Chains of evidence from correlations to causal molecules in microbiome-linked diseases
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

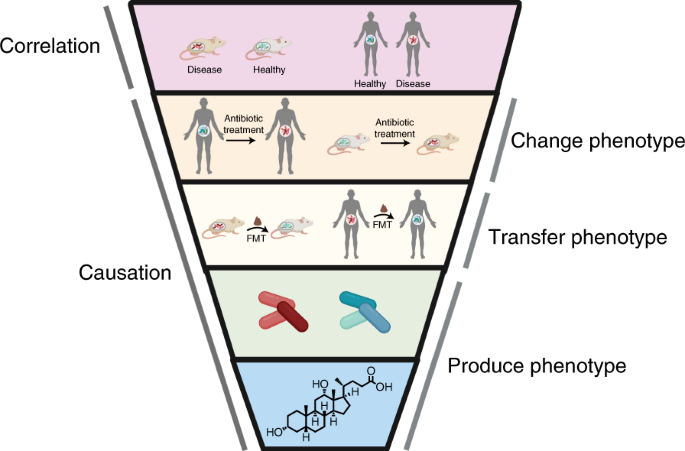
ABSTRACT Human-associated microorganisms play a vital role in human health, and microbial imbalance has been linked to a wide range of disease states. In this Review, we explore recent
efforts to progress from correlative studies that identify microorganisms associated with human disease to experiments that establish causal relationships between microbial products and host
phenotypes. We propose that successful efforts to uncover phenotypes often follow a chain of evidence that proceeds from (1) association studies; to (2) observations in germ-free animals
and antibiotic-treated animals and humans; to (3) fecal microbiota transplants (FMTs); to (4) identification of strains; and then (5) molecules that elicit a phenotype. Using this
experimental ‘funnel’ as our guide, we explore how the microbiota contributes to metabolic disorders and hypertension, infections, and neurological conditions. We discuss the potential to
use FMTs and microbiota-inspired therapies to treat human disease as well as the limitations of these approaches. Access through your institution Buy or subscribe This is a preview of
subscription content, access via your institution ACCESS OPTIONS Access through your institution Access Nature and 54 other Nature Portfolio journals Get Nature+, our best-value
online-access subscription $29.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12 print issues and online access $259.00 per year only $21.58 per issue Learn more
Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS:
* Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS GUT MICROBIOTA IN HUMAN METABOLIC HEALTH AND DISEASE
Article 04 September 2020 A CONSENSUS STATEMENT ON ESTABLISHING CAUSALITY, THERAPEUTIC APPLICATIONS AND THE USE OF PRECLINICAL MODELS IN MICROBIOME RESEARCH Article 03 March 2025 CAUSAL
EFFECTS IN MICROBIOMES USING INTERVENTIONAL CALCULUS Article Open access 11 March 2021 REFERENCES * Nicolas, G. R. & Chang, P. V. Deciphering the chemical lexicon of host–gut microbiota
interactions. _Trends Pharmacol. Sci._ 40, 430–445 (2019). Article CAS PubMed PubMed Central Google Scholar * Luczynski, P. et al. Growing up in a bubble: using germ-free animals to
assess the influence of the gut microbiota on brain and behavior. _Int. J. Neuropsychopharmacol._ 19, pyw020 (2016). Article PubMed PubMed Central CAS Google Scholar * Kennedy, E. A.,
King, K. Y. & Baldridge, M. T. Mouse microbiota models: comparing germ-free mice and antibiotics treatment as tools for modifying gut bacteria. _Front. Physiol._ 9, 1534 (2018). Article
PubMed PubMed Central Google Scholar * Bramante, C. T., Lee, C. J. & Gudzune, K. A. Treatment of obesity in patients with diabetes. _Diabetes Spectr._ 30, 237–243 (2017). Article
PubMed PubMed Central Google Scholar * Schnurr, T. M. et al. Obesity, unfavourable lifestyle and genetic risk of type 2 diabetes: a case-cohort study. _Diabetologia_ 63, 1324–1332 (2020).
Article CAS PubMed Google Scholar * Jiang, S. Z., Lu, W., Zong, X. F., Ruan, H. Y. & Liu, Y. Obesity and hypertension. _Exp. Ther. Med._ 12, 2395–2399 (2016). Article PubMed
PubMed Central Google Scholar * Grigorescu, I. & Dumitrascu, D. L. Implication of gut microbiota in diabetes mellitus and obesity. _Acta Endocrinol._ 12, 206–214 (2016). CAS Google
Scholar * Castaner, O. et al. The gut microbiome profile in obesity: a systematic review. _Int. J. Endocrinol._ 2018, 4095789 (2018). PubMed PubMed Central Google Scholar * Dao, M. C. et
al. _Akkermansia muciniphila_ abundance is lower in severe obesity, but its increased level after bariatric surgery is not associated with metabolic health improvement. _Am. J. Physiol.
Endocrinol. Metab._ 317, E446–E459 (2019). Article CAS PubMed Google Scholar * Dao, M. C. et al. _Akkermansia muciniphila_ and improved metabolic health during a dietary intervention in
obesity: relationship with gut microbiome richness and ecology. _Gut_ 65, 426–436 (2016). Article CAS PubMed Google Scholar * Yan, Q. et al. Alterations of the gut microbiome in
hypertension. _Front. Cell Infect. Microbiol._ 7, 381 (2017). Article PubMed PubMed Central CAS Google Scholar * Li, J. et al. Gut microbiota dysbiosis contributes to the development of
hypertension. _Microbiome_ 5, 14 (2017). Article PubMed PubMed Central Google Scholar * Liu, J. et al. Correlation analysis of intestinal flora with hypertension. _Exp. Ther. Med._ 16,
2325–2330 (2018). PubMed PubMed Central Google Scholar * Scott, F. I. et al. Administration of antibiotics to children before age 2 years increases risk for childhood obesity.
_Gastroenterology_ 151, 120–129 (2016). Article CAS PubMed Google Scholar * Hwang, I. et al. Alteration of gut microbiota by vancomycin and bacitracin improves insulin resistance via
glucagon-like peptide 1 in diet-induced obesity. _FASEB J._ 29, 2397–2411 (2015). Article CAS PubMed Google Scholar * Miao, Z. et al. Antibiotics can cause weight loss by impairing gut
microbiota in mice and the potent benefits of lactobacilli. _Biosci. Biotechnol. Biochem._ 84, 411–420 (2020). Article CAS PubMed Google Scholar * Hooper, L. V. Bacterial contributions
to mammalian gut development. _Trends Microbiol._ 12, 129–134 (2004). Article CAS PubMed Google Scholar * Davis, C. D. The gut microbiome and its role in obesity. _Nutr. Today_ 51,
167–174 (2016). Article PubMed PubMed Central Google Scholar * Honour, J. W., Borriello, S. P., Ganten, U. & Honour, P. Antibiotics attenuate experimental hypertension in rats. _J.
Endocrinol._ 105, 347–350 (1985). Article CAS PubMed Google Scholar * Sanada, T. J. et al. Gut microbiota modification suppresses the development of pulmonary arterial hypertension in an
SU5416/hypoxia rat model. _Pulm. Circ._ 10, 2045894020929147 (2020). Article PubMed PubMed Central CAS Google Scholar * Galla, S. et al. Disparate effects of antibiotics on
hypertension. _Physiol. Genomics_ 50, 837–845 (2018). Article CAS PubMed PubMed Central Google Scholar * Ridaura, V. K. et al. Gut microbiota from twins discordant for obesity modulate
metabolism in mice. _Science_ 341, 1241214 (2013). Article PubMed CAS Google Scholar * Wang, S. et al. Gut microbiota mediates the anti-obesity effect of calorie restriction in mice.
_Sci. Rep._ 8, 13037 (2018). Article PubMed PubMed Central CAS Google Scholar * Lai, Z. L. et al. Fecal microbiota transplantation confers beneficial metabolic effects of diet and
exercise on diet-induced obese mice. _Sci. Rep._ 8, 15625 (2018). Article PubMed PubMed Central CAS Google Scholar * de Groot, P. et al. Donor metabolic characteristics drive effects of
faecal microbiota transplantation on recipient insulin sensitivity, energy expenditure and intestinal transit time. _Gut_ 69, 502–512 (2020). Article PubMed CAS Google Scholar * Wu, H.
et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. _Nat. Med._ 23, 850–858 (2017). Article
CAS PubMed Google Scholar * Wang, H. et al. Promising treatment for type 2 diabetes: fecal microbiota transplantation reverses insulin resistance and impaired islets. _Front. Cell Infect.
Microbiol._ 9, 455 (2019). Article CAS PubMed Google Scholar * Kootte, R. S. et al. Improvement of insulin sensitivity after lean donor feces in metabolic syndrome is driven by baseline
intestinal microbiota composition. _Cell Metab._ 26, 611–619 (2017). Article CAS PubMed Google Scholar * Vrieze, A. et al. Transfer of intestinal microbiota from lean donors increases
insulin sensitivity in individuals with metabolic syndrome. _Gastroenterology_ 143, 913–6 (2012). Article CAS PubMed Google Scholar * Zhang, Z. et al. Impact of fecal microbiota
transplantation on obesity and metabolic syndrome—a systematic review. _Nutrients_ 11, 2291 (2019). Article CAS PubMed Central Google Scholar * Durgan, D. J. et al. Role of the gut
microbiome in obstructive sleep apnea-induced hypertension. _Hypertension_ 67, 469–474 (2016). Article CAS PubMed Google Scholar * Adnan, S. et al. Alterations in the gut microbiota can
elicit hypertension in rats. _Physiol. Genomics_ 49, 96–104 (2017). Article CAS PubMed Google Scholar * Ridlon, J. M., Kang, D.-J. & Hylemon, P. B. Bile salt biotransformations by
human intestinal bacteria. _J. Lipid Res._ 47, 241–259 (2006). Article CAS PubMed Google Scholar * Broeders, E. P. et al. The bile acid chenodeoxycholic acid increases human brown
adipose tissue activity. _Cell Metab._ 22, 418–426 (2015). Article CAS PubMed Google Scholar * Kars, M. et al. Tauroursodeoxycholic acid may improve liver and muscle but not adipose
tissue insulin sensitivity in obese men and women. _Diabetes_ 59, 1899–1905 (2010). Article CAS PubMed PubMed Central Google Scholar * Zhang, H. M. et al. Beneficial effect of farnesoid
X receptor activation on metabolism in a diabetic rat model. _Mol. Med. Rep._ 13, 2135–2142 (2016). Article CAS PubMed Google Scholar * Sun, L. et al. Gut microbiota and intestinal FXR
mediate the clinical benefits of metformin. _Nat. Med._ 24, 1919–1929 (2018). Article CAS PubMed PubMed Central Google Scholar * Schittenhelm, B. et al. Role of FXR in beta-cells of
lean and obese mice. _Endocrinology_ 156, 1263–1271 (2015). Article CAS PubMed Google Scholar * Koh, A., De Vadder, F., Kovatcheva-Datchary, P. & Backhed, F. From dietary fiber to
host physiology: short-chain fatty acids as key bacterial metabolites. _Cell_ 165, 1332–1345 (2016). Article CAS PubMed Google Scholar * Liu, Y. et al. Gut microbiome fermentation
determines the efficacy of exercise for diabetes prevention. _Cell Metab._ 31, 77–91 (2020). Article CAS PubMed Google Scholar * La Rosa, S. L. et al. The human gut Firmicute _Roseburia
intestinalis_ is a primary degrader of dietary β-mannans. _Nat. Commun._ 10, 905 (2019). Article PubMed PubMed Central CAS Google Scholar * Chambers, E. S. et al. Effects of targeted
delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. _Gut_ 64, 1744–1754 (2015). Article CAS PubMed Google Scholar
* van der Hee, B. & Wells, J. M. Microbial regulation of host physiology by short-chain fatty acids. _Trends Microbiol_. https://doi.org/10.1016/j.tim.2021.02.001 (2021). * Kim, K. N.,
Yao, Y. & Ju, S. Y. Short chain fatty acids and fecal microbiota abundance in humans with obesity: a systematic review and meta-analysis. _Nutrients_ 11, 2512 (2019). Article CAS
PubMed Central Google Scholar * Muller, M. et al. Circulating but not faecal short-chain fatty acids are related to insulin sensitivity, lipolysis and GLP-1 concentrations in humans. _Sci.
Rep._ 9, 12515 (2019). Article PubMed PubMed Central CAS Google Scholar * Canfora, E. E., Jocken, J. W. & Blaak, E. E. Short-chain fatty acids in control of body weight and insulin
sensitivity. _Nat. Rev. Endocrinol._ 11, 577–591 (2015). Article CAS PubMed Google Scholar * den Besten, G. et al. The role of short-chain fatty acids in the interplay between diet, gut
microbiota, and host energy metabolism. _J. Lipid Res._ 54, 2325–2340 (2013). Article CAS Google Scholar * Pluznick, J. L. Microbial short-chain fatty acids and blood pressure
regulation. _Curr. Hypertension Rep._ 19, 25 (2017). Article CAS Google Scholar * Oyama, J.-I. & Node, K. Gut microbiota and hypertension. _Hypertension Res._ 42, 741–743 (2019).
Article Google Scholar * Latif, S. A., Pardo, H. A., Hardy, M. P. & Morris, D. J. Endogenous selective inhibitors of 11β-hydroxysteroid dehydrogenase isoforms 1 and 2 of adrenal
origin. _Mol. Cell. Endocrinol._ 243, 43–50 (2005). Article CAS PubMed Google Scholar * Feighner, S. D. & Hylemon, P. B. Characterization of a corticosteroid 21-dehydroxylase from
the intestinal anaerobic bacterium, _Eubacterium lentum_. _J. Lipid Res._ 21, 585–593 (1980). Article CAS PubMed Google Scholar * Kumar, A., Ellermann, M. & Sperandio, V. Taming the
beast: interplay between gut small molecules and enteric pathogens. _Infect. Immun._ 87, 277 (2019). Article Google Scholar * Cameron, E. A. & Sperandio, V. Frenemies: signaling and
nutritional integration in pathogen–microbiota–host interactions. _Cell Host Microbe_ 18, 275–284 (2015). Article CAS PubMed PubMed Central Google Scholar * Manfredo Vieira, S. et al.
Translocation of a gut pathobiont drives autoimmunity in mice and humans. _Science_ 359, 1156–1161 (2018). Article CAS PubMed Google Scholar * Aykut, B. et al. The fungal mycobiome
promotes pancreatic oncogenesis via activation of MBL. _Nature_ 574, 264–267 (2019). Article CAS PubMed PubMed Central Google Scholar * Wortelboer, K., Nieuwdorp, M. & Herrema, H.
Fecal microbiota transplantation beyond _Clostridioides difficile_ infections. _EBioMedicine_ 44, 716–729 (2019). Article PubMed PubMed Central Google Scholar * Willing, B. P.,
Vacharaksa, A., Croxen, M., Thanachayanont, T. & Finlay, B. B. Altering host resistance to infections through microbial transplantation. _PLoS ONE_ 6, e26988 (2011). Article CAS PubMed
PubMed Central Google Scholar * Buffie, C. G. et al. Precision microbiome reconstitution restores bile acid mediated resistance to _Clostridium_ _difficile_. _Nature_ 517, 205–208
(2015). Article CAS PubMed Google Scholar * Vuong, H. E., Yano, J. M., Fung, T. C. & Hsiao, E. Y. The microbiome and host behavior. _Annu. Rev. Neurosci._ 40, 21–49 (2017). Article
CAS PubMed PubMed Central Google Scholar * Scheperjans, F. et al. Gut microbiota are related to Parkinson’s disease and clinical phenotype. _Mov. Disord._ 30, 350–358 (2015). Article
PubMed Google Scholar * Keshavarzian, A. et al. Colonic bacterial composition in Parkinson’s disease. _Mov. Disord._ 30, 1351–1360 (2015). Article CAS PubMed Google Scholar * Peng, A.
et al. Altered composition of the gut microbiome in patients with drug-resistant epilepsy. _Epilepsy Res._ 147, 102–107 (2018). Article CAS PubMed Google Scholar * Xie, G. et al.
Ketogenic diet poses a significant effect on imbalanced gut microbiota in infants with refractory epilepsy. _World J. Gastroenterol._ 23, 6164–6171 (2017). Article CAS PubMed PubMed
Central Google Scholar * Naseribafrouei, A. et al. Correlation between the human fecal microbiota and depression. _Neurogastroenterol. Motil._ 26, 1155–1162 (2014). Article CAS PubMed
Google Scholar * Jiang, H. et al. Altered fecal microbiota composition in patients with major depressive disorder. _Brain Behav. Immun._ 48, 186–194 (2015). Article PubMed Google Scholar
* Cekanaviciute, E. et al. Gut bacteria from multiple sclerosis patients modulate human T cells and exacerbate symptoms in mouse models. _Proc. Natl Acad. Sci. USA_ 114, 10713–10718
(2017). Article CAS PubMed PubMed Central Google Scholar * Berer, K. et al. Gut microbiota from multiple sclerosis patients enables spontaneous autoimmune encephalomyelitis in mice.
_Proc. Natl Acad. Sci. USA_ 114, 10719–10724 (2017). Article CAS PubMed PubMed Central Google Scholar * De Angelis, M. et al. Fecal microbiota and metabolome of children with autism and
pervasive developmental disorder not otherwise specified. _PLoS ONE_ 8, e76993 (2013). Article PubMed PubMed Central CAS Google Scholar * Kang, D.-W. et al. Reduced incidence of
_Prevotella_ and other fermenters in intestinal microflora of autistic children. _PLoS ONE_ 8, e68322 (2013). Article CAS PubMed PubMed Central Google Scholar * Sharon, G. et al. Human
gut microbiota from autism spectrum disorder promote behavioral symptoms in mice. _Cell_ 177, 1600–1618 (2019). Article CAS PubMed PubMed Central Google Scholar * Sampson, T. R. et al.
Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease. _Cell_ 167, 1469–1480 (2016). Article CAS PubMed PubMed Central Google Scholar * Berer,
K. et al. Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. _Nature_ 479, 538–541 (2011). Article CAS PubMed Google Scholar * Kim, S. et al.
Maternal gut bacteria promote neurodevelopmental abnormalities in mouse offspring. _Nature_ 549, 528–532 (2017). Article PubMed PubMed Central CAS Google Scholar * Blacher, E. et al.
Potential roles of gut microbiome and metabolites in modulating ALS in mice. _Nature_ 572, 474–480 (2019). Article CAS PubMed Google Scholar * Olson, C. A. et al. The gut microbiota
mediates the anti-seizure effects of the ketogenic diet. _Cell_ 173, 1728–1741 (2018). Article CAS PubMed PubMed Central Google Scholar * Chu, C. et al. The microbiota regulate neuronal
function and fear extinction learning. _Nature_ 574, 543–548 (2019). Article CAS PubMed PubMed Central Google Scholar * Makkawi, S., Camara-Lemarroy, C. & Metz, L. Fecal microbiota
transplantation associated with 10 years of stability in a patient with SPMS. _Neurol. Neuroimmunol. Neuroinflamm._ 5, e459 (2018). Article PubMed PubMed Central Google Scholar * Kang,
D.-W. et al. Microbiota transfer therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. _Microbiome_ 5, 10 (2017). Article PubMed PubMed
Central Google Scholar * He, Z. et al. Fecal microbiota transplantation cured epilepsy in a case with Crohn’s disease: the first report. _World J. Gastroenterol._ 23, 3565–3568 (2017).
Article PubMed PubMed Central Google Scholar * Hang, S. et al. Bile acid metabolites control TH17 and Treg cell differentiation. _Nature_ 576, 143–148 (2019). Article CAS PubMed
PubMed Central Google Scholar * Strandwitz, P. et al. GABA-modulating bacteria of the human gut microbiota. _Nat. Microbiol._ 4, 396–403 (2019). Article CAS PubMed Google Scholar *
Luscher, B., Shen, Q. & Sahir, N. The GABAergic deficit hypothesis of major depressive disorder. _Mol. Psychiatry_ 16, 383–406 (2011). Article CAS PubMed Google Scholar * Devlin, A.
S. et al. Modulation of a circulating uremic solute via rational genetic manipulation of the gut microbiota. _Cell Host Microbe_ 20, 709–715 (2016). Article CAS PubMed PubMed Central
Google Scholar * Yu, E. W. et al. Fecal microbiota transplantation for the improvement of metabolism in obesity: the FMT-TRIM double-blind placebo-controlled pilot trial. _PLoS Med._ 17,
e1003051 (2020). Article PubMed PubMed Central CAS Google Scholar * Young, M. T., Phelan, M. J. & Nguyen, N. T. A decade analysis of trends and outcomes of male vs female patients
who underwent bariatric surgery. _J. Am. Coll. Surg._ 222, 226–231 (2016). Article PubMed Google Scholar * DeFilipp, Z. et al. Drug-resistant _E. coli_ bacteremia transmitted by fecal
microbiota transplant. _N. Engl. J. Med._ 381, 2043–2050 (2019). Article PubMed Google Scholar * Depommier, C. et al. Supplementation with _Akkermansia muciniphila_ in overweight and
obese human volunteers: a proof-of-concept exploratory study. _Nat. Med._ 25, 1096–1103 (2019). Article CAS PubMed PubMed Central Google Scholar * Chiang, J. Y. L. & Ferrell, J. M.
Bile acids as metabolic regulators and nutrient sensors. _Annu. Rev. Nutr._ 39, 175–200 (2019). Article CAS PubMed PubMed Central Google Scholar * Bedford, A. & Gong, J.
Implications of butyrate and its derivatives for gut health and animal production. _Anim. Nutr._ 4, 151–159 (2018). Article PubMed Google Scholar * Sato, F. T. et al. Tributyrin
attenuates metabolic and inflammatory changes associated with obesity through a GPR109A-dependent mechanism. _Cells_ 9, 2007 (2020). Article CAS PubMed Central Google Scholar * Nguyen,
T. D., Prykhodko, O., Hållenius, F. F. & Nyman, M. Monobutyrin reduces liver cholesterol and improves intestinal barrier function in rats fed high-fat diets. _Nutrients_ 11, 308 (2019).
Article CAS PubMed Central Google Scholar * Yao, L. et al. A selective gut bacterial bile salt hydrolase alters host metabolism. _eLife_ 7, e37182 (2018). Article PubMed PubMed Central
Google Scholar * Bai, L. et al. Engineered butyrate-producing bacteria prevents high fat diet-induced obesity in mice. _Microbe Cell Fact._ 19, 94–13 (2020). Article CAS Google Scholar
* Larsen, N. et al. Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. _PLoS ONE_ 5, e9085 (2010). Article PubMed PubMed Central CAS Google Scholar
* Kan, H., Zhao, F., Zhang, X. X., Ren, H. & Gao, S. Correlations of gut microbial community shift with hepatic damage and growth inhibition of _Carassius auratus_ induced by
pentachlorophenol exposure. _Environ. Sci. Technol._ 49, 11894–11902 (2015). Article CAS PubMed Google Scholar * Haro, C. et al. Intestinal microbiota is influenced by gender and body
mass index. _PLoS ONE_ 11, e0154090 (2016). Article PubMed PubMed Central CAS Google Scholar * Patil, D. P. et al. Molecular analysis of gut microbiota in obesity among Indian
individuals. _J. Biosci._ 37, 647–657 (2012). Article CAS PubMed Google Scholar * Mullish, B. H. & Williams, H. R. _Clostridium difficile_ infection and antibiotic-associated
diarrhoea. _Clin. Med._ 18, 237–241 (2018). Article Google Scholar * Zheng, P. et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s
metabolism. _Mol. Psychiatry_ 21, 786 (2016). Article CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS This work was supported by National Institutes of Health grants R35
GM128618 and R01 DK126855 (A.S.D.). S.N.C. acknowledges an American Heart Association Postdoctoral Fellowship. M.D.M. acknowledges an NSF Graduate Research Fellowship (DGE1745303). Figures
created with BioRender.com. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Biological Chemistry and Molecular Pharmacology, Blavatnik Institute, Harvard Medical School, Boston,
MA, USA Snehal N. Chaudhari, Megan D. McCurry & A. Sloan Devlin Authors * Snehal N. Chaudhari View author publications You can also search for this author inPubMed Google Scholar * Megan
D. McCurry View author publications You can also search for this author inPubMed Google Scholar * A. Sloan Devlin View author publications You can also search for this author inPubMed
Google Scholar CORRESPONDING AUTHORS Correspondence to Snehal N. Chaudhari or A. Sloan Devlin. ETHICS DECLARATIONS COMPETING INTERESTS A.S.D. is an ad hoc consultant for Takeda
Pharmaceuticals and Axial Therapeutics. The other authors have declared no competing interests. ADDITIONAL INFORMATION PEER REVIEW INFORMATION _Nature Chemical Biology_ thanks Andrew Gewirtz
and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in
published maps and institutional affiliations. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Chaudhari, S.N., McCurry, M.D. & Devlin, A.S. Chains
of evidence from correlations to causal molecules in microbiome-linked diseases. _Nat Chem Biol_ 17, 1046–1056 (2021). https://doi.org/10.1038/s41589-021-00861-z Download citation *
Received: 01 September 2020 * Accepted: 16 July 2021 * Published: 22 September 2021 * Issue Date: October 2021 * DOI: https://doi.org/10.1038/s41589-021-00861-z SHARE THIS ARTICLE Anyone you
share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the
Springer Nature SharedIt content-sharing initiative
