Risk factors and prognosis of postoperative delirium in nonagenarians with hip fracture
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT Hip fractures in nonagenarians is one of the great challenges for patients of this age, the family and the larger society. The purpose of this study was to investigate the risk
factors and prognosis of postoperative delirium in nonagenarians with hip fracture. 199 Eligible patients were enrolled. Confusion Assessment Method (CAM) were used to identify the delirium.
Logistic regressions were used to investigate the effect of 18 pre-existing conditions on postoperative delirium. Prognosis of postoperative delirium in nonagenarians with hip fracture were
also be evaluated. The results indicated the following: (1) the prevalence of postoperative delirium among nonagenarians with hip fracture was 28.1% (56 of 199); (2) coexisting disease ≥ 4
(OR = 5.355, 95% CI = 1.394–9.074, P = 0.007), longer admission to operating time (OR = 1.514, 95% CI = 1.247–1.837, P = 0.000), and general anesthesia (OR = 2.086, 95% CI = 1.804–7.968, P =
0.032) were independent risk factors for postoperative delirium in nonagenarians with hip fracture; (3) nonagenarians with postoperative delirium had a predominantly high burden of
perioperative complications, long length of stay, and postoperative mortality at 30 days follow-up and 1 year follow-up than the patients without postoperative delirium. The results could
enable clinicians to improve outcome after operation in nonagenarians with hip fracture. SIMILAR CONTENT BEING VIEWED BY OTHERS ANALYSIS OF RISK FACTORS FOR POSTOPERATIVE DELIRIUM IN
MIDDLE-AGED AND ELDERLY FRACTURE PATIENTS IN THE PERIOPERATIVE PERIOD Article Open access 10 August 2023 ASSOCIATION BETWEEN MULTIDIMENSIONAL PROGNOSTIC INDEX (MPI) AND PRE-OPERATIVE
DELIRIUM IN OLDER PATIENTS WITH HIP FRACTURE Article Open access 08 October 2022 RISK FACTORS AND MORTALITY OF PATIENTS UNDERGOING HIP FRACTURE SURGERY: A ONE-YEAR FOLLOW-UP STUDY Article
Open access 15 June 2020 INTRODUCTION Delirium, characterized by a change in mental status, loss of cognitive and perceptive functions, and alterations in the sleep cycle, is a common
complication in patients with hip fracture1. The reported prevalence of postsurgical delirium after hip fracture ranged from 28 to 61%2. Postsurgical delirium is associated with greater
morbidity and mortality, longer length of hospital stays, and higher rates of institutionalization, and has been suggested as significant predictor of poor prognosis in hip fracture
patients3,4,5. Predisposing factors, including dementia, underlying comorbidity, and precipitating events (including major trauma and anesthesia) play an important role in the occurrence of
delirium. Identifying the predisposing factors is critical for risk stratification for postsurgical delirium among the elderly hip fracture. Further, a complex intervention the preventable
risk factors would enable clinicians to achieve the maximum favorable outcome for patients with hip fracture. China has the largest population in the world and is facing population aging; as
a result, the risk of hip fractures increases, in particular in nonagenarians6. Nonagenarians with hip fractures are different from younger hip fracture patients. In one study, the group of
nonagenarians with hip fracture was with more women patients, higher prevalence of heart disease, lower prevalence of COPD and diabetes than younger patients with hip fracture7. A recent
study reported that patients older than 90 years with hip fractures had higher mortality rates per year than younger patients8. Baseline functional status was poorer among the nonagenarians.
The prevalence of independent for transferring from bed to chair before the fracture varied between 50 and 70% depending on the different countries and districts7. In addition, medical
complications after hip fracture, such as delirium, had been found more frequently in nonagenarian patients with hip fracture during their hospital stay9. Due to the reasons above,
nonagenarians with hip fracture are often excluded from clinical trials. Therefore, research on hip fractures in nonagenarians highlights the urgent need for management of this subgroup, and
is of great challenges to the patients, the family and the larger society. The purpose of this report was (i) to find the prevalence of postoperative delirium in nonagenarians with hip
fracture; (ii) to find which variables can predict postoperative delirium in nonagenarians with hip fracture; (iii) to find prognosis of postoperative delirium in nonagenarian patients with
hip fracture. METHODS STUDY DESIGN AND SETTING We performed a retrospective analysis of demographic, clinical, and delirium data in consecutive hip fracture patients at the Department of
Orthopedics, the Seventh Medical Center of People’s Liberation Army, between January 2012 and December 2020. This study was approved by the Seventh Medical Center of People’s Liberation Army
Institutional Review Board, all methods were carried out in accordance with relevant guidelines and regulations. And the patients or their family gave informed consent to use their data.
Data including age, gender, past medical history (hypertension, coronary heart disease, diabetes mellitus, chronic obstructive pulmonary diseases, lung infection, stroke, and renal
insufficiency), post-injury factors (admission to operating time, fracture type, white blood cell count, hemoglobin, and albumin), surgery related factors (type of anesthesia, amount of
blood transfusion, and surgical method), delirium (time of occurrence and duration), and length of stay were obtained by reviewing their medical records. Routine follow-up visits were
scheduled at 30 days and 1 year after surgery. Mortality outcomes of inpatients using the date of death were obtained from the medical records. Mortality status and walking ability at 1 year
follow-up were performed by using hospital records and/or phoning the patient’s family by a dedicated person. SUBJECTS Participants who met the following inclusion criteria were included:
(1) were aged ≥ 90 years; (2) walk independently or with the aid of tools before injury; (3) intertrochanteric fracture or femoral neck fracture; (4) low energy damage (a fall from standing
height or lower); (5) treated surgically for single hip fracture. Participants were excluded if they met any of the following criteria: (1) the presence of preoperative dementia; (2)
pathological fracture; (3) the American Society of Anesthesiologists (ASA) rating scale was Classes V; (4) refused follow-up after discharge or with incomplete data. Each patient was
identified by two senior orthopedists and fulfilled the criteria above. ASSESSMENT PROCEDURES The following assessments were all performed at the Seventh Medical Center of People’s
Liberation Army. The most widely used instrument for identification of delirium is the Confusion Assessment Method (CAM)10,11. CAM scores are determined by four features: (1) acute onset and
fluctuating changes in mental status, (2) inattention, (3) disorganized or incoherent thinking, and (4) an altered level of consciousness. The diagnosis of delirium by CAM requires the
presence of features (1) and (2) and either feature (3) or (4). After surgery, delirium based on CAM was assessed daily, and the enrolled patients were divided into delirium group and
delirium-free group. Because of difficulty in identifying true delirium and the residual effects of anesthesia, assessment of delirium on the day of surgery was excepted. The presence of
preoperative cognitive impairment/dementia was determined within 24 h of admission using the Mini-Mental State Examination (MMSE). The scores ranged from 0 to 30, with higher scores
indicating higher cognitive function. Normal mental status was defined as a MMSE score of 25 points or more (maximum score is 30). Walking ability at 1 year follow-up were categories into
independent (independent community or household ambulator), dependent (patient with a minimum level of mobility) and not walking (nonambulator). INTERVENTIONS After preoperative examination,
assessment and prepare for surgery, surgical treatment was given as soon as possible according to the type of fracture. Patients with Garden type I and II femoral neck fracture had been
treated with cancellous screws. Patients with Garden type III and IV femoral neck fracture underwent hip arthoplasty. Sliding hip screw (SHS) and intramedullary nail were allocated to the
treatment of stable intertrochanteric (A1, A2.1) and unstable intertrochanteric (A2.2, A2.3, A3), respectively. Different rehabilitation programs were applied to postoperative patients by
specialized rehabilitation therapist according to different fracture sites and treatments. The follow-up was performed by a dedicated person over the phone who were blinded to the grouping
situation at 30 day and 1 year after surgery. STUDY VARIABLES We obtained data on a wide range of factors that might contribute to delirium in patients after hip fracture surgery. 18
variables were grouped into the following categories:(1) sociodemographic data (age and gender; n = 2 variables), (2) past medical history (hypertension, coronary heart disease, diabetes
mellitus, chronic obstructive pulmonary diseases, lung infection, stroke, and renal insufficiency, and number of comorbidities; n = 8 variables), (3) post-injury factors (admission to
operating time, fracture type, white blood cell count, hemoglobin, and albumin; n = 5 variables), and (4) surgery related factors ( anesthesia, surgical approach, and amount of blood
transfusion; n = 3 variables). There were three kinds of variables in this model. Continuous variables: age, admission to operating time, white blood cell count, hemoglobin, amount of blood
transfusion, and albumin. Dichotomous variables: gender, fracture type, anesthesia, hypertension, coronary heart disease, diabetes mellitus, chronic obstructive pulmonary diseases, lung
infection, stroke, renal insufficiency, and number of comorbidities(≥ 4 or < 4). Patients receive either regional anesthesia (spinal, epidural, or both techniques combined with no
sedation) or general anesthesia (intravenous, inhalational, or combined anesthetic agents). Categorical variables: type of surgery (intramedullary nail, cancellous screws, SHS, hip
arthroplasty). STATISTICAL ANALYSIS We compared patients with delirium and those without using univariate analysis. Continuous variables were expressed as means ± standard deviation (SD) or
median (interquartile range, IQR) according to the distribution. The Shapiro–Wilk test was used to assess normal distribution. Differences between groups were analyzed using the independent
Student’s t test for normally distributed variables, and Wilcoxon rank-sum test for non-normally distributed variables. Categorical variables were shown as frequencies (percentages), and
compared by χ2 test. Multivariate logistic regression analyses were used to identify independent risk factors for delirium in nonagenarians after hip fracture surgery. Variables eligible for
inclusion in the multivariate models included those significant at P < 0.05 in univariate analyses. All statistical analyses were performed using SPSS software (version 24.0), and a P
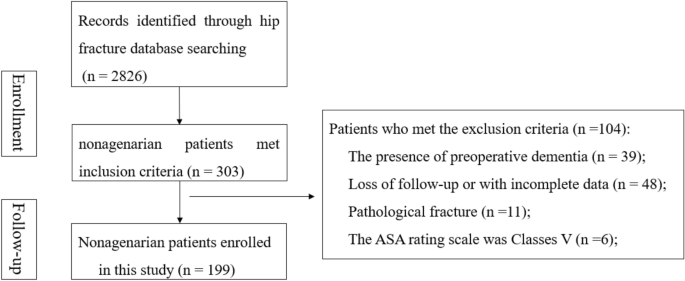
< 0.05 was considered statistically significant. RESULTS SUBJECTS’ CHARACTERISTICS A flow chart of hip fracture in nonagenarians screening from the database of hip fracture in our center
was presented in Fig. 1. After excluding patients who did not meet the inclusion criteria, a total of 199 patients were eligible for the study. Table 1 presents the baseline characteristics
of the 199 patients included, 36.7% were men, 27.1% were general anesthesia, and 64.8% developed intertrochanteric fracture. The surgical type included intramedullary nail (122, 61.3%),
cancellous screws(25, 12.6%), SHS (10, 5.0%), hip arthoplasty (42, 21.1%); The median number of subjects recruited was 92.00 years (IQR 33–482), and the median admission to operating time
was 4 days (IQR3–5). In our study, the prevalence of postoperative delirium among nonagenarians with hip fracture was 28.1% (56 of 199), and was more likely to happen at 1-3d after surgery.
COMPARISON OF NONAGENARIANS WITH HIP FRACTURE IN DELIRIUM GROUP AND DELIRIUM-FREE GROUP Comparing patients with and without postoperative delirium (Table 2), we found that age (P = 0.010),
stroke (P = 0.032), number of comorbidities (P = 0.001), admission to operating time (P = 0.000), anesthesia type (P = 0.006), blood transfusion (P = 0.034), hemoglobin (P = 0.019), and
albumin (P = 0.011) differed significantly. RISK FACTORS FOR POSTOPERATIVE DELIRIUM IN NONAGENARIANS WITH HIP FRACTURE All these factors were included in multivariable logistic analysis
(Table 3). There was no multicollinearity (all VIFs < 10). Multivariate logistic regression identified comorbidities greater than or equal to 4 (OR = 5.355, 95%CI = 1.394–9.074, P =
0.007), longer admission to operating time (OR = 1.514, 95%CI = 1.247–1.837, P = 0.000) and general anesthesia (OR = 2.086, 95%CI = 1.804–7.968, P = 0.032) were independent risk factors of
postoperative delirium in nonagenarians with hip fracture. COMPARISON OF THE OUTCOME OF PATIENTS WITH OR WITHOUT DELIRIUM IN NONAGENARIANS WITH HIP FRACTURE Comparison of the characteristics
of delirium group and delirium-free group in the follow-up were shown in Table 4. Nonagenarians in delirium group had a predominantly high burden of perioperative complications than in
delirium-free group, as represented by 7.1% cerebrovascular events, 21.4% adverse cardiac events, and 30.4% lung infection. We found no significant differences of gastrointestinal bleeding
and other complications between the two groups. The length of stay in delirium group was predominantly longer than the delirium-free group. 30 days mortality after surgery, 1 year mortality
after surgery, and overall mortality were significantly higher in delirium group than in delirium-free group. May be due to similar walking ability before the fracture, which could predict
activity level after 1 year, both groups had similar walking ability at 1 year follow-up. DISCUSSION Delirium is a common neuropsychiatric complication after hip fracture surgery among the
elderly12. Based on reports in different regions, delirium is quite different among elderly hip fracture patients13. Reported prevalence rates of delirium among elderly hip fracture patients
vary greatly due to differing definitions, tools of diagnosis, and patient populations14. In our study, the prevalence of postoperative delirium among nonagenarians with hip fracture was
26.1% (41 of 157), and was more likely to happen at 1-3d after surgery. Compared with elderly patients in the reported study, the incidence of postoperative delirium among nonagenarians in
our study does not show a particularly high incidence15. The possible reasons were as follows. First, this is likely related to a selection bias where healthier nonagenarians were offered an
operation. Second, a specialized department for elderly hip fractures has been established to manage this subgroup. Geriatric consultation and attendance both pre and postoperatively have
been performed, which could decrease the rate of post‐operative complications. Third, patients with dementia before injury were excluded to remove the effect of dementia on delirium. There
are many risk factors for postoperative delirium16,17, including advanced age, dementia, anemia, dehydration, pain, anesthesia and other factors. However, this is the first study to examine
risk factors associated with postoperative delirium among nonagenarians with hip fracture. Our findings suggested that coexisting disease greater than or equal to 4, having a longer
admission to operating time and general anesthesia were risk factors of postoperative delirium in nonagenarians with hip fracture. Different medical comorbidities, such as dementia,
hypertension, COPD, and heart failure had been found in previous studies18,19,20,21. The number of coexisting disease, instead of specific disease was used in our study to decrease the
heterogeneity of patients. In fact, the number of comorbidities can better reflect the body's physiological reserve compared to a single comorbid disease. Under stresses such as pain,
bed rest, and surgery, delirium is more likely to attack the patients with more coexisting disease, and ultimately influence the outcome. Clinically, we need to pay special attention to
patients with a large number of comorbidities. The primary disease should be controlled as much as possible to reduce the incidence of postoperative delirium. Our results showed that the
time interval between admission and operation was negatively associated with postoperative delirium among nonagenarians. Delay between admission and operation leads to increased long time in
bed, pain, dehydration, and inverted sleep rhythm, which may result the postoperative delirium among nonagenarians. Exploring the optimal operation time for nonagenarians may reduce the
incidence of postoperative delirium. At present, the relationship between anesthesia and postoperative delirium is not clear. Abbott et al22 showed that decrease in delirium in patients
receiving regional anesthesia compared with those receiving general anesthesia. While Bryson et al.23 reported a relationship between postoperative delirium and certain drugs in general
anesthesia, such as fentanyl and propofol. In our study, general anesthesia was one of the risk factors of postoperative delirium in nonagenarians with hip fracture. Accordingly, exposure to
general anesthesia should be avoided on such patients. Due to high mortality and fragility, nonagenarians with hip fracture completed the 1-year follow-up was rarely in the reported
research. Our study confirmed that delirium was an independent risk factor of hip fracture patients at 30 days mortality after surgery, 1 year mortality after surgery, and over-all
mortality, even after adjusting for various potential confounding factors. Comparing the delirium-free group, nonagenarians in delirium group had a predominantly high burden of perioperative
complications, long length of stay, high overall mortality, and high mortality after surgery at 30 days follow-up and 1 year follow-up. At 1 year follow-up, we assigned similar
postoperative walking ability between delirium group and delirium-free group, which had similar mobility before the fracture. The fact in elderly patients that functional status before hip
fracture was important when predicting the postoperative walking ability was also applicable to nonagenarians. There were several limitations to our study. First, our study was
retrospective, prospective research should be performed to validate our findings. Second, the analysis was performed using a dataset obtained from a single center, selection bias exits.
Third, the cause of death had not been analyzed. CONCLUSION In our study, the incidence of postoperative delirium, which is more likely to happen at 1-3d after surgery and remission within 1
week, was high in patients with postoperative delirium among nonagenarians. Coexisting disease greater than or equal to 4, having a longer admission to operating time and general anesthesia
were found to be statistically significant risk factors of postoperative delirium in nonagenarians with hip fracture. Comparing the control group, patients with delirium had a predominantly
high burden of perioperative complications, long length of stay, high overall mortality, and high mortality after surgery at 30 days follow-up and 1 year follow-up. After adjusting for
various potential confounding factors, delirium were independent risk factors of 30 days mortality after surgery and 1 year mortality after surgery for hip fracture patients (Supplementary
Information). DATA AVAILABILITY All data generated or analysed during this study are included in this published article and its supplementary information files. REFERENCES * Rengel, K. F.,
Pandharipande, P. P. & Hughes, C. G. Postoperative delirium. _Presse Med._ 47(4 Pt 2), e53–e64. https://doi.org/10.1016/j.lpm.2018.03.012 (2018). Article Google Scholar * Lee, K. H.,
Ha, Y. C., Lee, Y. K., Kang, H. & Koo, K. H. Frequency, risk factors, and prognosis of prolonged delirium in elderly patients after hip fracture surgery. _Clin. Orthop. Relat. Res._
469(9), 2612–2620 (2011). Article Google Scholar * Lee, P. J. & Shorten, G. D. Delirium after hip fracture surgery. _J. Clin. Anesth._ 58, 119–120.
https://doi.org/10.1016/j.jclinane.2019.06.034 (2019). Article Google Scholar * van de Ree, C. L. P. _et al._ The prevalence and prognostic factors of psychological distress in older
patients with a hip fracture: A longitudinal cohort study. _Injury_ 51(11), 2668–2675. https://doi.org/10.1016/j.injury.2020.07.049 (2020). Article Google Scholar * Lee, S. J. _et al._
Postoperative delirium after hip surgery is a potential risk factor for incident dementia: A systematic review and meta-analysis of prospective studies. _Arch. Gerontol. Geriatr._ 87, 103977
(2020). Article Google Scholar * Lo, J. C. _et al._ Trends in mortality following hip fracture in older women. _Am. J. Manag Care_ 21(3), e206–e214 (2015). Google Scholar *
Mayordomo-Cava, J. _et al._ Hip fracture in nonagenarians: Characteristics and factors related to 30-day mortality in 1177 patients. _J. Arthroplasty_ 35(5), 1186–1193 (2020). Article
Google Scholar * Leal, J. A. _et al._ Patients aged ninety years and older are exposed to increased risk of one-year mortality after hip fractures. _Eur. J. Orthop. Surg. Traumatol._ 31(7),
1501–1506 (2021). Article Google Scholar * Graver, A. _et al._ Comorbid profile rather than age determines hip fracture mortality in a nonagenarian population. _HSS J._ 11(3), 223–235.
https://doi.org/10.1007/s11420-015-9435-y (2015). Article Google Scholar * Arshi, A. _et al._ Predictors and sequelae of postoperative delirium in geriatric hip fracture patients.
_Geriatr. Orthop. Surg. Rehabil._ 5(9), 2151459318814823. https://doi.org/10.1177/2151459318814823 (2018). Article Google Scholar * Setters, B. & Solberg, L. M. Delirium. _Prim. Care_
44(3), 541–559. https://doi.org/10.1016/j.pop.2017.04.010 (2017). Article Google Scholar * Mattison, M. L. P. Delirium. _Ann. Intern. Med._ 173(7), ITC49–ITC64 (2020). Article Google
Scholar * Harris, M. J., Brovman, E. Y. & Urman, R. D. Clinical predictors of postoperative delirium, functional status, and mortality in geriatric patients undergoing non-elective
surgery for hip fracture. _J. Clin. Anesth._ 58, 61–71. https://doi.org/10.1016/j.jclinane.2019.05.010 (2019). Article Google Scholar * Wu, J., Yin, Y., Jin, M. & Li, B. The risk
factors for postoperative delirium in adult patients after hip fracture surgery: A systematic review and meta-analysis. _Int. J. Geriatr. Psychiatry_ 36(1), 3–14 (2021). Article Google
Scholar * Uzoigwe, C. E. _et al._ Factors associated with delirium and cognitive decline following hip fracture surgery. _Bone Jt. J._ 102-B(12), 1675–1681.
https://doi.org/10.1302/0301-620X.102B12.BJJ-2019-1537.R3 (2020). Article Google Scholar * Wu, J. _et al._ The risk factors for postoperative delirium in adult patients after hip fracture
surgery: A systematic review and meta-analysis. _Int. J. Geriatr. Psychiatry_ 36(1), 3–14. https://doi.org/10.1002/gps.5408 (2021). Article Google Scholar * Plaza-Carmona, M.,
Requena-Hernández, C. & Jiménez-Mola, S. Predictors of delirium in octogenarian patients hospitalized for a hip fracture. _Int. J. Environ. Res. Public Health_ 17(20), 7467.
https://doi.org/10.3390/ijerph17207467 (2020). Article Google Scholar * Cher, E. W. L., Allen, J. C., Howe, T. S. & Koh, J. S. B. Comorbidity as the dominant predictor of mortality
after hip fracture surgeries. _Osteoporos. Int._ 30(12), 2477–2483. https://doi.org/10.1007/s00198-019-05139-8 (2019). Article Google Scholar * Zhu, C. _et al._ Risk factors for
postoperative delirium after spinal surgery: A systematic review and meta-analysis. _Aging Clin. Exp. Res._ 32(8), 1417–1434 (2020). Article Google Scholar * Kim, E. M., Li, G. & Kim,
M. Development of a risk score to predict postoperative delirium in patients with hip fracture. _Anesth. Analgs._ 130(1), 79–86 (2020). Article Google Scholar * Smith, T. O. _et al._
Factors predicting incidence of post-operative delirium in older people following hip fracture surgery: A systematic review and meta-analysis. _Int. J. Geriatr. Psychiatry_ 32(4), 386–396
(2017). Article CAS Google Scholar * Abbott, T. E. F. & Pearse, R. M. Depth of anesthesia and postoperative delirium. _JAMA_ 321(5), 459–460. https://doi.org/10.1001/jama.2019.0164
(2019). Article Google Scholar * Bryson, G. L. & Wyand, A. Evidence-based clinical update: General anesthesia and the risk of delirium and postoperative cognitive dysfunction. _Can. J.
Anaesth._ 53(7), 669–677. https://doi.org/10.1007/BF03021625 (2006). Article Google Scholar Download references ACKNOWLEDGEMENTS The authors would like to thank the patients in our study.
AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Neurorehabilitation, China Rehabilitation Research Center, Capital Medical University School of Rehabilitation Medicine, No. 10,
JiaoMenBei Lu, Beijing, 100068, China Shengjie Zhao * Department of Orthopedics, The Seventh Medical Center of China General Hospital of People’s Liberation Army, Beijing, 100700, China
Tiansheng Sun, Jianzheng Zhang, Xiaobin Chen & Xiaowei Wang Authors * Shengjie Zhao View author publications You can also search for this author inPubMed Google Scholar * Tiansheng Sun
View author publications You can also search for this author inPubMed Google Scholar * Jianzheng Zhang View author publications You can also search for this author inPubMed Google Scholar *
Xiaobin Chen View author publications You can also search for this author inPubMed Google Scholar * Xiaowei Wang View author publications You can also search for this author inPubMed Google
Scholar CONTRIBUTIONS Z.S.J., S.T.S., Z.J.Z., C.X.B., and W.X.W. are the investigators responsible for project design and protocol writing. Z.S.J. and W.X.W. have participated in sample size
calculation and statistical analysis planning. S.T.S., Z.J.Z., and C.X.B. have contributed to study background, general design and study variable definition. Z.S.J. and W.X.W. have
contributed to the preparation of the project and have read and approved the final manuscript. CORRESPONDING AUTHOR Correspondence to Xiaowei Wang. ETHICS DECLARATIONS COMPETING INTERESTS
The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and
institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0
International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the
source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's
Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not
permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Zhao, S., Sun, T., Zhang, J. _et al._ Risk factors and prognosis of postoperative
delirium in nonagenarians with hip fracture. _Sci Rep_ 13, 2167 (2023). https://doi.org/10.1038/s41598-023-27829-4 Download citation * Received: 22 September 2021 * Accepted: 09 January 2023
* Published: 07 February 2023 * DOI: https://doi.org/10.1038/s41598-023-27829-4 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable
link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
