Primary efficacy of percutaneous microwave ablation of malignant liver tumors: comparison of stereotactic and conventional manual guidance
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT In this study, we compare the primary efficacy of computed tomography-navigated stereotactic guidance to that of manual guidance for percutaneous microwave ablation of liver
malignancies. In total, 221 patients (140, 17, and 64 with hepatocellular carcinoma, cholangiocellular carcinoma, and liver metastases, respectively) with 423 treated liver lesions underwent
microwave ablation (MWA). Manual guidance (M) and stereotactic guidance (S) were used for 136 and 287 lesions, respectively. The primary endpoint was the primary efficacy and the secondary
endpoint was the radiation dose. A generalised estimating equation was applied to analyse the correlation between the primary efficacy (lesion basis) and the type of guidance, size and
location of lesion. The primary efficacy rate was significantly higher in the S-group (84.3%) than in the M-group (75.0%, p = 0.03). Lesion size > 30 mm was negatively correlated with the
efficacy rate (odds ratio 0.38; 95% confidence interval 0.20–0.74). Stereotactic guidance was associated with a significantly lower dose length product (p < 0.01). In this retrospective
study, percutaneous microwave ablation under stereotactic guidance exhibited significantly greater primary efficacy than conventional manual guidance. SIMILAR CONTENT BEING VIEWED BY OTHERS
MICROWAVE VERSUS RADIOFREQUENCY ABLATION FOR THE TREATMENT OF LIVER MALIGNANCIES: A RANDOMIZED CONTROLLED PHASE 2 TRIAL Article Open access 10 January 2022 2450-MHZ MICROWAVE ABLATION OF
LIVER METASTASES UNDER 3.0 T WIDE-BORE MAGNETIC RESONANCE GUIDANCE: A PILOT STUDY Article Open access 25 July 2022 OPTIMIZING MICROWAVE ABLATION PLANNING WITH THE ABLATION SUCCESS RATIO
Article Open access 26 March 2025 INTRODUCTION In recent years, percutaneous ablation of primary and secondary liver tumors has become an important alternative to surgical resection and is
likely to occupy a more central role in the management of patients with hepatocellular carcinoma (HCC) and liver metastases from colorectal cancer (CRC)1. One crucial factor during the
procedure is the complete ablation of the malignant lesion with a sufficient safety margin. A study by Solbiati et al. showed that re-treatment of residual tumor tissue after ablation of
colorectal metastasis significantly increased patient survival, thus emphasising the importance of complete tumor eradication2. Similarly, for HCC, an initial complete response to
percutaneous ablation was associated with improved survival3. Therefore, one predictive factor for patient survival is a high primary efficacy rate, which is defined as the percentage of
tumor tissue that is successfully eradicated after the initial ablation procedure3,4,5. To achieve high primary efficacy, the ablation probes must be placed as precisely as possible in or
around the tumor, which can be a major challenge when tumors are in difficult locations. A large-scale study with over 1000 ablations showed that the incorporation of computer-assisted
targeting techniques limits operator dependency and optimises the results6. To achieve optimal probe placement, the improved visualisation of the lesion through software support, is a great
advantage. Thus, both the anatomical situation and the expected ablation zone, in relation to the semi-automatically segmented tumor can be visualised in all spatial directions and also
three-dimensionally (3D), which enables a correction or adjustment of the ablation settings, if necessary. To our knowledge, no studies have compared primary efficacy rates between
stereotactic ablation and conventional manual ablation. Therefore, the purpose of this study was to evaluate the primary efficacy of stereotactic ablation for malignant liver tumors and
compare the findings with those for conventional manual ablation in a retrospective cohort. RESULTS PATIENT AND TUMOR CHARACTERISTICS The baseline patient characteristics are summarised in
Table 1. A total of 221 patients (179 male) were included in the study. The median age was 64 years (range 30–85). In total, 285 ablation sessions were performed with a median number of
treatment sessions per patient of one (range 1–5) and 170 patients required one, 41 required two, and 10 required three or more sessions. A median of one (range 1–5) tumor was treated per
ablation session. TUMOR CHARACTERISTICS A total of 423 tumors spread across all liver segments were treated using microwave ablation (MWA) with either stereotactic (S) or manual guidance (M)
(Table 2).The two most frequent tumor entities were HCC (n = 274) and CRC liver metastasis (n = 82), followed by cholangiocellular carcinoma CCC (n = 30).The median tumor size was 17 mm,
with 61 tumors being 30 mm or larger. PRIMARY EFFICACY AND PROGNOSTIC FACTORS The primary efficacy rate using stereotactic guidance was significantly higher than that using manual guidance
in both the univariable (p = 0.046) and multivariable model (p = 0.028). There was a negative correlation between increasing tumor size and efficacy rate (p ≤ 0.01).The results of
generalized estimating equation GEE are shown in Table 3. Difficult to reach lesion locations or the proximity to large vessels were not predictive factors of primary efficacy. RADIATION
DOSE The mean dose length product (DLP) was 2633 µGy⋅ cm (range 679–9969 µGy cm). Stereotactic guidance was associated with a significantly lower DLP (Table 4). PROCEDURAL SAFETY In total,
out of 423 MWA procedures, 248 (87.02%) were performed without any adverse events. Grade I and II complications (any deviation from the normal postinterventional course, e.g. fever or pain
medication) occurred in 20 MWA procedures (7.02%). There was no significant difference in the frequency of complications (p = 0.75) between the groups. One patient died after MWA due to an
accidental puncture of the pericardium with hemopericardium. The incidence of all documented complications is listed in Table 5. DISCUSSION One predictive factor for patient survival is a
high primary efficacy rate, which is defined as the percentage of successfully eradicated tumor tissue after the initial ablation procedure3,4,5. The present study showed that the primary
efficacy rate for stereotactic ablation was significantly higher than that for manual ablation (84.3% vs. 75.0%) in patients with malignant liver tumors. Lesion size > 30 mm and efficacy
rate were negatively correlated (odds ratio (OR) 0.38; 95% confidence interval 0.20–0.74). Stereotactic guidance was associated with a significantly lower DLP (p < 0.01). To achieve the
most accurate probe position, navigation systems can be a helpful tool7,8,9,10,11,12,13. An accurate placement of the probe is a precondition for a high primary efficacy. A precise
positioning of the probe, supported by a navigation software that improves visualization of the lesion, leads to complete eradication of the tumor and a sufficient safety margin. The
improved display of the lesion and the expected ablation zone in all spatial directions and in 3D enables to optimize the ablation settings. Studies have also shown that the use of
stereotactic navigation for liver ablation leads to a very high accuracy and primary efficacy, with a mean lateral error of 3.6 ± 2.5 mm at the needle tip, an angular error of 1.3° ± 1.2°,
and a longitudinal error of − 7.4 ± 6.2 mm at the needle tip14,15. This method can also contribute to precise probe placement during other surgeries such as liver biopsy16 or ablation of
osteoid osteomas17. Our study demonstrated for the first time that the primary efficacy for malignant liver tumor ablation was significantly higher with stereotactic navigation (S-group)
than with conventional fluoroscopic navigation (M-group). In fact, 84.3% of lesions in the S-group were completely ablated; this value was 75.0% in the M-group. However, there was a negative
correlation between an increase in the tumor size and the primary efficacy rate (OR 0.38; 95% CI 0.20–0.74). In addition, the use of stereotactic navigation resulted in a significantly
lower radiation dose (p < 0.01). This is consistent with the findings of previous studies on stereotactic ablation, which found that the total DLP was significantly lower in the S-group
than in the M-group (2115 µGy⋅ cm (SD 276) vs. 3109 µGy⋅ cm (SD 1137), respectively; p < 0.01)18. A potential limitation of our work is the long duration of ablations, factors affecting
the ablation settings, and involvement of multiple specialists (three experienced radiologists L.P.B, L.L., and P.W.). Thus, it is possible that inter-user differences could have influenced
our results or led to bias. Although the longer time span may have led to distortions, it has indeed ensured that a large number of patients could be included in this study. Furthermore, the
ablations were performed by the same team during the entire time; hence, a high level of experience of the interventionalists can be assumed. There was also no significant change in the
choice of the ablation systems. Over the entire period, the AcculisMicrowave Tissue Ablation (MTA) System (AngioDynamics, Latham, NY, USA), the Emprint™ Ablation System (Medtronic,
Minneapolis, USA) and subsequently, the NeuWave Ablation System (Ethicon, Johnson & Johnson, Bridgewater New Jersey and Cincinnati, Ohio) were used. Until 2016 all ablations were
performed manually. From 2016 onwards, the Cascination navigation system became available and was used whenever possible. The shorter period of navigation use, with a corresponding learning
curve and better results, further supports the use of navigation for improved primary efficacy. The indications based on the BCLC guidelines have not changed over the years. In our opinion,
despite the long time span, constant and comparable conditions can be assumed. Another limitation is the retrospective single-center study design. Nevertheless, we are convinced that the
large sample size has provided valuable data with a consistently high level of quality. To conclude, we demonstrated that the use of stereotactic navigation improved primary efficacy
compared to conventional manual guidance. Considering the limitations mentioned above, for the first time, we have shown that SMWA might lead to a higher primary efficacy rate compared to
non-navigated ablation. Future, prospective studies should focus on improving navigation systems so that the treatment of patients can be continuously optimized. METHODS STUDY DESIGN AND
PARTICIPANT SELECTION The ethics committee of the University of Regensburg approved this retrospective study (approval no. 16-101-0137). All procedures performed in this study were in
accordance with the ethical standards of our institution and with the 1964 Helsinki declaration and its later amendments. Patients gave written informed consent for use of their imaging and
clinical data before the ablation procedure for research purposes. Written informed consent was obtained for publication of identifying information/images. In all patients, the treatment
plan was established by a multidisciplinary tumor board consisting of hepatologists, abdominal surgeons, oncologists, and interventional radiologists. The decision to perform HCC ablation
was based on Barcelona Clinic Liver Cancer guidelines (BCLC). Ablation was primarily performed on patients with very early and early HCC who were neither eligible for liver resection nor
liver transplantation. Apart from a few individual cases discussed in the tumor conference, patients with single tumors smaller than 5 cm or up to three tumors smaller than 3 cm each, were
treated. Contraindications included vascular invasion, extrahepatic disease, or extrahepatic metastases that could not be resected. Colorectal liver metastases were treated when surgical
resection was not possible. The ablation registry of the University of Regensburg was searched for all patients who received percutaneous liver tumor ablation between 8/2011 and 04/2020. We
included all patients treated with MWA with or without stereotactic navigation support. The following parameters were assessed for both groups: * Primary efficacy as determined by a lack of
residual tumor tissue on the 6-week follow-up magnetic resonance (MRI) scans with a liver-specific contrast agent; the scans were evaluated by two experienced readers (L.B. [9 years of
experience] and L.L. [8 years of experience]). * Size of the tumor (long and short axes of the axial plane). * Location of the tumor, determined through radiological assessments (computed
tomography (CT)/MRI). * DLP according to the dose report. * Complications (during the procedures or postinterventional) as noted in the patient records and classified according to the
Clavien-Dindo system. All data generated or analysed during this study are included in this published article and its supplementary information files (Supplementary Table S1). NAVIGATION
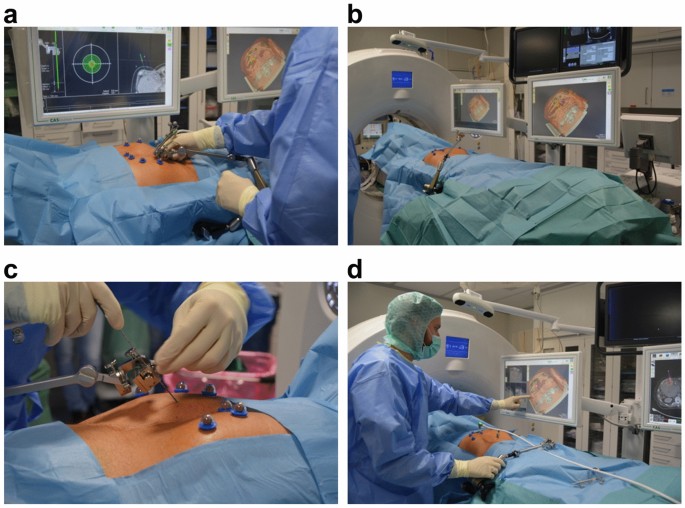
SYSTEM AND ABLATION PROCEDURE All ablation procedures were performed under general anesthesia. Temporary apnoea was used during the planning CT scan and probe positioning to control
respiratory movement in both groups (Fig. 1a). In the S-group, sterile radiopaque reflective optical markers were attached to the patient after sterile scrubbing and draping. The tracking
camera was fixed above the patient to track the markers and the aiming device (Fig. 1b). An arterial and portal venous planning CT scan (Definition Edge or Somatom Sensation 16, Siemens
Healthcare, Forchheim, Germany) was acquired under apnoea, and the data were sent to the navigation system (CAS-One IR, CAScination AG, Bern, Switzerland) adjacent to the CT gantry. If not
automatically recognized, the spherical markers were manually identified. The registration was layer-based. However, if there were significant deviations due to different breathing
positions, the registration was performed manually, by point-based method. The desired ablation area and the target and entry points of the probe(s) were defined on multiplanar
reconstructions of the 3D-CT datasets. The resulting trajectories were visualized on the 2D and 3D reconstructions accordingly (Fig. 2). The probes were then positioned using the CAScination
aiming device, which allows locking of the probe axis relative to the patient (Fig. 1c). Before ablation, an unenhanced verification scan was performed and, if necessary, the probes were
manually repositioned (Fig. 1d) and Fig. 3. Another native control scan was performed after completion of the ablation to exclude acute complications. In the M-group, probe placement was
achieved manually with repeated verifications using CT fluoroscopy after an initial 3-phase planning CT scan. CT fluoroscopy is an acquisition mode that allows continuous image updates using
an in-room footswitch. During the ablation procedure, the probes were manually repositioned until the ablation area seemed to cover the tumor with a sufficient safety margin. If necessary,
several overlapping ablations were performed. For MWA, depending on tumor configuration and relationship to the surrounding tissue, either the AcculisMicrowave Tissue Ablation (MTA) System
(AngioDynamics, Latham, NY, USA), the Emprint™ Ablation System (Medtronic, Minneapolis, USA), or the NeuWave Ablation System (Ethicon, Johnson & Johnson, Bridgewater New Jersey and
Cincinnati, Ohio) was used. The navigation system was selected based on the specialists´ experience and the manufacturer’s. The Emprint system, for example, was used for round shaped tumors
whereas the Accoulis was more likely used for large lesions with an ovoid configuration. STATISTICAL ANALYSIS Continuous data are presented as median, interquartile range, and data range,
whereas categorical data are presented as absolute and relative frequencies. A GEE was applied to analyze the correlation between the primary efficacy (lesion basis) and the type of guidance
(manual vs. stereotactic), size, and location of the lesion. As multiple lesions were ablated in the same patient, we included repeated measure analyses in our model. Adjusted odds ratios
(ORs) and corresponding 95% confidence intervals (CIs) are reported as effect estimates. A two-sided p-value of < 0.05 was considered statistically significant. All analyses were
performed using R 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria). DATA AVAILABILITY All data generated or analysed during this study are included in this published article
and its supplementary information files (Supplementary Table S1). REFERENCES * Freedman, J., Nilsson, H. & Jonas, E. New horizons in ablation therapy for hepatocellular carcinoma.
_Hepatic. Oncol._ 2, 349–358 (2015). Article Google Scholar * Solbiati, L. _et al._ Small liver colorectal metastases treated with percutaneous radiofrequency ablation: Local response rate
and long-term survival with up to 10-year follow-up. _Radiology_ 265, 958–968 (2012). Article PubMed Google Scholar * Sala, M. _et al._ Initial response to percutaneous ablation predicts
survival in patients with hepatocellular carcinoma. _Hepatology_ 40, 1352–1360 (2004). Article PubMed Google Scholar * Takahashi, S. _et al._ Initial treatment response is essential to
improve survival in patients with hepatocellular carcinoma who underwent curative radiofrequency ablation therapy. _Oncology_ 72, 98–103 (2007). Article PubMed Google Scholar * Ahmed, M.
_et al._ Image-guided tumor ablation: Standardization of terminology and reporting criteria—A 10-year update. _Radiology_ 273, 241–260 (2014). Article PubMed Google Scholar * Beermann, M.
_et al._ 1000 consecutive ablation sessions in the era of computer assisted image guidance—Lessons learned. _Eur. J. Radiol. Open_ 6, 1–8 (2019). Article PubMed Google Scholar * Solomon,
S. B., Patriciu, A., Bohlman, M. E., Kavoussi, L. R. & Stoianovici, D. Robotically driven interventions: A method of using CT fluoroscopy without radiation exposure to the physician.
_Radiology_ 225, 277–282 (2002). Article PubMed Google Scholar * Schullian, P., Putzer, D., Eberle, G., Laimer, G. & Bale, R. Simultaneous stereotactic radiofrequency ablation of
multiple (≥ 4) liver tumors: Feasibility, safety, and efficacy. _J. Vasc. Interv. Radiol._ 31, 943–952 (2020). Article PubMed Google Scholar * Schullian, P. _et al._ Stereotactic
radiofrequency ablation as first-line treatment of recurrent hcc following hepatic resection. _Eur. J. Surg. Oncol._ https://doi.org/10.1016/j.ejso.2020.03.207 (2020). Article PubMed
Google Scholar * Schullian, P. _et al._ Safety and efficacy of stereotactic radiofrequency ablation for very large (≥8 cm) primary and metastatic liver tumors. _Sci. Rep._ 10, 1618 (2020).
Article ADS CAS PubMed PubMed Central Google Scholar * Tinguely, P. _et al._ Stereotactic image-guided microwave ablation for malignant liver tumors-a multivariable accuracy and
efficacy analysis. _Front. Oncol._ 10, 842 (2020). Article PubMed PubMed Central Google Scholar * Perrodin, S. _et al._ Percutaneous stereotactic image-guided microwave ablation for
malignant liver lesions. _Sci. Rep._ 9, 13836 (2019). Article ADS PubMed PubMed Central Google Scholar * Schullian, P., Putzer, D., Laimer, G., Levy, E. & Bale, R. Feasibility,
safety, and long-term efficacy of stereotactic radiofrequency ablation for tumors adjacent to the diaphragm in the hepatic dome: A case-control study. _Eur. Radiol._ 30, 950–960 (2020).
Article PubMed Google Scholar * Widmann, G., Schullian, P., Haidu, M., Fasser, M. & Bale, R. Targeting accuracy of CT-guided stereotaxy for radiofrequency ablation of liver tumors.
_Minim. Invas. Ther. Allied Technol._ 20, 218–225 (2011). Article Google Scholar * Haidu, M. _et al._ Stereotactic radiofrequency ablation of unresectable intrahepatic cholangiocarcinomas:
A retrospective study. _Cardiovasc. Interv. Radiol._ 35, 1074–1082 (2012). Article Google Scholar * Schullian, P., Widmann, G., Lang, T. B., Knoflach, M. & Bale, R. Accuracy and
diagnostic yield of CT-guided stereotactic liver biopsy of primary and secondary liver tumors. _Comput. Aided Surg._ 16, 181–187 (2011). Article PubMed Google Scholar * Widmann, G.,
Schullian, P., Fasser, M., Niederwanger, C. & Bale, R. CT-guided stereotactic targeting accuracy of osteoid osteoma. _Int. J. Med. Robot. Comput. Assist. Surg._ 9, 274–279 (2013).
Article Google Scholar * Beyer, L. P. _et al._ Stereotactically navigated percutaneous microwave ablation (MWA) compared to conventional MWA: a matched pair analysis. _Int. J. Comput.
Assist. Radiol. Surg._ 13, 1991–1997 (2018). Article CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS We would like to thank Editage (www.editage.com) for English language
editing. FUNDING Open Access funding enabled and organized by Projekt DEAL. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Radiology, University Medical Center Regensburg,
93053, Regensburg, Germany Jan Schaible, Lukas Lürken, Niklas Verloh, Ingo Einspieler, Christian Stroszczynski & Lukas Beyer * Department of Radiology and Nuclear Medicine, Hospital
Braunschweig, Braunschweig, Germany Philipp Wiggermann * Center for Clinical Studies, University Medical Center Regensburg, Regensburg, Germany Florian Zeman * Department of Radiology,
Brandenburg Medical School, Brandenburg, Germany Andreas G. Schreyer * Department of Microinvasive Therapy (SIP), Medical University Innsbruck, Innsbruck, Austria Reto Bale Authors * Jan
Schaible View author publications You can also search for this author inPubMed Google Scholar * Lukas Lürken View author publications You can also search for this author inPubMed Google
Scholar * Philipp Wiggermann View author publications You can also search for this author inPubMed Google Scholar * Niklas Verloh View author publications You can also search for this author
inPubMed Google Scholar * Ingo Einspieler View author publications You can also search for this author inPubMed Google Scholar * Florian Zeman View author publications You can also search
for this author inPubMed Google Scholar * Andreas G. Schreyer View author publications You can also search for this author inPubMed Google Scholar * Reto Bale View author publications You
can also search for this author inPubMed Google Scholar * Christian Stroszczynski View author publications You can also search for this author inPubMed Google Scholar * Lukas Beyer View
author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS J.S. and L.P.B. wrote the manuscript. J.S., L.L. and B.P. collected data. N.V., C.S., R.B. and
A.G.S. performed literature review. L.P.B., P.W. and L.L. performed the ablations. F.Z. carried out the statistical evaluation. J.S., I.E., P.W. and L.P.B. prepared figures. All authors
reviewed the manuscript. CORRESPONDING AUTHOR Correspondence to Jan Schaible. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION
PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY
INFORMATION. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution
and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if
changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the
material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will
need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE
CITE THIS ARTICLE Schaible, J., Lürken, L., Wiggermann, P. _et al._ Primary efficacy of percutaneous microwave ablation of malignant liver tumors: comparison of stereotactic and conventional
manual guidance. _Sci Rep_ 10, 18835 (2020). https://doi.org/10.1038/s41598-020-75925-6 Download citation * Received: 24 February 2020 * Accepted: 18 October 2020 * Published: 02 November
2020 * DOI: https://doi.org/10.1038/s41598-020-75925-6 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable
link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
