High cd3 and icos and low tim-3 expression predict favourable survival in resected oesophageal squamous cell carcinoma
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT With the increasing oncological potential of immunotherapy, several immune checkpoint modulators are being investigated. The value of immune markers, including programmed cell death
ligand-1, programmed cell death-1 (PD-1), inducible co-stimulator (ICOS), lymphocyte activation gene-3, T-cell immunoglobulin, and mucin-dominant containing-3 (TIM-3), is not well known.
Using tissue microarrays of 396 patients who underwent surgery for oesophageal squamous cell carcinoma (ESCC), infiltrated T-cell subsets (CD3, CD8, and Foxp3) and checkpoint protein
expression were scored. With a median follow-up of 24.8 months, CD3+ TIL subsets (50.0%) had longer median recurrence-free survival (RFS, 55.0 vs 21.4 months) and overall survival (OS, 77.7
vs 35.8 months). Patients with high ICOS expression (46.5%) had longer median RFS (53.9 vs 25.3 months) and OS (88.8 vs 36.9 months). For PD-1, RFS (hazard ratio [HR] 0.67) and OS (HR 0.66)
were significantly longer in the high-expression group (45.2%). In the multivariate analysis, high TIM-3 expression (50.8%) had a significant relationship with shorter RFS (HR = 1.52) and OS
(HR = 1.60). High CD3+ TIL and T-cell ICOS expression were associated with favourable prognosis, whereas high TIM-3 expression suggested a poor prognosis. Our findings may confer new
insights to improve ESCC outcomes beyond the application of PD-1 blockade. SIMILAR CONTENT BEING VIEWED BY OTHERS CLINICAL EFFICACY AND IMMUNE RESPONSE OF NEOADJUVANT CAMRELIZUMAB PLUS
CHEMOTHERAPY IN RESECTABLE LOCALLY ADVANCED OESOPHAGEAL SQUAMOUS CELL CARCINOMA: A PHASE 2 TRIAL Article Open access 20 August 2024 INTEGRATIVE IMMUNE TRANSCRIPTOMIC CLASSIFICATION IMPROVES
PATIENT SELECTION FOR PRECISION IMMUNOTHERAPY IN ADVANCED GASTRO-OESOPHAGEAL ADENOCARCINOMA Article Open access 17 October 2022 PROGNOSTIC FACTORS OF RESECTED PATHOLOGICAL STAGE I LUNG
ADENOCARCINOMA: EVALUATING SUBTYPES AND PD-L1/CD155 EXPRESSION Article Open access 07 December 2023 INTRODUCTION Oesophageal cancer is the sixth leading cause of global cancer-related
death1. Despite developments in surgical and radiation techniques and chemotherapeutic agents, the prognosis of advanced oesophageal squamous cell carcinoma (ESCC) is generally poor, with a
<35% 5-year survival rate2. There are two types of oesophageal cancer: ESCC and oesophageal adenocarcinoma. In Eastern Asia, >90% of oesophageal cancer cases are ESCC, with growing
recognition that ESCC and oesophageal adenocarcinoma have distinct phenotypes, aetiologies, and pathogeneses3. The seventh and upcoming eighth edition cancer staging systems of the American
Joint Committee on Cancer (AJCC) assign separate guidelines for staging these two cancer types4. Immune escape occurs when cancer cells evade the host immune system. The interaction between
programmed cell death ligand-1 (PD-L1) and programmed cell death protein-1 (PD-1) is a common and important immune-evading mechanism in many cancer types and blocking this interaction has
emerged as a breakthrough in cancer therapy5. Since late 2016, PD-1 inhibitors have been approved for melanoma, non-small cell lung cancer, renal cell carcinoma, and head and neck cancer by
the U.S. Food and Drug Administration; compared with old cytotoxic agents, PD-1 inhibitors have superior efficacy with an improved safety profile in various tumour types6. These checkpoint
inhibitors have been adapted to daily clinical practice, dramatically changing malignant tumour treatment. Clinical trials with pembrolizumab and nivolumab are ongoing and include almost
every tumour type from solid tumours to haematologic malignancies and from neoadjuvant and adjuvant to the palliative setting7. Besides the PD-1/PD-L1 pathway, agents modulating other
checkpoints, including inducible co-stimulator (ICOS), lymphocyte activation gene-3 (LAG-3), T-cell immunoglobulin and mucin-dominant containing-3 (TIM-3), and T-cell immunoreceptor with Ig
and ITIM domains (TIGIT), are actively under development8,9,10. With PD-1/PD-L1 blockade as a backbone, combination approaches with these immune checkpoint modulators appear promising; this
strategy may help overcome resistance to PD-1/PD-L1 inhibitors. Despite this approach, studies evaluating the prognostic and predictive impacts in each cancer type have produced inconsistent
results11,12. The roles of PD-1, PD-L1, and other immune checkpoints in various cancer types remain unknown. Moreover, the clinical implications of various immune receptors in ESCC,
including PD-1, PD-L1, LAG-3, TIM-3, and TIGIT, remain undefined. Here, we investigated the distribution and frequency of CD3+/CD8+ T-cells, regulatory T-cells, and other immune checkpoints,
including PD-L1, PD-1, ICOS, LAG-3, and TIM-3, in surgically resected ESCC and also determined their prognostic value in identifying potential therapeutic targets. RESULTS BASELINE
CHARACTERISTICS Overall, 407 patients who underwent surgical resection for ESCC were identified. Eleven cases were excluded due to incomplete staining, and 396 eligible ESCC tumour samples
were assessed. They were evaluated for PD-L1 expression (on both tumour and immune cells) and CD3, CD8, Foxp3, ICOS, LAG-3, and TIM-3 expression (Supplementary Fig. 1). Table 1 shows the
patients’ baseline characteristics. The median age was 64 years (range: 41–83 years); most patients were male (93.4%) and were current or former smokers (73.5%). The percentages of patients
in stage I, II, III, and IV at surgery were 21.2%, 45.7%, 30.0%, and 3.0%, respectively. None of the patients received neoadjuvant treatment. During the median follow-up period of 24.8
(range 0.5–210) months, 129 (32.6%) patients experienced recurrence, and 181 (45.7%) deaths occurred. The 5-year overall survival (OS) rate was 44.9% in the total population. PROGNOSTIC
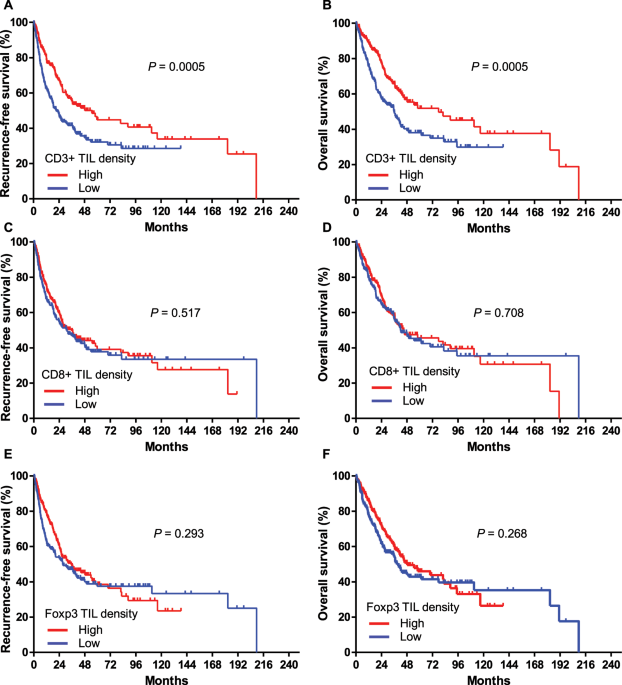
IMPACT OF CD3+, CD8+, AND FOXP3+ T-CELL LYMPHOCYTE DENSITY Patients were grouped into low- and high-frequency groups based on tumour-infiltrating lymphocytes (TILs) according to a median
value of 252/4HPFs for CD3+ TILs, 96/4HPFs for CD8+ TILs, and 0/4HPFs for Foxp3+ TILs. The association between the frequency of CD3+, CD8+, and Foxp3+ T-cell lymphocytes and the
clinicopathological characteristics of patients are shown in Supplementary Tables 1–3, respectively. High densities of both CD3+ TIL and FoxP3 + TIL were associated with high pathologic T
and TNM stage (Supplementary Tables 1 and 3). The high-frequency CD3+ TILs group (n = 198, 50.0%) had a significant longer RFS (hazard ratio [HR] = 0.61, 95% confidence interval [CI]:
0.46–0.81, _P_ = 0.0005) and OS (HR = 0.59, 95% CI: 0.44–0.80, _P_ = 0.0005) than the low frequency CD3+ TILs group (Fig. 1A,B). The high- and low-frequency CD3+ TILs groups had medians of
55.0 and 21.4 months for RFS and medians of 77.7 and 35.8 months for OS, respectively. After adjusting for age, sex, smoking status, and various T-cell marker expression levels, multivariate
analysis demonstrated a low risk of disease relapse (HR = 0.57, 95% CI: 0.41–0.78, _P_ < 0.001) and death (HR = 0.52, 95% CI: 0.37–0.74, _P_ < 0.001) in the high-frequency CD3+ TILs
group (Tables 2 and 3). However, there was no prognostic association between the density of CD8+ TILs or Foxp3+ TILs and RFS or OS (Fig. 1C–F). PROGNOSTIC IMPLICATION OF ICOS, LAG-3, PD-1,
AND TIM-3 EXPRESSION IN IMMUNE CELLS We investigated the expression of immune receptors (ICOS, LAG-3, PD-1, and TIM-3) in immune cells. The median values of ICOS, LAG-3, and PD-1 expression
in immune cells were 0/4HPFs, 22/4HPFs, and 0/4HPFs, respectively. Given the abundance of TIM-3 expression, the proportion of TIM-3-positive immune cells was not numbered as the cell
count/HPF but scored as the percentage of stained cells in the total immune cells. Because the median percentage of TIM-3 expression was 0%, TIM-3 expression of ≥1% was defined as high
density. The association between the expression of ICOS, LAG-3, PD-1, and TIM-3 and clinicopathological characteristics of patients are shown in Supplementary Tables 4–7, respectively.
Fisher’s exact test indicated that low ICOS expression was associated with smoking. Additionally, low pathologic T and pathologic TNM stage was related to high LAG-3 expression. There was no
significant association between PD-1 expression and the clinical characteristics. In the survival analysis of these markers, patients with high ICOS expression (n = 184, 46.5%) demonstrated
a significantly longer RFS (HR = 0.72, 95% CI: 0.55–0.95, _P = _0.021) and OS (HR = 0.67, 95% CI: 0.50–0.89, _P = _0.007) compared to that in patients with low ICOS expression (Fig. 2A,B).
The high and low ICOS groups had medians of 53.9 and 25.3 months, respectively, for RFS and medians of 88.8 and 36.9 months, respectively, for OS. Similar results were observed in uni- and
multivariate Cox analyses comparing high vs low ICOS expression (Tables 2 and 3; HR = 0.67, 95% CI: 0.50–0.89, _P_ = 0.007 for recurrence; and HR = 0.61, 95% CI: 0.45–0.85, _P_ = 0.003 for
survival, all in multivariate analysis). LAG-3 expression was not associated with RFS and OS duration in either Kaplan-Meier or uni- and multivariate analyses (Fig. 2C,D, and Table 2).
Regarding PD-1 expression, RFS (HR = 0.67, 95% CI: 0.50–0.88, _P_ = 0.004) and OS (HR = 0.66, 95% CI: 0.49–0.88, _P_ = 0.006) were significantly better in the high-expression group (n = 179)
than in the low-expression group (n = 217) (Fig. 2E,F). While there was a trend toward better survival in patients with high PD-1 expression, Cox regression analysis indicated that
associations between survival and PD-1 expression were non-significant (Tables 2 and 3). TIM-3 expression had no prognostic value for RFS and OS in the Kaplan-Meier analysis (Fig. 2G,H).
However, in the uni- and multivariate analyses using Cox regression, high TIM-3 expression (n = 201, 50.8%) was associated with a higher probability of recurrence (HR = 1.52, 95% CI:
1.10–2.10, _P_ = 0.011 in multivariate analysis) and death (HR = 1.60, 95% CI: 1.13–2.27, _P_ = 0.008 in multivariate analysis) (Tables 2 and 3). To refer our finding to an independent
patient cohort, we applied gene expression to The Cancer Genome Atlas (TCGA) ESCC samples regarding TIM-3 (n = 85, Supplementary Fig. 2). At first, mRNA expression data of hepatitis A virus
cellular receptor 2 (_HAVCR2_) gene, which encodes the TIM-3 protein in ESCC, were obtained from the Genomic Data Commons Data Portal (CDC) in TCGA and OncoLnc. OncoLnc is a resource to link
TCGA survival data to mRNA, miRNA, or lncRNA expression (available at http://www.oncolnc.org)13,14. There was no difference in OS between the high and low _HAVCR2_ mRNA expressions (median
OS, 42.1 and 18.9 months, respectively, HR = 0.67, 95% CI 0.3–1.48, _P_ = 0.32). PD-L1 IMMUNOHISTOCHEMISTRY Among 396 patients, 101 (25.5%), 89 (22.5%), 60 (15.7%), 33 (8.3%), and 14 (3.5%)
had positive IHC staining of PD-L1 in ≥1%, ≥5%, ≥10%, ≥25%, and ≥50% of tumour cells, respectively. For immune cells, 189 (47.7%), 141 (35.6%), 97 (24.4%), 44 (11.1%), and 21 (5.3%) patients
had ≥1%, ≥5%, ≥10%, ≥25%, and ≥50% of cells showing PD-L1 IHC staining, respectively. Seventy-four percent of tumour cells and 52% of immune cells did not express PD-L1 (Supplementary Fig.
3). With a 5% cut-off point, no significant correlation was observed between T-cell frequency and age, sex, tumour location, smoking status, and TNM stage. However, higher PD-L1 expression
in tumour cells was related to a higher N stage (Supplementary Tables 8 and 9). PROGNOSTIC IMPACT OF PD-L1 EXPRESSION ON TUMOUR AND IMMUNE CELLS PD-L1 expression on tumour and immune cells
with various cut-offs (1%, 5%, 10%, 25%, and 50%) were evaluated among 396 samples and analysed in relation to the survival data (Fig. 3). The median PD-L1 expression rate was 0% in both
tumour and immune cells, while the corresponding means were 5.6% and 8.0%, respectively. Even after incorporating various cut-off points in tumour and immune cells, our data indicated no
significant correlation between PD-L1 expression and RFS and OS. Multivariate Cox analysis showed similar results (Tables 2 and 3). Median RFS and OS of patients with PD-L1 expression in
≥50% immune cells (n = 21, 5.3%) were numerically greater than those in patients with PD-L1 expression in <50% of cells (median RFS: 111.1 vs 30.7 months, _P_ = 0.355, median OS: 111.1 vs
42.3 months, _P_ = 0.367). However, this difference was not statistically significant. RELATIONSHIPS AMONG EXPRESSION OF VARIOUS IMMUNE MARKERS Overall, the median expression levels of
FoxP3, ICOS, PD-1, and PD-L1 were 0, and any expression from these markers was considered as a “higher expression”. Moreover, the expression of one immune marker has close associations with
other markers (Supplementary Table 10). After performing Spearman’s rank correlation analysis, CD8+ TIL expression was related with LAG-3, PD-1, TIM-3, and PD-L1 expression in immune cells
(_P_ < 0.001, respectively). Two immune markers, CD3 and ICOS, that displayed a prognostic role in this study were linked (_r_ = 0.128, _P_ = 0.011). However, no significant association
was present between CD8 and ICOS expression or between ICOS and LAG-3 expression. COMBINATION OF CD3+ TIL WITH ICOS, PD-1, AND TIM-3 EXPRESSION We classified ESCC subjects into four
subgroups based on CD3+ TIL positivity and ICOS expression, and the same method was applied for CD3 with PD-1 and CD3 with TIM-3, as these were proposed to have a prognostic impact in the
current analysis. The Kaplan-Meier analysis revealed significant differences in RFS among these four types in each subgroup (Supplementary Fig. 4). Consistent with the strong prognostic
characteristics of ICOS and PD-1, CD3+ subgroups with positive ICOS or PD-1 expression showed the longest RFS (median: 88.8 and 58.0 months, respectively) compared with subgroups that were
CD3+/ICOS- or CD3+/PD-1- (median: 18.6 and 17.6 months, respectively). Furthermore, consistent with the poor prognostic profile of TIM-3, subgroups that were CD3+/TIM-3− demonstrated the
longest RFS (median: 59.7 vs 3.5 months in CD3−/TIM-3−). However, these correlations with RFS did not translate into OS. DISCUSSION ESCC is one of the most aggressive cancers. Definitive
surgical therapy, including oesophagectomy, is considered a standard treatment for resectable diseases; however, >50% of patients undergo local recurrence and/or distant metastasis15,16.
Even with recent improvements in sequencing techniques and precision medicine, molecularly targeted therapy has a limited role. Furthermore, traditional cytotoxic agents have not
demonstrated progress in the last decade. Therefore, ESCC prognosis is dismal, with a high unmet need. In other cancer types such as lung cancer, immune checkpoint inhibitors, represented by
PD-1/PD-L1 blockade, have recently shown promising efficacy in treating advanced/metastatic ESCC17,18. In a clinical trial, the objective response rate of 17% and a median OS of 10.8 months
appear to be encouraging considering the heavily treated characteristics in the study population18. Despite the impressive outcomes of PD-1/PD-L1 inhibitory cancer immunotherapy, efficacy
is suboptimal, and most patients with many tumour types do not show a response19. Thus, the focus has shifted to targeting alternative immune checkpoints receptors. Combining two or more
anti-tumour drugs for improving cancer treatment is not a new concept in oncology, and it is also valid in the immuno-oncology era20. Combination therapy involving PD-1/PD-L1 inhibitors with
other immune checkpoint modulators has been considered an important strategy to overcome primary and secondary resistances to PD-1/PD-L1 blockade21. Several immune modulators are being
investigated in pre-clinical models and clinical trials; however, our understanding of these checkpoints is incomplete, especially in ESCC. Furthermore, the expression level cut-offs,
associations with clinicopathological features, and prognostic impact of these various checkpoints have not been established for ESCC. The PD-L1 expression level has a critical role in
T-cell regulation, but the precise significance varies among studies and cancer types22. We comprehensively investigated the prognostic impact of immune cell infiltration and various immune
checkpoints, including PD-L1, PD-1, ICOS, LAG-3, and TIM-3, in resected ESCC. Additionally, the significance of clinical factors such as sex, age, smoking status, and TNM stage was explored.
The most significant prognostic factor was the TNM stage (Table 2 and Supplementary Fig. 5). Given that the number of stage IV subjects was small, it may not have a significant impact on OS
and mitigate the influence of immune markers. Several studies report that TILs have a positive prognostic effect across various cancer types23,24,25. TILs have an important role in
anticancer immune responses and the cancer immunity cycle26. However, TILs are divided into several subgroups based on cell surface antigen expression. Each subset has a distinct interactive
function between the tumour and tumour microenvironments and sometimes the roles differ across cancer types27. CD3 is a transmembrane protein that is exclusively expressed in the T-cell
pedigree and thus is considered to represent a mature T-cell marker and whole tumour-infiltrating T-cells28. CD8 T-cells generally represent cytotoxic T-cells, and Foxp3 is the distinct
transcription marker of regulatory T-cells29. Among different lymphocyte types, CD3-positive TILs are most significantly associated with survival across various tumours27. Consistent with
previous literature on total TILs or stromal TILs in ESCC, in the present ESCC study, high CD3+ TIL density showed good prognostic impact, whereas CD8+ TILs and Foxp3+ TILs did not30,31,32.
We attempted to investigate stromal and intra-tumoural CD3+ or CD8+ TILs independently; however, TIL abundance made it unfeasible. One meta-analysis showed that CD8+ TILs were associated
with good prognosis; however, it included a heterogeneous population of patients with oesophageal adenocarcinoma and squamous cell carcinoma33. To our knowledge, we are the first to report
ICOS, LAG-3, and TIM-3 expressions and their clinical implication in a large ESCC cohort. As expected, ICOS, LAG-3, and TIM-3 expressions were related to PD-1 expression on TILs, possibly
indicating the feedback nature of the immune system (Supplementary Table 10). ICOS is a surface antigen in T-cells, and its expression is low in naïve T-cells. Once ICOS is stimulated by
both the T-cell receptor and CD28 signals, it is upregulated in activated T-cells34. Co-stimulation by ICOS and ICOS ligand confers an anticancer response, but ICOS signalling also engages
regulatory T-cell activity induction35. Thus, ICOS might have a dual role in oncogenesis. The prognostic impact of ICOS expression is inconsistent across various tumour types (e.g.,
melanoma, colorectal cancer, breast cancer, gastric cancer, and renal cell carcinoma), and these clinical findings support the dual role of ICOS in carcinogenesis8. In our study, high ICOS
expression in immune cells was significantly associated with longer RFS and OS in the Kaplan-Meier method and multivariate Cox regression model (Fig. 2 and Table 2). Our findings suggest
that ICOS-expressing immune cells include tumour neoantigen-specific T-cells and are associated with favourable prognosis, at least in ESCC. However, this should be validated in an
independent patient cohort and in clinical trials with ICOS-targeted therapies. Despite the existence of several LAG-3-related studies, data regarding the prognostic impact of LAG-3 in most
cancer types are limited9. Two reports on NSCLC have contradictory results36,37. Moreover, one exploratory study showed that LAG-3 expression was associated with good prognosis in resected
ESCC; however, this is inconsistent with the current data38. Accordingly, the role of LAG-3 in cancer and ESCC in particular remains elusive. As a marker of CD8+ T-cell dysfunction or
exhaustion, TIM-3 is occasionally co-expressed with PD-1 in CD8+ T-cells in several tumours19. Moreover, TIM-3 is expressed in natural killer cells, regulatory T-cells, dendritic cells,
B-cells, macrophages, and other myeloid cells. TIM-3 expression inhibited anti-tumour immunity by T-cell exhaustion, suppressed immune response from the status of innate immunity, and
exhibited pro-tumour activity by promoting myeloid-derived suppressor cells9. Consistent with the previously known immune regulatory role of TIM-3 in oncogenesis, TIM-3 expression is
associated with poor prognosis in several cancers39,40. The high probability of recurrence or death was also related to high TIM-3 expression in the present study, which is the first to
report the prognostic impact of TIM-3 in ESCC. In several preclinical studies, blocking TIM-3 enhanced cancer immunity by T-cell proliferation and cytokine production, as well as combination
with PD-1 blockade, also demonstrated a remarkable synergy in these models10. Additionally, many clinical trials focusing on targeting TIM-3 are ongoing globally41. One important issue
regarding blocking TIM-3 might be related to their expression levels in various tumour-infiltrating immune cells. Most patients (92%, 364/396, data not shown) in the present study expressed
TIM-3 in T-cells. Thus, based on the high frequency of TIM-3 expression and its demonstrated poor prognostic value, TIM-3 may be a potential target candidate in ESCC. In conjunction with the
current role of PD-1 blocking agents in ESCC, the use of TIM-3-targeted therapy in combination with PD-1 blockade may be a promising strategy. Although more studies are needed, our study
may provide some evidence supporting the approach to target TIM-3 in ESCC. Together with advances in PD-1/PD-L1 blockade, the relationship of PD-1/PD-L1 expression and its prognostic impact
in various tumour types are gaining increased attention. Although the Kaplan-Meier method revealed that high PD-1 expression in TILs was associated with better RFS and OS, in Cox regression
analyses, patients with high PD-1 expression had increased risk of relapse and death compared with those with low PD-1 expression. Considering the high association with PD-1 and other immune
checkpoints, the overlap and diverse interaction between various immune checkpoints may attenuate the prognostic impact of PD-1 in ESCC (Supplementary Table 10). Regarding PD-L1, 25.5%
(101/396) of patients showed PD-L1 expression in ≥1% of tumour cells and in 47.7% (189/396) of immune cells (Supplementary Fig. 3). We used various cut-offs of PD-L1 expression in tumour or
immune cells to determine associations with prognosis, but we did not identify any meaningful associations with recurrence or survival. Because blocking PD-1/PD-L1 has gained much attention,
several studies have investigated the prognostic role of PD-L1 expression in ESCC. However, these studies presented inconsistent results30. Some studies reported that PD-L1 expression was
associated with poor prognosis, but another study indicated it was not associated with poor prognosis. A meta-analysis showed a positive but statistically non-significant trend in prognosis
with PD-L1 expression42. In our study, there were no clinically significant relationships between survival and PD-L1 expression in tumour or immune cells. These conflicting results might
derive from differences in the patient population, staining method and antibodies, and definition of PD-L1 positivity. Thus, heterogeneity in the prognostic role of PD-L1 has been observed
in several cancer types. Our study has some limitations. First, it was retrospective in nature. Second, it did not include the localisation information of each marker and therefore did not
provide data on the spatial distribution of immune cells. Furthermore, since most patients underwent oesophagectomy when the neoadjuvant concurrent chemoradiation data was published and
incorporated into clinical practice, none of the patients received preoperative treatment43. Additionally, no patient underwent immunotherapy; thus, this study did not provide any data
regarding the response to immune checkpoint modulators. In conclusion, we demonstrated that a high frequency of CD3+ TILs and high ICOS expression on immune cells are related to a favourable
prognosis in ESCC. Furthermore, TIM-3 expression in immune cells was associated with poor prognosis in uni- and multivariate analyses. Our findings may help improve ESCC outcomes beyond the
application of PD-1 blockade. These discoveries have important implications for using antibody therapies in addition to the PD-1/PD-L1 signalling pathway, such as TIM-3, in ESCC. METHODS
PATIENTS AND TISSUE SAMPLES The study population comprised ESCC patients who underwent radical surgical resection at Severance Hospital and Samsung Medical Center, Seoul, Korea between 1996
and 2012. The inclusion criteria were (1) surgically resected ESCC with a curative aim and (2) availability of tumour tissue. Clinicopathologic data were collected and reviewed. Tumours were
re-classified based on the 7th edition of the AJCC TNM cancer staging system. Twelve subjects underwent oesophagectomy and were subsequently identified as having stage IV. The study was
approved by the Institutional Review Board (IRB) of Severance Hospital and was conducted according to the ethical principles, guidelines, and relevant regulations. The IRB approved our
research, and as the study was a retrospective review of subjects, the requirement for informed consent was waived. TISSUE MICROARRAY PREPARATION AND IHC ESCC specimens were histologically
reviewed by two experienced pathologists (Y.C. and S.S.). Haematoxylin- and eosin-stained sections from formalin-fixed paraffin-embedded tissues were reviewed to identify the invasive
carcinoma area. The most densely viable carcinoma areas were chosen as the representative areas (core – 3.0 mm). Tissue microarrays were constructed from these samples and assessed by
immunohistochemical staining for PD-L1, PD-1, CD3, CD8, Foxp3 (forkhead box P3), ICOS, TIM-3, and LAG-3. The following primary antibodies were used: PD-L1 (dilution 1:100; clone SP142;
Ventana), PD-1 (dilution 1:100; clone NAT105; Cell Marque, Rocklin, CA, USA), CD3 (dilution 1:200; LabVision, Fremont, CA, USA), CD8 (RTU; clone C8/144B; Dako, Glostrup, Denmark), Foxp3
(dilution 1:100; Abcam, Cambridge, UK), ICOS (clone SP98; dilution 1:50; Thermo Scientific, Rockford, IL, USA), TIM-3 (dilution 1:200; clone D5D5RTM; Cell Signaling), and LAG-3 (clone
EPR4392(2); dilution 1:100; Abcam). The staining protocols were the same as published previously44. IHC SCORING Two well-experienced pathologists manually scored each IHC in the tissue
microarray samples. PD-L1 expression on tumour and immune cells was analysed separately. Tumour cells showing any intensity of membranous and/or cytoplasmic staining were defined as having
positive staining, and the proportion of PD-L1-positive tumour cells was estimated as the percentage of total tumour cells in the whole section. The pre-specified cut-off values at 1%, 5%,
10%, 10%, 25%, and 50% were established. The same method was applied to assess PD-L1 expression in immune cells. The expression was defined as high density for CD3, CD8, ICOS, Foxp3, LAG-3,
and PD-1 when the expression level was above the median value per four high-power fields (4HPFs). STATISTICAL ANALYSIS We investigated the association between various immune markers and
clinical data using the chi-squared test or Fisher’s exact test. Survival was analysed by the Kaplan-Meier method with log-rank for categorical variables. Uni- and multivariate analyses for
predicting recurrence and survival were performed using the Cox regression method for the following variables: age, sex, smoking status, stage, histology, location, and each immune marker
status. RFS was defined from the time of surgery to initial relapse or death. OS was defined as the time from the surgery until death from any cause or the most recent follow-up. The cases
for OS included cases that were still alive and cases whose causes of death were not related to oesophageal cancer. Living patients were censored at the time of the last follow-up.
Spearman’s rank correlation test was used to assess the relationship among various immune markers. All statistical analyses were performed using SPSS version 23.0 (SPSS, Chicago, IL). _P_
< 0.05 was considered statistically significant by the Kaplan-Meier method. DATA AVAILABILITY As per institutional policy, the datasets generated and analysed during the current study are
publicly unavailable; however, they are available from the corresponding author upon reasonable request. REFERENCES * Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015.
_CA: a cancer journal for clinicians_ 65, 5–29 (2015). Google Scholar * Chen, G., Wang, Z., Liu, X. Y. & Liu, F. Y. Recurrence pattern of squamous cell carcinoma in the middle thoracic
esophagus after modified Ivor-Lewis esophagectomy. _World journal of surgery_ 31, 1107–1114 (2007). PubMed Google Scholar * Xu, G. _et al_. Prognosis and Progression of ESCC Patients with
Perineural Invasion. _Scientific reports_ 7, 43828 (2017). Article ADS PubMed PubMed Central Google Scholar * Rice, T. W., Ishwaran, H., Ferguson, M. K., Blackstone, E. H. &
Goldstraw, P. Cancer of the Esophagus and Esophagogastric Junction: An Eighth Edition Staging Primer. _Journal of thoracic oncology: official publication of the International Association for
the Study of Lung Cancer_ 12, 36–42 (2017). Article Google Scholar * Ni, L. & Dong, C. New checkpoints in cancer immunotherapy. _Immunological reviews_ 276, 52–65 (2017). Article CAS
PubMed Google Scholar * Chiavenna, S. M., Jaworski, J. P. & Vendrell, A. State of the art in anti-cancer mAbs. _Journal of biomedical science_ 24, 15 (2017). Article CAS PubMed
PubMed Central Google Scholar * Gong, J., Chehrazi-Raffle, A., Reddi, S. & Salgia, R. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review
of registration trials and future considerations. _Journal for immunotherapy of cancer_ 6, 8 (2018). Article PubMed PubMed Central Google Scholar * Amatore, F., Gorvel, L. & Olive,
D. Inducible Co-Stimulator (ICOS) as a potential therapeutic target for anti-cancer therapy. _Expert opinion on therapeutic targets_ 22, 343–351 (2018). Article CAS PubMed Google Scholar
* Anderson, A. C., Joller, N. & Kuchroo, V. K. Lag-3, Tim-3, and TIGIT: Co-inhibitory Receptors with Specialized Functions in Immune Regulation. _Immunity_ 44, 989–1004 (2016). Article
CAS PubMed PubMed Central Google Scholar * Anderson, A. C. Tim-3: an emerging target in the cancer immunotherapy landscape. _Cancer immunology research_ 2, 393–398 (2014). Article CAS
PubMed Google Scholar * Hu-Lieskovan, S. & Ribas, A. New Combination Strategies Using Programmed Cell Death 1/Programmed Cell Death Ligand 1 Checkpoint Inhibitors as a Backbone.
_Cancer journal (Sudbury, Mass.)_ 23, 10–22 (2017). Article CAS Google Scholar * Day, D. _et al_. From Famine to Feast: Developing Early-Phase Combination Immunotherapy Trials Wisely.
_Clinical cancer research : an official journal of the American Association for Cancer Research_ 23, 4980–4991 (2017). Article Google Scholar * Cancer Genome Atlas Research, N. _et al_.
Integrated genomic characterization of oesophageal carcinoma. _Nature_ 541, 169–175 (2017). Article CAS Google Scholar * Anaya, J. OncoLnc: linking TCGA survival data to mRNAs, miRNAs,
and lncRNAs. _Peerj Computer Science_ 2, e67 (2016). Article Google Scholar * Smit, J. K. _et al_. Prognostic factors and patterns of recurrence in esophageal cancer assert arguments for
extended two-field transthoracic esophagectomy. _American journal of surgery_ 200, 446–453 (2010). Article PubMed Google Scholar * Doki, Y. _et al_. Association of the primary tumor
location with the site of tumor recurrence after curative resection of thoracic esophageal carcinoma. _World journal of surgery_ 29, 700–707 (2005). Article PubMed Google Scholar * Doi,
T. _et al_. Safety and Antitumor Activity of the Anti-Programmed Death-1 Antibody Pembrolizumab in Patients With Advanced Esophageal Carcinoma. _Journal of clinical oncology: official
journal of the American Society of Clinical Oncology_ 36, 61–67 (2018). Article CAS Google Scholar * Kudo, T. _et al_. Nivolumab treatment for oesophageal squamous-cell carcinoma: an
open-label, multicentre, phase 2 trial. _The Lancet. Oncology_ 18, 631–639 (2017). Article CAS PubMed Google Scholar * Ott, P. A., Hodi, F. S., Kaufman, H. L., Wigginton, J. M. &
Wolchok, J. D. Combination immunotherapy: a road map. _Journal for immunotherapy of cancer_ 5, 16 (2017). Article PubMed PubMed Central Google Scholar * Palmer, A. C. & Sorger, P. K.
Combination Cancer Therapy Can Confer Benefit via Patient-to-Patient Variability without Drug Additivity or Synergy. _Cell_ 171, 1678–1691 e1613 (2017). Article CAS PubMed PubMed Central
Google Scholar * Sathyanarayanan, V. & Neelapu, S. S. Cancer immunotherapy: Strategies for personalization and combinatorial approaches. _Molecular oncology_ 9, 2043–2053 (2015).
Article CAS PubMed PubMed Central Google Scholar * Patel, S. P. & Kurzrock, R. PD-L1 Expression as a Predictive Biomarker in Cancer Immunotherapy. _Molecular cancer therapeutics_
14, 847–856 (2015). Article CAS PubMed Google Scholar * Zhang, L. _et al_. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. _The New England journal of
medicine_ 348, 203–213 (2003). Article CAS PubMed Google Scholar * Sato, E. _et al_. Intraepithelial CD8+ tumor-infiltrating lymphocytes and a high CD8+/regulatory T cell ratio are
associated with favorable prognosis in ovarian cancer. _Proceedings of the National Academy of Sciences of the United States of America_ 102, 18538–18543 (2005). Article ADS CAS PubMed
PubMed Central Google Scholar * Galon, J. _et al_. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. _Science (New York, N.Y.)_ 313,
1960–1964 (2006). Article ADS CAS Google Scholar * Chen, D. S. & Mellman, I. Oncology meets immunology: the cancer-immunity cycle. _Immunity_ 39, 1–10 (2013). Article PubMed CAS
Google Scholar * Gooden, M. J., de Bock, G. H., Leffers, N., Daemen, T. & Nijman, H. W. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with
meta-analysis. _British journal of cancer_ 105, 93–103 (2011). Article CAS PubMed PubMed Central Google Scholar * Matsumoto, H. _et al_. Increased CD4 and CD8-positive T cell infiltrate
signifies good prognosis in a subset of triple-negative breast cancer. _Breast cancer research and treatment_ 156, 237–247 (2016). Article CAS PubMed Google Scholar * Lopez, M. _et al_.
The role of regulatory T lymphocytes in the induced immune response mediated by biological vaccines. _Immunobiology_ 211, 127–136 (2006). Article CAS PubMed Google Scholar * Yagi, T.
_et al_. PD-L1 Expression, Tumor-infiltrating Lymphocytes, and Clinical Outcome in Patients With Surgically Resected Esophageal Cancer. _Annals of surgery_ 269, 471–478 (2019). Article
PubMed Google Scholar * Jiang, D. _et al_. Tumour infiltrating lymphocytes correlate with improved survival in patients with esophageal squamous cell carcinoma. _Scientific reports_ 7,
44823 (2017). Article ADS CAS PubMed PubMed Central Google Scholar * Jesinghaus, M. _et al_. Increased intraepithelial CD3+ T-lymphocytes and high PD-L1 expression on tumor cells are
associated with a favorable prognosis in esophageal squamous cell carcinoma and allow prognostic immunogenic subgrouping. _Oncotarget_ 8, 46756–46768 (2017). Article PubMed PubMed Central
Google Scholar * Zheng, X. _et al_. Prognostic Role of Tumor-Infiltrating Lymphocytes in Esophagus Cancer: a Meta-Analysis. _Cellular physiology and biochemistry: international journal of
experimental cellular physiology, biochemistry, and pharmacology_ 45, 720–732 (2018). Article CAS Google Scholar * Sharpe, A. H. & Freeman, G. J. The B7-CD28 superfamily. _Nature
reviews. Immunology_ 2, 116–126 (2002). Article CAS PubMed Google Scholar * Wallin, J. J., Liang, L., Bakardjiev, A. & Sha, W. C. Enhancement of CD8+ T cell responses by ICOS/B7h
costimulation. _Journal of immunology (Baltimore, Md.: 1950)_ 167, 132–139 (2001). Article CAS Google Scholar * Hald, S. M. _et al_. LAG-3 in Non-Small-cell Lung Cancer: Expression in
Primary Tumors and Metastatic Lymph Nodes Is Associated With Improved Survival. _Clinical lung cancer_ 19, 249–259 e242 (2018). Article CAS PubMed Google Scholar * He, Y. _et al_. LAG-3
Protein Expression in Non-Small Cell Lung Cancer and Its Relationship with PD-1/PD-L1 and Tumor-Infiltrating Lymphocytes. _Journal of thoracic oncology: official publication of the
International Association for the Study of Lung Cancer_ 12, 814–823 (2017). Article Google Scholar * Zhang, Y. _et al_. Prognostic Value of Lymphocyte Activation Gene-3 (LAG-3) Expression
in Esophageal Squamous Cell Carcinoma. _Journal of Cancer_ 9, 4287–4293 (2018). Article CAS PubMed PubMed Central Google Scholar * Jiang, J. _et al_. Decreased galectin-9 and increased
Tim-3 expression are related to poor prognosis in gastric cancer. _PloS one_ 8, e81799 (2013). Article ADS PubMed PubMed Central CAS Google Scholar * Zhuang, X. _et al_. Ectopic
expression of TIM-3 in lung cancers: a potential independent prognostic factor for patients with NSCLC. _American journal of clinical pathology_ 137, 978–985 (2012). Article CAS PubMed
Google Scholar * He, Y. _et al_. TIM-3, a promising target for cancer immunotherapy. _OncoTargets and therapy_ 11, 7005–7009 (2018). Article CAS PubMed PubMed Central Google Scholar *
Tsutsumi, S. _et al_. Programmed death-ligand 1 expression at tumor invasive front is associated with epithelial-mesenchymal transition and poor prognosis in esophageal squamous cell
carcinoma. _Cancer science_ 108, 1119–1127 (2017). Article CAS PubMed PubMed Central Google Scholar * van Hagen, P. _et al_. Preoperative chemoradiotherapy for esophageal or junctional
cancer. _The New England journal of medicine_ 366, 2074–2084 (2012). Article PubMed Google Scholar * Kim, H. R. _et al_. PD-L1 expression on immune cells, but not on tumor cells, is a
favorable prognostic factor for head and neck cancer patients. _Scientific reports_ 6, 36956 (2016). Article ADS CAS PubMed PubMed Central Google Scholar Download references
ACKNOWLEDGEMENTS This work was supported by a grant from the National research foundation (NRF), Republic of Korea (NRF-2017R1D1A1B03029874, NRF-2017M3A9E9072669, NRF-2019M3A9B6065231, and
NRF-2016R1A5A2945889). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Division of Medical Oncology, Department of Internal Medicine, Yonsei Cancer Center, Severance Hospital, Yonsei
University College of Medicine, Seoul, Korea Min Hee Hong, Byoung Chul Cho & Hye Ryun Kim * Department of Pathology, Gangnam Severance Hospital, Yonsei University College of Medicine,
Seoul, Korea Su-Jin Shin * Division of Gastroenterology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea Sung Kwan Shin * Department of Thoracic and
Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea Dae Joon Kim & Seong Yong Park * Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center,
Sungkyunkwan University School of Medicine, Seoul, Korea Jae Ill Zo & Young Mog Shim * Department of Pathology, Konkuk University Medical Center, Konkuk University School of Medicine,
Seoul, Republic of Korea Seung Eun Lee * Department of Pathology and Translational Genomics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea Yoon-La Choi
Authors * Min Hee Hong View author publications You can also search for this author inPubMed Google Scholar * Su-Jin Shin View author publications You can also search for this author
inPubMed Google Scholar * Sung Kwan Shin View author publications You can also search for this author inPubMed Google Scholar * Dae Joon Kim View author publications You can also search for
this author inPubMed Google Scholar * Jae Ill Zo View author publications You can also search for this author inPubMed Google Scholar * Young Mog Shim View author publications You can also
search for this author inPubMed Google Scholar * Seung Eun Lee View author publications You can also search for this author inPubMed Google Scholar * Byoung Chul Cho View author publications
You can also search for this author inPubMed Google Scholar * Seong Yong Park View author publications You can also search for this author inPubMed Google Scholar * Yoon-La Choi View author
publications You can also search for this author inPubMed Google Scholar * Hye Ryun Kim View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS
M.H.H., and S.S. were involved in manuscript preparation and editing. H.R.K. and Y.C. were involved in study concepts. Y.C., B.C.C. and H.R.K. were involved in study design. D.J.K., S.Y.P.,
S.K.S., S.E.L. and Y.C. were involved in data acquisition. S.S., Y.C., J.I. Zo. and Y.M.S. were involved in quality control of data and algorithms and data analysis and interpretation.
M.H.H., S.S. and S.K.S. all contributed equally to the work and should be considered co-first authors. S.Y.P., Y.C. and H.R.K. contributed equally to this work as corresponding authors.
CORRESPONDING AUTHORS Correspondence to Seong Yong Park, Yoon-La Choi or Hye Ryun Kim. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL
INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY
INFORMATION RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution
and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if
changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the
material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to
obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS
ARTICLE Hong, M.H., Shin, SJ., Shin, S.K. _et al._ High CD3 and ICOS and low TIM-3 expression predict favourable survival in resected oesophageal squamous cell carcinoma. _Sci Rep_ 9, 20197
(2019). https://doi.org/10.1038/s41598-019-56828-7 Download citation * Received: 04 July 2019 * Accepted: 04 December 2019 * Published: 27 December 2019 * DOI:
https://doi.org/10.1038/s41598-019-56828-7 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
