Propensity score-matched analysis for comparing transpancreatic sphincterotomy and needle-knife precut in difficult biliary cannulation
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

Transpancreatic sphincterotomy (TPS) can be an alternative approach of difficult biliary access in endoscopic retrograde cholangiopancreatography (ERCP). We aimed to evaluate the efficacy
and safety of TPS compared to needle-knife precut (NKP), considering the early and late outcomes of both techniques. The prospectively collected clinical data, ERCP procedure findings, and
outcomes of patients who underwent ERCP with difficult biliary access in our hospital from July 2016 to January 2018 were retrospectively analyzed. The patients were divided into two groups
according to the applied secondary cannulation techniques. The propensity score matching (PSM) was applied to reduce the potential selection bias and unify the preventive measures of
post-ERCP pancreatitis (PEP) in both groups. A total of 125 patients were enrolled in this study, with 54.4% male and a mean age of 63.29 ± 16.33 years. NKP group included 82 patients, and
43 patients received TPS. Prophylactic pancreatic stents were placed in all patients with TPS and 58.5% of patients with NKP. After applying PSM, the cohort was comprised to 86 patients with
43 patients in each TPS and NKP groups. Successful selective cannulation was achieved by 95.3% using TPS and by 93% using NKP. The mean procedure time was shorter in the TPS group without
significant difference. Compared to NKP, using TPS did not affect the rate of PEP. Moreover, TPS was associated with less frequent post-ERCP bleeding and perforation, but without significant
differences (all p > 0.05). Patients who received TPS or NKP had no symptoms related to papillary stenosis or chronic pancreatitis during the follow-up period. In conclusion, using TPS in
difficult cannulation cases was useful to achieve success cannulation with an acceptable PEP rate and less frequent post-ERCP bleeding and perforation compared to NKP. There were no symptoms
related to papillary stenosis or chronic pancreatitis during the follow-up period.
Endoscopic retrograde cholangiopancreatography (ERCP) has become a common therapeutic intervention for several pancreaticobiliary conditions. Selective cannulation of the common bile duct
(CBD), which is the key to the successful biliary therapeutic procedure, could be achieved after a few attempts of standard cannulation methods in around 80% of cases1.
According to the European Society of Gastrointestinal Endoscopy (ESGE) guidelines, biliary cannulation is defined as difficult if cannulation lasts longer than five minutes, success requires
more than five attempts, or the guidewire accidentally passes the pancreatic duct at least twice. Therefore, additional cannulation methods are often needed in difficult cannulation cases.
Difficult cannulation is frequently reported as a risk factor for adverse events with a probability of failed biliary cannulation ranges from 5 to 18% of cases1,2,3.
Different techniques are reported in the literature regarding papillary cannulation in difficult cases4,5,6,7. Transpancreatic sphincterotomy (TPS) is a technique used for exposing the bile
duct orifice by making an incision through the septum between the pancreatic and biliary duct. It involves the placement of a papillotome in the pancreatic duct and performing sphincterotomy
in the direction of the bile duct, then extending the sphincterotomy to cannulate the biliary duct1,8,9. TPS is resorted when attempts with the primary methods had failed and should be
performed by experienced endoscopists.
ERCP is an invasive procedure with an overall adverse events rate of approximately 4–11%, and the most common one is post-ERCP pancreatitis (PEP)10,11. Using advanced cannulation techniques
in a native papilla is considered a risk factor of PEP. The ESGE suggested prophylactic pancreatic stenting in patients receiving TPS to decrease the risk of PEP1,12,13. Pancreatic duct
stricture or chronic pancreatitis could be developed after pancreatic sphincterotomy; therefore, a long follow-up period is needed to detect those adverse outcomes.
Several retrospective studies compared the effects of different cannulation techniques on ERCP outcomes, but without considering uniformed PEP preventive measures4,14,15. Therefore, more
studies are needed to clarify the role of TPS in the case of difficult biliary access. This study tries to fill the gap and offer a new evaluation of the efficacy and adverse events rate of
TPS compared to NKP, considering the same PEP preventive methods in both techniques. Furthermore, we aim to evaluate the impact of TPS in developing any symptoms related to the ductal
stricture or chronic pancreatitis (CP) during the 6-month follow-up period.
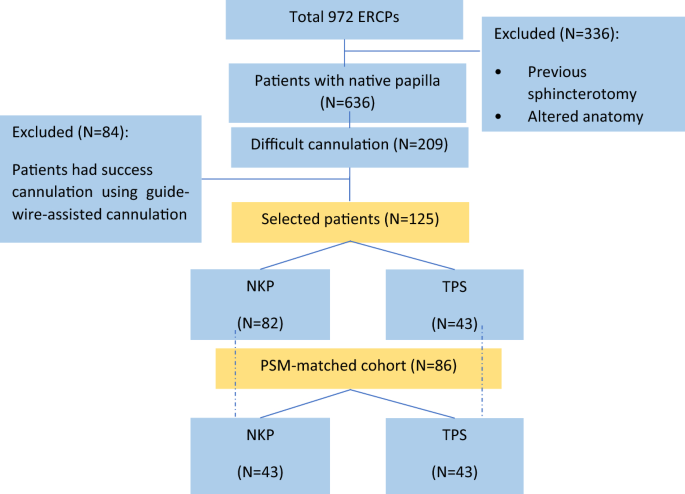
The study protocol was approved by the institutional review board of the Second Affiliated Hospital of Nanjing Medical University. The clinical data of 972 patients who underwent ERCP in our
hospital between July 2016 and January 2018 were prospectively collected, and all patients gave their written informed consent to participate in ERCP after full explanation of the
procedure. The clinical procedures were carried out in accordance with the Declaration of Helsinki. After excluding the patients with previous sphincterotomy and patients with altered
anatomy, the difficult cannulation was reported in 209 cases (see Fig. 1), and these cases were retrospectively analyzed to achieve the aim of this study.
Study design and sample breakdown based on used difficult cannulation techniques before and after propensity score matching (PSM).
In 84 difficult cannulation cases, repeating guidewire-assisted cannulation attempts was a successful method to achieve deep cannulation. Accordingly, a total of 125 difficult cannulation
cases required using NKP or TPS during ERCP to achieve biliary cannulation. For the purpose of analysis, those 125 patients were divided into two groups based on the secondary cannulation
technique. Patients' clinical and therapeutic features, including demographics, indications, procedure details, and ERCP related adverse events, were analyzed. Additionally, comorbidities
were weighted using the Charlson Comorbidity Index (CCI) depending on the risk of mortality associated with each comorbid disease. We used the cutoff of CCI ≥ 2 to stratify the patients
based on their comorbidities.
All ERCP procedures were performed by three experienced endoscopists in our center with an experience of over 250 ERCPs/year in the last 5 years. Patients underwent therapeutic ERCP using
standard side-view duodenoscope following an overnight fast under conscious sedation. Patients were monitored continuously during the procedure using a pulse oximeter, electrocardiography
monitoring, and an automatic blood pressure recording device. Supplementary oxygen was provided when needed. Prophylactic octreotide dose was administered to all patients before ERCP for PEP
prevention. Besides, a prophylactic pancreatic stent (PPS) was deployed in difficult cannulation cases, especially with multiple pancreatic cannulations.
Initial biliary cannulation was routinely performed using a guidewire-assisted technique with sphincterome. Needle knife precut or transpancreatic sphincterotomy was resorted when selective
biliary access failed after standard cannulation attempts. Both conventional precut sphincterotomy and needle knife fistulotomy were used to apply the precut method in difficult cannulation
cases. Choosing the suitable secondary cannulation technique was according to the expertise of endoscopists, which was mainly based on the orientation and morphology of the papilla and the
repetitive unintended guidewire insertion into the pancreatic duct. NKP was considered as the preferred choice in the absence of pancreatic cannulation and the cases with impacted biliary
stones at the ampulla or the distal CBD. In the cases of prior guidewire insertion in the pancreatic duct, TPS was performed using a sphincterotome towards the bile duct axis. After that,
the pancreatic stent was placed, then the biliary cannulation was performed (see Fig. 2). An additional needle-knife incision was applied in some cases from the upper end of the previous
pancreatic sphincterotomy towards 10 o'clock to expose the bile duct.
Transpancreatic sphincterotomy technique. (a) Fluoroscopy image showed the guidewire inserted in the pancreatic duct. (b) The septum was cut with a sphincterotome from the pancreatic duct
towards the bile duct axis. (c) The placement of pancreatic duct stent. (d) After a stent was placed in the pancreatic duct. (e) Cannulation toward the bile duct was performed. (f) The
biliary cannulation was successfully achieved.
The standard process in our hospital requires that all the patients should be hospitalized 3 days after the procedure for observation and serum amylase testing after the procedure. All
discharged patients were informed to stay in contact for any delayed adverse events.
According to ESGE criteria1, cannulation was considered difficult if either took more than 5 min, if it needed more than five cannulation attempts on the papilla, or if the pancreatic duct
was cannulated more than one time.
All adverse events were defined according to published criteria. Post-ERCP pancreatitis was defined as new or worsened abdominal pain with an elevated amylase at least three times the upper
limit of the normal level, at more than 24 h after ERCP, requiring admission or prolongation of planned hospitalization. Post-procedural bleeding evidenced by a drop-in haemoglobin > 2 g/dl.
Perforation was diagnosed according to the imaging evidence of intraperitoneal or retroperitoneal leakage of contrast agent observed under radioscopy.
Differences among different patient were determined by using Fisher's exact test for categorical variables, and non-categorical variables with the Mann–Whitney U test. Univariate regression
was performed with significant variables (p
