz, C. & Stoll, G. Ischaemic stroke: a thrombo-inflammatory disease? _J. Physiol._ 589, 4115–4123 (2011). CAS
PubMed PubMed Central Google Scholar * Maiocchi, S., Alwis, I., Wu, M. C. L., Yuan, Y. & Jackson, S. P. Thromboinflammatory functions of platelets in ischemia-reperfusion injury and
its dysregulation in diabetes. _Semin. Thromb. Hemost._ 44, 102–113 (2018). CAS PubMed Google Scholar * Kleinschnitz, C. et al. Targeting platelets in acute experimental stroke: impact of
glycoprotein Ib, VI, and IIb/IIIa blockade on infarct size, functional outcome, and intracranial bleeding. _Circulation_ 115, 2323–2330 (2007). CAS PubMed Google Scholar * Bierings, R.
& Voorberg, J. Up or out: polarity of VWF release. _Blood_ 128, 154–155 (2016). CAS PubMed Google Scholar * Sreeramkumar, V. et al. Neutrophils scan for activated platelets to
initiate inflammation. _Science_ 346, 1234–1238 (2014). CAS PubMed PubMed Central Google Scholar * Gerdes, N. et al. Platelet CD40 exacerbates atherosclerosis by transcellular activation
of endothelial cells and leukocytes. _Arterioscler. Thromb. Vasc. Biol._ 36, 482–490 (2016). CAS PubMed Google Scholar * Wang, Y. et al. Leukocyte integrin Mac-1 regulates thrombosis via
interaction with platelet GPIbα. _Nat. Commun._ 8, 15559 (2017). CAS PubMed PubMed Central Google Scholar * Koenen, R. R. et al. Disrupting functional interactions between platelet
chemokines inhibits atherosclerosis in hyperlipidemic mice. _Nat. Med._ 15, 97–103 (2009). CAS PubMed Google Scholar * Vajen, T., Mause, S. F. & Koenen, R. R. Microvesicles from
platelets: novel drivers of vascular inflammation. _Thromb. Haemost._ 114, 228–236 (2015). CAS PubMed PubMed Central Google Scholar * Ekdahl, K. N. et al. Thromboinflammation in
therapeutic medicine. _Adv. Exp. Med. Biol._ 865, 3–17 (2015). CAS PubMed Google Scholar * Martinod, K. et al. Neutrophil histone modification by peptidylarginine deiminase 4 is critical
for deep vein thrombosis in mice. _Proc. Natl Acad. Sci. USA_ 110, 8674–8679 (2013). CAS PubMed PubMed Central Google Scholar * Muller, K. A., Chatterjee, M., Rath, D. & Geisler, T.
Platelets, inflammation and anti-inflammatory effects of antiplatelet drugs in ACS and CAD. _Thromb. Haemost._ 114, 498–518 (2015). PubMed Google Scholar * Chatterjee, M. & Geisler, T.
Inflammatory contribution of platelets revisited: new players in the arena of inflammation. _Semin. Thromb. Hemost._ 42, 205–214 (2016). CAS PubMed Google Scholar * Koupenova, M.,
Clancy, L., Corkrey, H. A. & Freedman, J. E. Circulating platelets as mediators of immunity, inflammation, and thrombosis. _Circ. Res._ 122, 337–351 (2018). CAS PubMed PubMed Central
Google Scholar * Virmani, R., Burke, A. P., Farb, A. & Kolodgie, F. D. Pathology of the vulnerable plaque. _J. Am. Coll. Cardiol._ 47, C13–C18 (2006). CAS PubMed Google Scholar *
Hechler, B. & Gachet, C. Comparison of two murine models of thrombosis induced by atherosclerotic plaque injury. _Thromb. Haemost._ 105 (Suppl. 1), S3–12 (2011). CAS PubMed Google
Scholar * Kuijpers, M. J. E. et al. Complementary roles of platelets and coagulation in thrombus formation on plaques acutely ruptured by targeted ultrasound treatment: a novel intravital
model. _J. Thromb. Haemost._ 7, 152–161 (2009). CAS PubMed Google Scholar * Farb, A. et al. Coronary plaque erosion without rupture into a lipid core. A frequent cause of coronary
thrombosis in sudden coronary death. _Circulation_ 93, 1354–1363 (1996). CAS PubMed Google Scholar * Sato, Y. et al. Proportion of fibrin and platelets differs in thrombi on ruptured and
eroded coronary atherosclerotic plaques in humans. _Heart_ 91, 526–530 (2005). CAS PubMed PubMed Central Google Scholar * Xing, L. et al. EROSION study (Effective Anti-Thrombotic Therapy
Without Stenting: Intravascular Optical Coherence Tomography-Based Management in Plaque Erosion): a 1-year follow-up report. _Circ. Cardiovasc. Interv_. 10 (2017). * Mackman, N. Triggers,
targets and treatments for thrombosis. _Nature_ 451, 914–918 (2008). CAS PubMed PubMed Central Google Scholar * Olie, R. H., van der Meijden, P. E. J. & Ten Cate, H. The coagulation
system in atherothrombosis: implications for new therapeutic strategies. _Res. Pract. Thromb. Haemost._ 2, 188–198 (2018). CAS PubMed PubMed Central Google Scholar * Patrono, C. et al.
Antiplatelet agents for the treatment and prevention of coronary atherothrombosis. _J. Am. Coll. Cardiol._ 70, 1760–1776 (2017). PubMed Google Scholar * Halvorsen, S. et al. Aspirin
therapy in primary cardiovascular disease prevention: a position paper of the European Society of Cardiology working group on thrombosis. _J. Am. Coll. Cardiol._ 64, 319–327 (2014). CAS
PubMed Google Scholar * McFadyen, J. D., Schaff, M. & Peter, K. Current and future antiplatelet therapies: emphasis on preserving haemostasis. _Nat. Rev. Cardiol._ 15, 181–191 (2018).
CAS PubMed Google Scholar * Cattaneo, M. P2Y12 receptors: structure and function. _J. Thromb. Haemost._ 13 (Suppl. 1), S10–S16 (2015). CAS PubMed Google Scholar * Claessen, B. E. et
al. Stent thrombosis: a clinical perspective. _JACC Cardiovasc. Interv._ 7, 1081–1092 (2014). PubMed Google Scholar * Torrado, J. et al. Restenosis, stent thrombosis, and bleeding
complications: navigating between Scylla and Charybdis. _J. Am. Coll. Cardiol._ 71, 1676–1695 (2018). PubMed Google Scholar * Levine, G. N. et al. 2016 ACC/AHA Guideline Focused Update on
duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice
Guidelines. _J. Am. Coll. Cardiol._ 68, 1082–1115 (2016). PubMed Google Scholar * Jones, B. M. et al. Matching patients with the ever-expanding range of TAVI devices. _Nat. Rev. Cardiol._
14, 615–626 (2017). PubMed Google Scholar * Nishimura, R. A. et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: a
report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. _J. Am. Coll. Cardiol._ 70, 252–289 (2017). PubMed Google Scholar *
Raheja, H. et al. Comparison of single versus dual antiplatelet therapy after TAVR: a systematic review and meta-analysis. _Catheter Cardiovasc. Interv._ 00, 1–9 (2018). Google Scholar *
Baumann Kreuziger, L. M., Kim, B. & Wieselthaler, G. M. Antithrombotic therapy for left ventricular assist devices in adults: a systematic review. _J. Thromb. Haemost._ 13, 946–955
(2015). CAS PubMed Google Scholar * Bergmeijer, T. O. et al. Genome-wide and candidate gene approaches of clopidogrel efficacy using pharmacodynamic and clinical end points-Rationale and
design of the International Clopidogrel Pharmacogenomics Consortium (ICPC). _Am. Heart. J._ 198, 152–159 (2018). CAS PubMed Google Scholar * Gilio, K. et al. Non-redundant roles of
phosphoinositide 3-kinase isoforms α and β in glycoprotein VI-induced platelet signaling and thrombus formation. _J. Biol. Chem._ 284, 33750–33762 (2009). CAS PubMed PubMed Central Google
Scholar * Nylander, S., Wagberg, F., Andersson, M., Skarby, T. & Gustafsson, D. Exploration of efficacy and bleeding with combined phosphoinositide 3-kinase β inhibition and aspirin in
man. _J. Thromb. Haemost._ 13, 1494–1502 (2015). CAS PubMed Google Scholar * Tullemans, B. M. E., Heemskerk, J. W. M. & Kuijpers, M. J. E. Acquired platelet antagonism: off-target
antiplatelet effects of malignancy treatment with tyrosine kinase inhibitors. _J. Thromb. Haemost._ 16, 1–14 (2018). Google Scholar * Busygina, K. et al. Oral Bruton tyrosine kinase
inhibitors selectively block atherosclerotic plaque-triggered thrombus formation in humans. _Blood_ 131, 2605–2616 (2018). CAS PubMed Google Scholar * Moeckel, D. et al. Optimizing human
apyrase to treat arterial thrombosis and limit reperfusion injury without increasing bleeding risk. _Sci. Transl. Med._ 6, 248ra105 (2014). PubMed PubMed Central Google Scholar * Tardif,
J. C. et al. Effects of the P-selectin antagonist inclacumab on myocardial damage after percutaneous coronary intervention for non-ST-segment elevation myocardial infarction: results of the
SELECT-ACS trial. _J. Am. Coll. Cardiol._ 61, 2048–2055 (2013). CAS PubMed Google Scholar * Pasalic, L. et al. Novel assay demonstrates that coronary artery disease patients have
heightened procoagulant platelet response. _J. Thromb. Haemost._ 16, 1198–1210 (2018). CAS PubMed PubMed Central Google Scholar * Eikelboom, J. W. et al. Rivaroxaban with or without
aspirin in stable cardiovascular disease. _N. Engl. J. Med._ 377, 1319–1330 (2017). CAS PubMed Google Scholar * Bye, A. P., Unsworth, A. J. & Gibbins, J. M. Platelet signaling: a
complex interplay between inhibitory and activatory networks. _J. Thromb. Haemost._ 14, 918–930 (2016). CAS PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS The
authors thank the Cardiovascular Centre (HVC) of Maastricht University Medical Centre, The Netherlands, for support. We thank C. Baaten and J. van Geffen (Maastricht University, The
Netherlands) for their help in preparing the figures before submission. REVIEWER INFORMATION _Nature Reviews Cardiology_ thanks E. Gardiner, M. Gawaz, and the other, anonymous reviewer for
their contribution to the peer review of this work. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Biochemistry, Cardiovascular Research Institute Maastricht (CARIM), Maastricht
University, Maastricht, The Netherlands Paola E. J. van der Meijden & Johan W. M. Heemskerk Authors * Paola E. J. van der Meijden View author publications You can also search for this
author inPubMed Google Scholar * Johan W. M. Heemskerk View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Both authors researched data for the
article, discussed its content, wrote the manuscript, and reviewed and edited it before submission. CORRESPONDING AUTHORS Correspondence to Paola E. J. van der Meijden or Johan W. M.
Heemskerk. ETHICS DECLARATIONS COMPETING INTERESTS P.E.J.v.d.M. is a consultant at Bayer AG. J.W.M.H. is a founder and shareholder of FlowChamber BV. ADDITIONAL INFORMATION PUBLISHER’S NOTE
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. GLOSSARY * Fibrin coat Fibrin-coated platelets are a subpopulation of
phosphatidylserine-exposing platelets that bind fibrin via transglutaminase activity and activated integrin αIIbβ3. Fibrin is ‘coated’ on the platelet surface. * Membrane ballooning Adherent
platelets on a collagen surface form phosphatidylserine-exposing, balloon-like membrane structures as a result of salt and water entry into the platelets. * Procoagulant platelet Platelet
swollen to a balloon shape, with surface exposure of phosphatidylserine and displaying greatly increased capacity for coagulation factor activation. * Pseudopod formation Cytoplasm-filled
projection of the platelet membrane following platelet activation. * α-Granules Platelet secretion granules containing multiple stored proteins including growth factors. * δ-Granules
Platelet secretion granules with dense appearance in electron microscopy, containing Ca2+-bound nucleotides (ADP, ATP, and polyphosphates). * Plateletcrit Product of mean platelet volume and
platelet count in blood. * Negative or positive platelet priming Suppression or promotion of platelet activation by bioactive molecules in the blood. * Exhausted platelets Also known as
refractive platelets; platelets with reduced secretion capacity owing to previous activation. * Weibel–Palade bodies Storage granules of endothelial cells that store ultralarge von
Willebrand factor multimers. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE van der Meijden, P.E.J., Heemskerk, J.W.M. Platelet biology and functions:
new concepts and clinical perspectives. _Nat Rev Cardiol_ 16, 166–179 (2019). https://doi.org/10.1038/s41569-018-0110-0 Download citation * Published: 14 November 2018 * Issue Date: March
2019 * DOI: https://doi.org/10.1038/s41569-018-0110-0 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable
link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
