Genomic and transcriptomic determinants of response to neoadjuvant therapy in rectal cancer
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

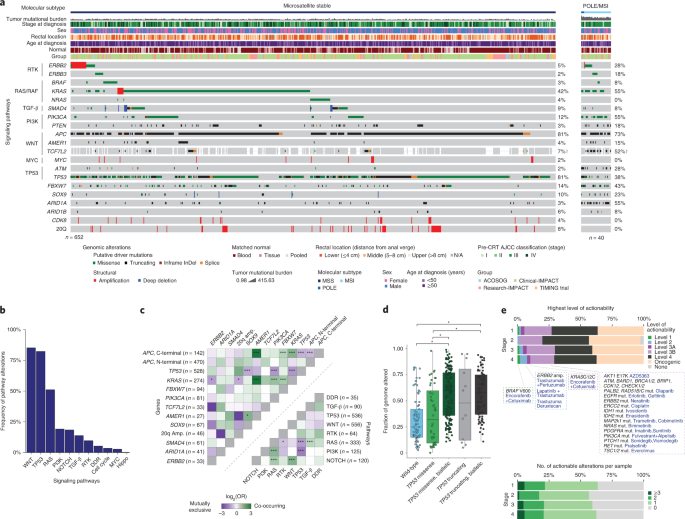
ABSTRACT The incidence of rectal cancer is increasing in patients younger than 50 years. Locally advanced rectal cancer is still treated with neoadjuvant radiation, chemotherapy and surgery,
but recent evidence suggests that patients with a complete response can avoid surgery permanently. To define correlates of response to neoadjuvant therapy, we analyzed genomic and
transcriptomic profiles of 738 untreated rectal cancers. _APC_ mutations were less frequent in the lower than in the middle and upper rectum, which could explain the more aggressive behavior
of distal tumors. No somatic alterations had significant associations with response to neoadjuvant therapy in a treatment-agnostic manner, but _KRAS_ mutations were associated with faster
relapse in patients treated with neoadjuvant chemoradiation followed by consolidative chemotherapy. Overexpression of _IGF2_ and _L1CAM_ was associated with decreased response to neoadjuvant
therapy. RNA-sequencing estimates of immune infiltration identified a subset of microsatellite-stable immune hot tumors with increased response and prolonged disease-free survival. Access
through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Access Nature and 54 other
Nature Portfolio journals Get Nature+, our best-value online-access subscription $29.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12 print issues and online
access $209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which
are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS
COMPREHENSIVE ASSESSMENT OF ACTIONABLE GENOMIC ALTERATIONS IN PRIMARY COLORECTAL CARCINOMA USING TARGETED NEXT-GENERATION SEQUENCING Article Open access 16 July 2022 TUMOR LOCATION MATTERS,
NEXT GENERATION SEQUENCING MUTATION PROFILING OF LEFT-SIDED, RECTAL, AND RIGHT-SIDED COLORECTAL TUMORS IN 552 PATIENTS Article Open access 26 February 2024 TUMOR MICROENVIRONMENT-ADJUSTED
PROGNOSTIC IMPLICATIONS OF THE _KRAS_ MUTATION SUBTYPE IN PATIENTS WITH STAGE III COLORECTAL CANCER TREATED WITH ADJUVANT FOLFOX Article Open access 16 July 2021 DATA AVAILABILITY All
genomic results and associated clinical data for all of the patients in this study have been deposited in the cBioPortal for Cancer Genomics55,56 and are publicly available for browsing and
bulk download at https://www.cbioportal.org/study/summary?id=rectal_msk_2022. The raw RNA sequencing data have also been deposited in GEO (accession number GSE209746 available at
https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE209746). The raw DNA sequencing data are protected; de-identified data are available under restricted access to protect patient privacy
in accordance with Federal and State law. These data can be requested for research use from the corresponding author. Data will be shared for a span of 2 years within 2 weeks of execution of
a data transfer agreement with MSK, which will retain all title and rights to the data and results from their use. The OncoKB knowledge base that we used to annotate genomic alterations is
publicly available at https://www.oncokb.org/. TCGA data used for comparison are available via the Genomic Data Commons Portal (https://portal.gdc.cancer.gov/). CODE AVAILABILITY The
mutational signature decomposition code can be found at https://github.com/mskcc/tempoSig. The OncoKB annotator tool is also available through its own GitHub repository at
https://github.com/oncokb. Additional custom written tools and programs used for the analysis of MSK-IMPACT data are available through the MSK GitHub repository at https://github.com/mskcc.
REFERENCES * Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer Statistics, 2021. _CA Cancer J. Clin._ 71, 7–33 (2021). Article PubMed Google Scholar * Saad El Din, K. et
al. Trends in the epidemiology of young-onset colorectal cancer: a worldwide systematic review. _BMC Cancer_ 20, 288 (2020). Article PubMed Google Scholar * Marr, R. et al. The modern
abdominoperineal excision: the next challenge after total mesorectal excision. _Ann. Surg._ 242, 74–82 (2005). Article PubMed PubMed Central Google Scholar * Smith, J. J. et al.
Assessment of a watch-and-wait strategy for rectal cancer in patients with a complete response after neoadjuvant therapy. _JAMA Oncol._ 5, e185896 (2019). Article PubMed PubMed Central
Google Scholar * Garcia-Aguilar, J. et al. Organ preservation in patients with rectal adenocarcinoma treated with total neoadjuvant therapy. _J. Clin. Oncol._
https://doi.org/10.1200/JCO.22.00032 (2022). * Garcia-Aguilar, J. et al. Effect of adding mFOLFOX6 after neoadjuvant chemoradiation in locally advanced rectal cancer: a multicentre, phase 2
trial. _Lancet Oncol._ 16, 957–966 (2015). Article CAS PubMed PubMed Central Google Scholar * Probst, C. P. et al. Extended intervals after neoadjuvant therapy in locally advanced
rectal cancer: the key to improved tumor response and potential organ preservation. _J. Am. Coll. Surg._ 221, 430–440 (2015). Article PubMed PubMed Central Google Scholar *
Garcia-Aguilar, J. et al. Identification of a biomarker profile associated with resistance to neoadjuvant chemoradiation therapy in rectal cancer. _Ann. Surg._ 254, 486–492 (2011). Article
PubMed Google Scholar * Chow, O. S. et al. KRAS and combined KRAS/TP53 mutations in locally advanced rectal cancer are independently associated with decreased response to neoadjuvant
therapy. _Ann. Surg. Oncol._ 23, 2548–2555 (2016). Article PubMed PubMed Central Google Scholar * Kamran, S. C. et al. Integrative molecular characterization of resistance to neoadjuvant
chemoradiation in rectal cancer. _Clin. Cancer Res._ 25, 5561–5571 (2019). Article CAS PubMed PubMed Central Google Scholar * Cancer Genome Atlas Network. Comprehensive molecular
characterization of human colon and rectal cancer. _Nature_ 487, 330–337 (2012). Article CAS Google Scholar * Liu, Y. et al. Comparative molecular analysis of gastrointestinal
adenocarcinomas. _Cancer Cell_ 33, 721–735 (2018). Article CAS PubMed PubMed Central Google Scholar * Garcia-Aguilar, J. et al. Organ preservation for clinical T2N0 distal rectal cancer
using neoadjuvant chemoradiotherapy and local excision (ACOSOG Z6041): results of an open-label, single-arm, multi-institutional, phase 2 trial. _Lancet Oncol._ 16, 1537–1546 (2015).
Article PubMed PubMed Central Google Scholar * Sanchez-Vega, F. et al. Oncogenic signaling pathways in the cancer genome atlas. _Cell_ 173, 321–337. (2018). Article CAS PubMed PubMed
Central Google Scholar * Mondaca, S. et al. Specific mutations in APC, but not alterations in DNA damage response, associate with outcomes of patients with metastatic colorectal cancer.
_Gastroenterology_ 159, 1975–1978 (2020). Article CAS PubMed Google Scholar * Bielski, C. M. et al. Genome doubling shapes the evolution and prognosis of advanced cancers. _Nat. Genet._
50, 1189–1195 (2018). Article CAS PubMed PubMed Central Google Scholar * Ciriello, G. et al. Emerging landscape of oncogenic signatures across human cancers. _Nat. Genet._ 45, 1127–1133
(2013). Article CAS PubMed PubMed Central Google Scholar * Taylor, A. M. et al. Genomic and functional approaches to understanding cancer aneuploidy. _Cancer Cell_ 33, 676–689. (2018).
Article CAS PubMed PubMed Central Google Scholar * Lawrence, M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. _Nature_ 499, 214–218
(2013). Article CAS PubMed PubMed Central Google Scholar * Chakravarty, D. et al. Oncokb: a precision oncology knowledge base. _JCO Precis. Oncol._ 2017, PO.17.00011 (2017). Google
Scholar * Infante, J. R. et al. Safety, pharmacokinetic, pharmacodynamic, and efficacy data for the oral MEK inhibitor trametinib: a phase 1 dose-escalation trial. _Lancet Oncol._ 13,
773–781 (2012). Article CAS PubMed Google Scholar * Cleary, J. M. et al. Differential outcomes in codon 12/13 and codon 61 NRAS-mutated cancers in the phase II NCI-MATCH trial of
binimetinib in patients with NRAS-mutated tumors. _Clin. Cancer Res._ 27, 2996–3004 (2021). Article CAS PubMed PubMed Central Google Scholar * Bendell, J. C. et al. Phase I,
dose-escalation study of BKM120, an oral pan-class I PI3K inhibitor, in patients with advanced solid tumors. _J. Clin. Oncol._ 30, 282–290 (2012). Article CAS PubMed Google Scholar * van
Geel, R. M. J. M. et al. A phase Ib dose-escalation study of encorafenib and cetuximab with or without alpelisib in metastatic BRAF-mutant colorectal cancer. _Cancer Discov._ 7, 610–619
(2017). Article PubMed PubMed Central CAS Google Scholar * Yaeger, R. et al. Clinical sequencing defines the genomic landscape of metastatic colorectal cancer. _Cancer Cell_ 33, 125–136
(2018). Article CAS PubMed PubMed Central Google Scholar * Roxburgh, C. S. D. et al. Changes in the multidisciplinary management of rectal cancer from 2009 to 2015 and associated
improvements in short-term outcomes. _Colorectal Dis._ 21, 1140–1150 (2019). Article CAS PubMed PubMed Central Google Scholar * Cercek, A. et al. Mismatch repair-deficient rectal cancer
and resistance to neoadjuvant chemotherapy. _Clin. Cancer Res._ 26, 3271–3279 (2020). Article CAS PubMed PubMed Central Google Scholar * Guinney, J. et al. The consensus molecular
subtypes of colorectal cancer. _Nat. Med._ 21, 1350–1356 (2015). Article CAS PubMed PubMed Central Google Scholar * Korkeila, E. et al. Expression of carbonic anhydrase IX suggests poor
outcome in rectal cancer. _Br. J. Cancer_ 100, 874–880 (2009). Article CAS PubMed PubMed Central Google Scholar * Lee-Kong, S. A. et al. Hypoxia-related proteins in patients with
rectal cancer undergoing neoadjuvant combined modality therapy. _Dis. Colon Rectum_ 55, 990–995 (2012). Article PubMed Google Scholar * Ganesh, K. et al. L1CAM defines the regenerative
origin of metastasis-initiating cells in colorectal cancer. _Nat. Cancer_ 1, 28–45 (2020). Article CAS PubMed PubMed Central Google Scholar * Bindea, G. et al. Spatiotemporal dynamics
of intratumoral immune cells reveal the immune landscape in human cancer. _Immunity_ 39, 782–795 (2013). Article CAS PubMed Google Scholar * Davoli, T., Uno, H., Wooten, E. C. &
Elledge, S. J. Tumor aneuploidy correlates with markers of immune evasion and with reduced response to immunotherapy. _Science_ 355, eaaf8399 (2017). Article PubMed PubMed Central CAS
Google Scholar * Chen, D. S. & Mellman, I. Oncology meets immunology: the cancer–immunity cycle. _Immunity_ 39, 1–10 (2013). Article PubMed CAS Google Scholar * Liberzon, A. et al.
The Molecular Signatures Database (MSigDB) hallmark gene set collection. _Cell Syst._ 1, 417–425 (2015). Article CAS PubMed PubMed Central Google Scholar * Nishimura, T. et al. The
critical role of Th1-dominant immunity in tumor immunology. _Cancer Chemother. Pharmacol._ 46, S52–S61 (2000). Article CAS PubMed Google Scholar * Lee, M. S., Menter, D. G. & Kopetz,
S. Right versus left colon cancer biology: integrating the consensus molecular subtypes. _J. Natl Compr. Canc. Netw._ 15, 411–419 (2017). Article PubMed Google Scholar * Νikolouzakis, Τ.
Κ. et al. Detailed and applied anatomy for improved rectal cancer treatment. _Ann. Gastroenterol._ 32, 431–440 (2019). Google Scholar * Cheng, L.-J. et al. Distinct prognosis of high
versus mid/low rectal cancer: a propensity score-matched cohort study. _J. Gastrointest. Surg._ 23, 1474–1484 (2019). Article PubMed Google Scholar * Yang, H. et al. Influence of tumor
location on short- and long-term outcomes after laparoscopic surgery for rectal cancer: a propensity score matched cohort study. _BMC Cancer_ 20, 761 (2020). Article PubMed PubMed Central
Google Scholar * Nagtegaal, I. D. et al. Low rectal cancer: a call for a change of approach in abdominoperineal resection. _J. Clin. Oncol._ 23, 9257–9264 (2005). Article PubMed Google
Scholar * Patel, S. V. et al. Distance to the anal verge is associated with pathologic complete response to neoadjuvant therapy in locally advanced rectal cancer. _J. Surg. Oncol._ 114,
637–641 (2016). Article CAS PubMed PubMed Central Google Scholar * Kim, J. K. et al. KRAS mutant rectal cancer cells interact with surrounding fibroblasts to deplete the extracellular
matrix. _Mol. Oncol._ 15, 2766–2781 (2021). Article PubMed PubMed Central CAS Google Scholar * Francois, Y. et al. Influence of the interval between preoperative radiation therapy and
surgery on downstaging and on the rate of sphincter-sparing surgery for rectal cancer: the Lyon R90-01 randomized trial. _J. Clin. Oncol._ 17, 2396 (1999). Article CAS PubMed Google
Scholar * Moore, H. G. et al. Rate of pathologic complete response with increased interval between preoperative combined modality therapy and rectal cancer resection. _Dis. Colon Rectum_
47, 279–286 (2004). Article PubMed Google Scholar * Le, D. T. et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. _Science_ 357, 409–413 (2017). Article
CAS PubMed PubMed Central Google Scholar * Ganesh, K. et al. Immunotherapy in colorectal cancer: rationale, challenges and potential. _Nat. Rev. Gastroenterol. Hepatol._ 16, 361–375
(2019). Article PubMed PubMed Central Google Scholar * Rahma, O. E. et al. Use of total neoadjuvant therapy for locally advanced rectal cancer: initial results from the pembrolizumab arm
of a phase 2 randomized clinical trial. _JAMA Oncol._ 7, 1225–1230 (2021). Article PubMed Google Scholar * Pagès, F. et al. International validation of the consensus Immunoscore for the
classification of colon cancer: a prognostic and accuracy study. _Lancet_ 391, 2128–2139 (2018). Article PubMed Google Scholar * El Sissy, C. et al. A diagnostic biopsy-adapted
immunoscore predicts response to neoadjuvant treatment and selects patients with rectal cancer eligible for a watch-and-wait strategy. _Clin. Cancer Res._ 26, 5198–5207 (2020). Article CAS
PubMed Google Scholar * Kirilovsky, A. et al. The “Immunoscore” in rectal cancer: could we search quality beyond quantity of life? _Oncotarget_ 13, 18–31 (2022). Article PubMed PubMed
Central Google Scholar * Zanella, E. R. et al. IGF2 is an actionable target that identifies a distinct subpopulation of colorectal cancer patients with marginal response to anti-EGFR
therapies. _Sci. Transl. Med._ 7, 272ra12 (2015). Article PubMed CAS Google Scholar * Smith, J. J. et al. Organ Preservation in Rectal Adenocarcinoma: a phase II randomized controlled
trial evaluating 3-year disease-free survival in patients with locally advanced rectal cancer treated with chemoradiation plus induction or consolidation chemotherapy, and total mesorectal
excision or nonoperative management. _BMC Cancer_ 15, 767 (2015). Article PubMed PubMed Central CAS Google Scholar * Schrag, D. et al. Challenges and solutions in the design and
execution of the PROSPECT phase II/III neoadjuvant rectal cancer trial (NCCTG N1048/Alliance). _Clin. Trials_ 16, 165–175 (2019). Article PubMed PubMed Central Google Scholar * Cerami,
E. et al. The cBio Cancer Genomics Portal: an open platform for exploring multidimensional cancer genomics data. _Cancer Discov._ 2, 401–404 (2012). Article PubMed Google Scholar * Gao,
J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. _Sci. Signal._ 6, pl1 (2013). Article PubMed PubMed Central CAS Google Scholar *
Cheng, D. T. et al. Memorial Sloan Kettering–Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT): a hybridization capture-based next-generation sequencing clinical assay
for solid tumor molecular oncology. _J. Mol. Diagn._ 17, 251–264 (2015). Article CAS PubMed PubMed Central Google Scholar * Zehir, A. et al. Mutational landscape of metastatic cancer
revealed from prospective clinical sequencing of 10,000 patients. _Nat. Med._ 23, 703–713 (2017). Article CAS PubMed PubMed Central Google Scholar * Shen, R. & Seshan, V. E. FACETS:
allele-specific copy number and clonal heterogeneity analysis tool for high-throughput DNA sequencing. _Nucleic Acids Res._ 44, e131 (2016). Article PubMed PubMed Central CAS Google
Scholar * Bielski, C. M. et al. Widespread selection for oncogenic mutant allele imbalance in cancer. _Cancer Cell_ 34, 852–862 (2018). Article CAS PubMed PubMed Central Google Scholar
* Niu, B. et al. MSIsensor: microsatellite instability detection using paired tumor–normal sequence data. _Bioinformatics_ 30, 1015–1016 (2014). Article CAS PubMed Google Scholar *
Middha, S. et al. Reliable pan-cancer microsatellite instability assessment by using targeted next-generation sequencing data. _JCO Precis. Oncol._ 2017, PO.17.00084 (2017). Google Scholar
* Alexandrov, L. B. et al. The repertoire of mutational signatures in human cancer. _Nature_ 578, 94–101 (2020). Article CAS PubMed PubMed Central Google Scholar * Love, M. I., Huber,
W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. _Genome Biol._ 15, 550 (2014). Article PubMed PubMed Central CAS Google Scholar *
Durinck, S., Spellman, P. T., Birney, E. & Huber, W. Mapping identifiers for the integration of genomic datasets with the R/Bioconductor package biomaRt. _Nat. Protoc._ 4, 1184–1191
(2009). Article CAS PubMed PubMed Central Google Scholar * Hänzelmann, S., Castelo, R. & Guinney, J. GSVA: gene set variation analysis for microarray and RNA-seq data. _BMC
Bioinformatics_ 14, 7 (2013). Article PubMed PubMed Central Google Scholar * Eide, P. W., Bruun, J., Lothe, R. A. & Sveen, A. CMScaller: an R package for consensus molecular
subtyping of colorectal cancer pre-clinical models. _Sci. Rep._ 7, 16618 (2017). Article PubMed PubMed Central CAS Google Scholar * Thorsson, V. et al. The immune landscape of cancer.
_Immunity_ 48, 812–830 (2018). Article CAS PubMed PubMed Central Google Scholar * Salgado, R. et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer:
recommendations by an International TILs Working Group 2014. _Ann. Oncol._ 26, 259–271 (2015). Article CAS PubMed Google Scholar * Budinska, E. et al. Gene expression patterns unveil a
new level of molecular heterogeneity in colorectal cancer. _J. Pathol._ 231, 63–76 (2013). Article CAS PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS The
authors acknowledge the use of services provided by the Molecular Cytology Core Facility, funded by the National Cancer Institute (NCI) Cancer Center Support Grant (CCSG, P30 CA008748-53).
The authors also acknowledge the use of the Integrated Genomics Operation Core, funded by the NCI Cancer Center Support Grant (CCSG, P30 CA08748), Cycle for Survival, and the Marie-Josée and
Henry R. Kravis Center for Molecular Oncology. W.K.C. is supported by a National Institutes of Health (NIH) research training grant (T32 GM132083). P.B.R. is supported by an NIH/NCI early
career development award (K08 CA255574). J.J.S. is supported by an NIH/NCI R37 248289 award. The content is solely the responsibility of the authors and does not necessarily represent the
official views of the NIH. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Marie-Josée and Henry R. Kravis Center for Molecular Oncology, Memorial Sloan Kettering Cancer Center, New York, NY,
USA Walid K. Chatila, Henry Walch, Anisha Luthra, Ritika Kundra, S. Duygu Selcuklu, Mark T. A. Donoghue, David B. Solit, Michael F. Berger & Nikolaus Schultz * Department of Epidemiology
and Biostatistics, Memorial Sloan Kettering Cancer Center, New York, NY, USA Walid K. Chatila, Henry Walch, Anisha Luthra, Ritika Kundra, Nikolaus Schultz & Francisco Sanchez-Vega *
Tri-Institutional Program in Computational Biology and Medicine, Weill Cornell Medical College, New York, NY, USA Walid K. Chatila * Colorectal Service, Department of Surgery, Memorial Sloan
Kettering Cancer Center, New York, NY, USA Jin K. Kim, Michael R. Marco, Chin-Tung Chen, Fan Wu, Dana M. Omer, Xuan Qu, Anisha Luthra, Seo-Hyun Choi, Katharine I. Groves, Martin R. Weiser,
Maria Widmar, Iris H. Wei, Emmanouil P. Pappou, Garrett M. Nash, Philip B. Paty, Raphael Pelossof, J. Joshua Smith, Francisco Sanchez-Vega & Julio Garcia-Aguilar * Colorectal Cancer
Research Center, Memorial Sloan Kettering Cancer Center, New York, NY, USA Chin-Tung Chen, Fan Wu, Karuna Ganesh, Andrea Cercek, Martin R. Weiser, Emmanouil P. Pappou, Philip B. Paty,
Efsevia Vakiani, Jinru Shia, Raphael Pelossof, Paul B. Romesser, Rona Yaeger, J. Joshua Smith, Francisco Sanchez-Vega & Julio Garcia-Aguilar * Department of Medicine, Memorial Sloan
Kettering Cancer Center, New York, NY, USA Danny N. Khalil, Karuna Ganesh, Andrea Cercek, David B. Solit, Paul B. Romesser & Rona Yaeger * Parker Institute for Cancer Immunotherapy, New
York, NY, USA Danny N. Khalil * Weill Cornell Medicine, New York, NY, USA Danny N. Khalil * Cancer Biology and Genetics Program, Memorial Sloan Kettering Cancer Center, New York, NY, USA
Yu-Jui Ho * Human Oncology and Pathogenesis Program, Memorial Sloan Kettering Cancer Center, New York, NY, USA Katharine I. Groves, Michael F. Berger & J. Joshua Smith * Department of
Cardiothoracic Surgery, Weill Cornell Medicine, New York-Presbyterian, New York, NY, USA Oliver S. Chow * Department of Quantitative Health Sciences, Mayo Clinic, Rochester, MN, USA Qian Shi
* Department of Pathology and Laboratory Medicine, Memorial Sloan Kettering Cancer Center, New York, NY, USA Efsevia Vakiani, Michael F. Berger & Jinru Shia * Department of Radiation
Oncology, Memorial Sloan Kettering Cancer Center, New York, NY, USA Paul B. Romesser Authors * Walid K. Chatila View author publications You can also search for this author inPubMed Google
Scholar * Jin K. Kim View author publications You can also search for this author inPubMed Google Scholar * Henry Walch View author publications You can also search for this author inPubMed
Google Scholar * Michael R. Marco View author publications You can also search for this author inPubMed Google Scholar * Chin-Tung Chen View author publications You can also search for this
author inPubMed Google Scholar * Fan Wu View author publications You can also search for this author inPubMed Google Scholar * Dana M. Omer View author publications You can also search for
this author inPubMed Google Scholar * Danny N. Khalil View author publications You can also search for this author inPubMed Google Scholar * Karuna Ganesh View author publications You can
also search for this author inPubMed Google Scholar * Xuan Qu View author publications You can also search for this author inPubMed Google Scholar * Anisha Luthra View author publications
You can also search for this author inPubMed Google Scholar * Seo-Hyun Choi View author publications You can also search for this author inPubMed Google Scholar * Yu-Jui Ho View author
publications You can also search for this author inPubMed Google Scholar * Ritika Kundra View author publications You can also search for this author inPubMed Google Scholar * Katharine I.
Groves View author publications You can also search for this author inPubMed Google Scholar * Oliver S. Chow View author publications You can also search for this author inPubMed Google
Scholar * Andrea Cercek View author publications You can also search for this author inPubMed Google Scholar * Martin R. Weiser View author publications You can also search for this author
inPubMed Google Scholar * Maria Widmar View author publications You can also search for this author inPubMed Google Scholar * Iris H. Wei View author publications You can also search for
this author inPubMed Google Scholar * Emmanouil P. Pappou View author publications You can also search for this author inPubMed Google Scholar * Garrett M. Nash View author publications You
can also search for this author inPubMed Google Scholar * Philip B. Paty View author publications You can also search for this author inPubMed Google Scholar * Qian Shi View author
publications You can also search for this author inPubMed Google Scholar * Efsevia Vakiani View author publications You can also search for this author inPubMed Google Scholar * S. Duygu
Selcuklu View author publications You can also search for this author inPubMed Google Scholar * Mark T. A. Donoghue View author publications You can also search for this author inPubMed
Google Scholar * David B. Solit View author publications You can also search for this author inPubMed Google Scholar * Michael F. Berger View author publications You can also search for this
author inPubMed Google Scholar * Jinru Shia View author publications You can also search for this author inPubMed Google Scholar * Raphael Pelossof View author publications You can also
search for this author inPubMed Google Scholar * Paul B. Romesser View author publications You can also search for this author inPubMed Google Scholar * Rona Yaeger View author publications
You can also search for this author inPubMed Google Scholar * J. Joshua Smith View author publications You can also search for this author inPubMed Google Scholar * Nikolaus Schultz View
author publications You can also search for this author inPubMed Google Scholar * Francisco Sanchez-Vega View author publications You can also search for this author inPubMed Google Scholar
* Julio Garcia-Aguilar View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS W.K.C., F.S.-V. and J.G.-A. conceived and designed the study in
concert with N.S., R.Y. and J.J.S. A.C., M.R.W., M.W., I.H.W., E.P.P., G.M.N., P.B.P., Q.S., K.G., R.Y., J.J.S. and J.G.-A. provided patient samples and clinical information. C.-T.C.,
S.-H.C., M.R.M., J.K.K., O.S.C. and M.F.B. generated genomic data. J.K.K., M.R.M., C.-T.C., D.M.O., K.I.G. and J.G.-A. annotated patient samples and curated the clinical data. W.K.C.,
F.S.-V., H.W., K.G., X.Q., F.W., P.B.R. and J.G.-A. performed data analysis and interpretation. J.S. and E.V. carried out the histopathologic analyses. D.N.K. interpreted the immunology
results. S.D.S. carried out the project management. W.K.C., H.W., F.W., X.Q., R.P., R.K., M.T.A.D., Y.-J.H., A.L., M.F.B., F.S.V. and N.S., provided bioinformatic support for data analysis,
annotation, visualization and dissemination. M.F.B., D.B.S. and N.S. provided support as part of the institutional MSK-IMPACT sequencing initiative. W.K.C., H.W., R.Y., J.J.S., N.S., F.S.-V.
and J.G.-A. wrote the manuscript. All authors reviewed and approved the manuscript. N.S., R.Y., F.S.-V. and J.G.-A. provided resources and funding for this work. F.S.-V. and J.G.-A.
supervised the study. CORRESPONDING AUTHORS Correspondence to Francisco Sanchez-Vega or Julio Garcia-Aguilar. ETHICS DECLARATIONS COMPETING INTERESTS D.N.K. has been a consultant for Merck
Sharp & Dohme with regard to intellectual property rights and for AbbVie and PsiOxus Therapeutics Ltd with regard to provision of services. E.P.P. has received support from Intuitive
Surgical. Q.S. reports a consulting or advisory role with Yiviva, Boehringer Ingelheim Pharmaceuticals, Regeneron Pharmaceuticals, Hoosier Cancer Research Network (to self), an honorarium or
speaker role with Chugai Pharmaceutical Co., stocks from Johnson & Johnson, Amgen and Merck & CO. (to self), and research funds from Celgene/BMS, Roche/Genentech, Janssen and
Novartis (to institution). D.B.S. has consulted for and received honoraria from Pfizer, Lilly/Loxo Oncology, Vividion Therapeutics, Scorpion Therapeutics and BridgeBio. M.F.B. has consulted
for Eli Lilly and PetDx, and has received research funding from Grail not related to the work presented. P.B.R. is an EMD Serono consultant and reports support for travel from Elekta and
Philips healthcare and prior research funding from EMD Serono. R.Y. has been an advisor for Pfizer, Mirati Therapeutics and Natera, and has received research support from Pfizer, Boehringer
Ingelheim and Forte Biosciences. J.J.S. has received travel support from Intuitive Surgical for fellow education and has served as a clinical advisor for Guardant Health. J.G.-A. has
received an honorarium for being a consultant with Medtronics, Ethicon, Johnson & Johnson and Intuitive Surgical, and owns stock in Intuitive Surgical. All other authors have no
competing interests. PEER REVIEW PEER REVIEW INFORMATION _Nature Medicine_ thanks the anonymous reviewers for their contribution to the peer review of this work. Primary Handling Editor:
Anna Maria Ranzoni, in collaboration with the _Nature Medicine_ team. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in
published maps and institutional affiliations. EXTENDED DATA EXTENDED DATA FIG. 1 COHORT OVERVIEW AND PATIENT BREAKDOWN BY ANALYSES. ((A) Overview of the different sample sets used for the
different analyses described in the manuscript, including sample sizes and reasons for exclusion. (B) Venn diagrams showing overlaps for patients with available MSK-IMPACT, WES, RNA-Seq and
neoadjuvant therapy (NAT) outcome data. Color bars show the distribution of different relevant clinical variables. (C-H) Same as B, but restricted to the subset of patients used in specific
analyses described in the manuscript. Thick red contours drawn on top of the Venn diagrams are used to highlight the set of patients used in each case. The G# in the titles refer to the
columns found in Supplementary Table 1. EXTENDED DATA FIG. 2 ADDITIONAL INSIGHTS INTO THE GENOMIC LANDSCAPE OF RECTAL CANCER. (A) Overview of driver alterations in rectal cancer stratified
by tumor stage. (B) Distribution of clonal versus driver mutations for the most frequently mutated genes in our rectal cancer cohort. (C) Fraction of samples with two driver mutations in
selected genes where both are clonal, both are subclonal or only one is clonal. (D) Distribution of KRAS mutations stratified by affected codon and specific amino acid change. Blue vertical
bars show the fraction of clonal versus subclonal mutations. Red and gray bars show the fraction of samples with allelic imbalance (mutant selection). (E) Distribution of mutational
signatures for samples in the WES cohort. Samples were ordered from left to right in terms of decreasing SBS1 signature (mitotic clock) and stratified according to dMMR/MSI status. EXTENDED
DATA FIG. 3 COMPARISON OF COLON AND RECTAL ADENOCARCINOMAS. (A) Clinicopathological features for right colon, left colon, and rectum samples. (B) Differences in first site of metastasis
stratified by primary tumor location. (C) Tumor mutational burden (TMB) and FGA in pMMR/MSS tumors from the right colon (n = 121), left colon (n = 187), and rectum (n = 449). Statistical
significance was assessed using a two-sided Mann–Whitney _U_-test. (D) Frequency of somatic alterations in oncogenic signaling pathways by anatomic location. Significant results were denoted
as * indicating q < 0.05, ** indicating q < 0.01, *** indicating q < 0.005, and **** indicating q < 0.001. (E) Frequency of RAS/RAF alterations in hypermutated and
non-hypermutated tumors stratified by tumor location. (F) Copy number profiles for tumors in the analyzed cohorts. (G) Frequency of copy number alterations affecting the p and q arms of
chromosome 20 by anatomic location. (H) FGA as a function of TP53 status, stratified by missense versus truncating and mono-allelic versus biallelic inactivation, for tumors from the right
colon (wild-type n = 39, missense n = 8, missense biallelic n = 33, truncating n = 1, truncating biallelic n = 17), left colon (wild-type n = 32, missense n = 10, missense biallelic n = 77,
truncating n = 5, truncating biallelic n = 29) and rectum (wild-type n = 73, missense n = 44, missense biallelic n = 175, truncating n = 12, truncating biallelic n = 81). (I) Fraction of
dMMR/MSI tumors by rectal segment. (J) Distance to the anal verge by APC status in the validation cohort of metastatic patients. APC WT (n = 43) were compared to APC altered (n = 115) using
a two-sided Mann–Whitney _U_-test, * indicates p = 0.0029. (K) Distribution of APC mutations by genomic location in tumors from the right colon, left colon, upper rectum, middle rectum, and
lower rectum. In panels (B), (D) and (G), statistical significance was assessed using a two-sided Fisher’s exact test and p values were corrected for multiple testing using false discovery
rate. In panels (C), (H) and (J), boxplots’ center lines indicate medians, edges indicate the interquartile range, and whiskers extend to the highest and lowest values not considered
outliers. EXTENDED DATA FIG. 4 CLINICAL AND GENOMIC DETERMINANTS OF RESPONSE TO NAT IN LARC. (A) Frequency of somatic alterations in rectal cancer driver genes for the patients used in our
analyses of clinical outcomes, stratified by cohort. (B) Frequency of somatic alterations in oncogenic signaling pathways for the patients used in our analyses of clinical outcomes,
stratified by cohort. (C) Left panel shows results from a multivariate analysis of associations between CR and a combination of clinicopathological and genomic features using a logistic
regression model. The error bars indicate the 95% confidence interval. Right panel shows results from a multivariate analysis of associations between DFS and a combination of
clinicopathological and genomic features using a Cox proportional hazards model. The results shown in this panel were obtained using patients treated with CRT-CNCT. (D) The left panel shows
a multivariate analysis of associations between CR and a combination of clinicopathological and genomic features using a logistic regression model. The error bars indicate the 95% confidence
interval. The right panel shows results from a multivariate analysis of associations between DFS and a combination of clinicopathological and genomic features using a Cox proportional
hazards model. The results shown in this panel were obtained using patients treated with INCT-CRT. EXTENDED DATA FIG. 5 STRATIFICATION OF RECTAL ADENOCARCINOMAS USING THE CONSENSUS MOLECULAR
SUBTYPES (CMS) CLASSIFICATION. (A) Expression levels for selected genes stratified by CMS group. Genes were annotated using the signatures from Budinska et al.70. (B) TMB stratified by CMS
groups. Sample sizes are: CMS1 (n = 11), CMS2 (n = 26), CMS3 (n = 26), and CMS4 (n = 38). (C) FGA stratified by CMS groups. Sample sizes are: CMS1 (n = 11), CMS2 (n = 26), CMS3 (n = 26), and
CMS4 (n = 38). (D) Percentage of KRAS mutated tumors by CMS group. (E) ssGSEA scores for selected pathways from the Hallmark dataset35. Sample sizes are: CMS1 (n = 11), CMS2 (n = 26), CMS3
(n = 26), and CMS4 (n = 38). (F) DFS for LARC patients treated with NAT, stratified by CMS group. (G) Levels of CA9 gene expression as a function of KRAS and PIK3CA mutational status. Double
mutants and KRAS-mutant tumors had significantly higher expression of CA9 compared to wild-type tumors, p = 1.3e-07 and p = 4.65e-05, respectively. Sample sizes are: Double-mutant (n = 8),
KRAS-mutant (n = 26), PIK3CA-mutant (n = 6), and wild-type (n = 5). Statistical significance was assessed using a two-sided Mann–Whitney _U_-test. (H) Expression of L1CAM stratified by CMS
group. L1CAM expression was higher in CMS2 and CMS4 compared to CMS3, q = 0.0498 and q = 0.096, respectively. Sample sizes are: CMS1 (n = 11), CMS2 (n = 26), CMS3 (n = 26), and CMS4 (n =
38). (I) Validation of transcriptomic findings using an independent cohort of 15 LARC cases from Kamran et al.10 Differential gene expression was conducted using DESeq2 and the p-values
attained by the Wald test were corrected using false discovery rates. In panels (B), (C), (E) and (H), statistical significance was assessed using a two-sided Mann–Whitney _U_-test. P values
were corrected using the Bonferroni method and significant results are denoted as *q < 0.05, **q < 0.01, ***q < 0.005 and ****q < 0.001. In panels (B), (C), (E), (G), and (H),
boxplots’ center lines indicate medians, edges indicate the interquartile range, and the whiskers extend to the highest and lowest values not considered outliers. EXTENDED DATA FIG. 6
SUPPORTING INFORMATION FOR THE CHARACTERIZATION OF IMMUNE HOT PMMR/MSS LARC TUMORS WITH FAVORABLE OUTCOMES FROM NAT. (A) Quantification of intra-tumoral TILs from H&E slides for 20
patients, including cases from IG1 (n = 6), IG2 (n = 6), IG3 (n = 5) and IG4 (n = 3). Statistical significance was assessed using a two-sided Mann–Whitney _U_-test. P values were corrected
using the Bonferroni method. Boxplots’ center lines indicate medians, edges indicate the interquartile range, and the whiskers extend to the highest and lowest values not considered
outliers. Right panel shows correlation between estimated fractions of intra-tumoral and inter-tumoral TILs. Statistical significance was assessed using a two-sided Spearman correlation.
Error bands represent 95% confidence intervals. (B) ssGSEA scores for immune cell signatures from Bindea et al.32. Displayed cell types are the ones with an adjusted p-value < 0.10 after
Bonferroni correction, based on a Kruskal-Wallis test. (C) Comparison of ssGSEA scores for specific oncogenic pathway signatures from the Hallmark set35 across the four immune clusters.
Displayed cell types are the ones with an adjusted p-value < 0.10 after Bonferroni correction, based on a Kruskal-Wallis test. In panels (B) and (C), sample sizes are: IG1 (n = 52), IG2
(n = 37), IG3 (n = 7), and IG4 (n = 5). (D) Correlation plot showing gene signatures for 27 selected oncogenic pathways (yellow diamonds) and immune cell infiltrates (green diamonds). Right
panels show illustrative scatter plots for pairs of variables with strong positive and negative correlations. White dots in the correlation heatmap highlight pairs of variables with
significant two-sided Spearman correlation after Bonferroni correction. Error bands represent 95% confidence intervals. In panels (B) and (C), statistical significance was assessed using a
two-sided Mann–Whitney _U_-test. P values were corrected using the Bonferroni method and significant results are denoted as *q < 0.05, **q < 0.01, ***q < 0.005 and ****q < 0.001.
Boxplots’ center lines indicate medians, edges indicate the interquartile range, and the whiskers extend to the highest and lowest values not considered outliers. EXTENDED DATA FIG. 7
VALIDATION OF IMMUNE GROUPS IN AN INDEPENDENT COHORT OF LARC TUMORS FROM TCGA. Validation of results using an independent cohort of 42 LARC samples from TCGA. (A) Unsupervised hierarchical
clustering of pMMR/MSS tumors using ssGSEA scores for a set of well established immune signatures reveals three groups with increasing levels of overall immune infiltrate (IG1–IG3). dMMR/MSI
tumors were added later as a fourth group (IG4). (B) Tumors in IG4 had higher TMB and had lower FGA than tumors in the IG1–IG3 groups. Sample sizes for each group are as follows: IG1 (n =
16), IG2 (n = 17), IG3 (n = 7), and IG4 (n = 2). Boxplots’ center lines indicate medians, edges indicate the interquartile range, and the whiskers extend to the highest and lowest values not
considered outliers. (C) Distribution of CMS classes across immune groups. (D) Selected significant differences in ssGSEA scores for specific immune cell types across immune groups. Sample
sizes for each group are as follows: IG1 (n = 16), IG2 (n = 17), IG3 (n = 7), and IG4 (n = 2). (E) Comparison of expression levels for genes encoding proteins involved in immune checkpoint
blockade. Sample sizes for each group are as follows: IG1 (n = 16), IG2 (n = 17), IG3 (n = 7), and IG4 (n = 2). In panels (D) and (E), statistical significance was assessed using a two-sided
Mann–Whitney _U_-test. P values were corrected using the Bonferroni method and significant results are denoted as *q < 0.05, **q < 0.01, ***q < 0.005 and ****q < 0.001.
Boxplots’ center lines indicate medians, edges indicate the interquartile range, and the whiskers extend to the highest and lowest values not considered outliers. SUPPLEMENTARY INFORMATION
REPORTING SUMMARY SUPPLEMENTARY TABLES Supplementary Tables 1–11: Table S1, Clinical, histopathological, and sequencing data; Table S2: Summary of clinical characteristics for the full
cohort. Table S3: Overview of cohorts and key clinicopathological features. Table S4: Summary of MutSigCV analysis using WES samples. Table S5: Sample identifiers and clinical information
for cases in supplemental cohorts. Table S6: Summary of clinical characteristics for the treatment response cohort. Table S7: Summary of outcome analysis (response and DFS) using genomic
data. Table S8: Summary of outcome analysis (response and DFS) using transcriptomic data. . Table S9: Results from TIL quantification analyses. Table S10: Validation of immune profiling
results using data from TCGA. Table S11: List of genes on the MSK-IMPACT targeted sequencing panels. RIGHTS AND PERMISSIONS Springer Nature or its licensor holds exclusive rights to this
article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of
such publishing agreement and applicable law. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Chatila, W.K., Kim, J.K., Walch, H. _et al._ Genomic and transcriptomic
determinants of response to neoadjuvant therapy in rectal cancer. _Nat Med_ 28, 1646–1655 (2022). https://doi.org/10.1038/s41591-022-01930-z Download citation * Received: 24 September 2021 *
Accepted: 29 June 2022 * Published: 15 August 2022 * Issue Date: August 2022 * DOI: https://doi.org/10.1038/s41591-022-01930-z SHARE THIS ARTICLE Anyone you share the following link with
will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt
content-sharing initiative
