A language-independent hearing screening self-test at school-entry
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT The usage of a tablet-based language-independent self-test involving the recognition of ecological sounds in background noise, the Sound Ear Check, was investigated. The results of
692 children, aged between 5 and 9 years and 4 months, recruited in seven different countries, were used to analyze the validity and the cultural independence of test. Three different test
procedures, namely a monaural adaptive procedure, a procedure presenting the sounds dichotically in diotic noise, and a procedure presenting all the sounds with a fixed signal-to-noise ratio
and a stopping rule were studied. Results showed high sensitivity and specificity of all three procedures to detect conductive, sensorineural and mixed hearing loss > 30 dB HL.
Additionally, the data collected from different countries were consistent, and there were no clinically relevant differences observed between countries. Therefore, the Sound Ear Check can
offer an international hearing screening test for young children at school entry, solving the current lack of hearing screening services on a global scale. SIMILAR CONTENT BEING VIEWED BY
OTHERS DIGITAL SPEECH HEARING SCREENING USING A QUICK NOVEL MOBILE HEARING IMPAIRMENT ASSESSMENT: AN OBSERVATIONAL CORRELATION STUDY Article Open access 10 September 2024 PSYCHOMETRIC
APPRAISAL OF THE KURDISH VERSION OF THE REVISED HEARING HANDICAP INVENTORY-SCREENING Article Open access 18 November 2024 OPTIMIZATION OF UTILIZING THE HHIE-S FOR HEARING SCREENING IN OLDER
PEOPLE: A CROSS-SECTIONAL STUDY OF ASSOCIATED FACTORS Article Open access 24 May 2025 INTRODUCTION About two to three in 1000 children are born with hearing loss1, and about the same number
acquire hearing loss during early childhood2. Untreated hearing loss increases the risk for speech, language, and learning difficulties and low social-communicative abilities3,4,5,6,7,8.
Early intervention has proven highly effective in reducing these adverse effects9,10,11,12,13 and therefore, cost-effectiveness ratios of childhood hearing screening are estimated to be
extremely high14,15,16. Many middle- and high-income countries have implemented newborn hearing screening (NHS) programs to ensure early detection and rehabilitation of congenital hearing
loss, and a third of these NHS programs capture data from at least 85% of newborns17. However, late-onset, progressive, and acquired hearing losses present themselves at a later stage.
Consequently, despite the installation of NHS, a significant number of children are still at risk for the numerous negative side effects of untreated childhood hearing loss3,4,5,6,7,8.
Therefore, the World Health Organization (WHO) and the European Federation of Audiology Societies (EFAS) strongly recommend screening all children for hearing loss and ear diseases at school
entry as a bare minimum15,18. However, in most countries, systematic school-age hearing screening (SHS) does not exist beyond NHS2,19, and if at all, data on the few installed SHS projects
are poorly documented, the protocols and practices are inconsistent, and loss of follow-up of the referred children is an ubiquitous concern14. As a result, novel and inventive approaches
are required to meet the recommendations of the WHO and EFAS and provide qualitative, standardized protocols for childhood hearing screening. For a couple of years, the EFAS workgroup for
childhood hearing screening has been working on a new and innovative approach to providing one standardized test method that can solve the lack of childhood hearing screening in many
countries. This novel methodology, utilizing Signal-in-Noise testing as its foundation, forms a solution to the challenges systematic childhood hearing screening currently faces. The test of
interest, named the ‘Sound Ear Check’ or ‘SEC’, is a closed-set, tablet-based self-test based on the perception of sounds, such as the barking of a dog or the honking of a car, chosen to
have similar temporal and spectral features as natural speech, covering the frequency range that is most important for speech understanding20,21. A pilot study with the SEC in adults showed
a high correlation with pure tone audiometry, the golden standard in audiology, and the Digit Triplet Test (DTT)22, a widely used speech understanding test used for hearing screening and
diagnostics23,24. The SEC is a self-test operated on a standard digital device such as a tablet with standard headphones, reducing the material cost largely and making a trained test leader
no longer required. Additionally, due to the language independence of the SEC's sound material, one version can be used across countries, which brings additional costs and scientific
resources needed for translation studies back to zero. Therefore, the SEC methodology may be an easily implementable, language-independent, low-cost alternative with similar results to, for
example, the widely used DTT22. In the current international study, the final version of the SEC was developed and validated. This test version was optimized for the application in young
children, implementing elements such as animated drawings and automatic test progression to increase the attention and motivation of the children tested. This study investigated and compared
the sensitivity and specificity of the SEC for normal-hearing (NH) children and children with various degrees of conductive (CHL), sensorineural (SNHL) and mixed hearing loss (MHL) with a
standard monaural adaptive procedure, such as tested in the pilot study22, a procedure with a fixed signal-to-noise ratio (SNR) and a stopping rule that has the potential to strongly
decrease the duration of the test25, and a binaural antiphasic procedure, i.e. a procedure where the noise is presented without phase difference between ears and the stimuli with a phase
difference of 180° between ears, that can half the duration and increase the sensitivity and specificity of the test for various types of hearing loss26,27. Moreover, this research
investigated whether, when used in a wide variety of countries, cultural differences affected the sound-reception threshold (SoRT)-values, their standard deviation (SD) as a measure of the
stability of the test, and the familiarity of the sounds. This study used data from seven countries that cover a broad range of cultures, including Belgium, Slovenia, Russia, Germany,
Norway, Israel, and Turkey, to deliver a language-independent hearing screening self-test for school-entry that can solve the lack of hearing screening in many countries. METHODS
PARTICIPANTS NH and hard of hearing (HoH) children aged between 5 and 9 years and 4 months (mean: 7 years 1 month ± 10 months) were recruited. The parent(s) and/or legal guardian(s) of the
participating children received a detailed explanation and signed an informed consent form before participation. A simplified informed consent explaining the important aspects of the
research was signed by the participating children. For the SEC with the monaural adaptive procedure (SECREF) and the SEC with the monaural fixed procedure (SECFIX), ears were considered
separately, meaning the same child could be included in different hearing loss groups. This means that a possible asymmetry in hearing is not considered for the analyses of the results of
the SECREF and SECFIX. However, as the sounds used in the SEC have spectral and temporal features similar to speech, the model of Plomp (1978)28 can be used to estimate the possibility of
crossover hearing affecting the results. The noise in the SECREF and SECFIX is fixed at 65 dB SPL. When speech is presented through air conduction, the interaural attenuation would be 40 dB
SPL, meaning that the noise would be heard at 25 dB SPL in the other ear. According to the model of Plomp (1978)28, the SRTs of normal hearing people start worsening when the noise is
presented at 30 dB SPL or lower. Therefore, even when the better ear overhears the stimuli and the noise without any distortion during the transmission, the results would still deviate from
the norm value and the hearing loss would still be detected. If the better ear is influenced by the worse ear, a screening test should be able to detect this problem so that the patient can
be referred for diagnostics. The diagnostic phase should then identify what causes the hearing problem and how to best rehabilitate it. For the antiphasic procedure (SECAPH), both ears were
considered together, and children were divided into groups based on the hearing in both ears (Table 1). Ears were considered NH when the air conduction (AC) pure-tone average (PTA)0.5–4 kHz
was < 20 dB HL and all thresholds from 250 to 8000 Hz were < 20 dB HL. Ears with a PTA0.5–4 kHz < 20 dB HL, but one or more thresholds ranging from 250 to 8000 Hz ≥ 20 dB HL were
considered as NH+, as depending on the configuration of the hearing loss, the effects on the SoRT-values obtained with the SEC versions can be very heterogenous, which asks for a more
detailed analysis. Ears were considered to have CHL when an AC PTA0.5–4 kHz ≥ 20 dB HL, a bone conduction (BC) PTA0.5–4 kHz < 20 dB HL, and an Air Bone Gap (ABG) ≥ 10 dB were present.
Ears were considered to have SNHL when an AC PTA0.5–4 kHz ≥ 20 dB HL, a BC PTA0.5–4 kHz ≥ 20 dB HL, and an ABG < 10 dB were present. Ears were considered to have MHL when an AC PTA0.5–4
kHz ≥ 20 dB HL, a BC PTA0.5–4 kHz ≥ 20 dB HL, and an ABG ≥ 10 dB were present. When a child had a hearing loss > 80 dB HL in their worse ear, the results on the SECAPH were removed from
the statistical analysis, as well as the results of SECREF and the SECFIX in that ear specifically, as it would be impossible to hear the noise and stimuli when such hearing loss was
present. The number of children included per country, the number of ears/children included per SEC-test, and the average PTA0.5–4 kHz per hearing group and per SEC version are given in Table
1. In total, data from 692 children were collected. Two hundred fifty-eight were female, 281 were male, and of 153 children, no data was available on their sex. In 111 of the cases, a
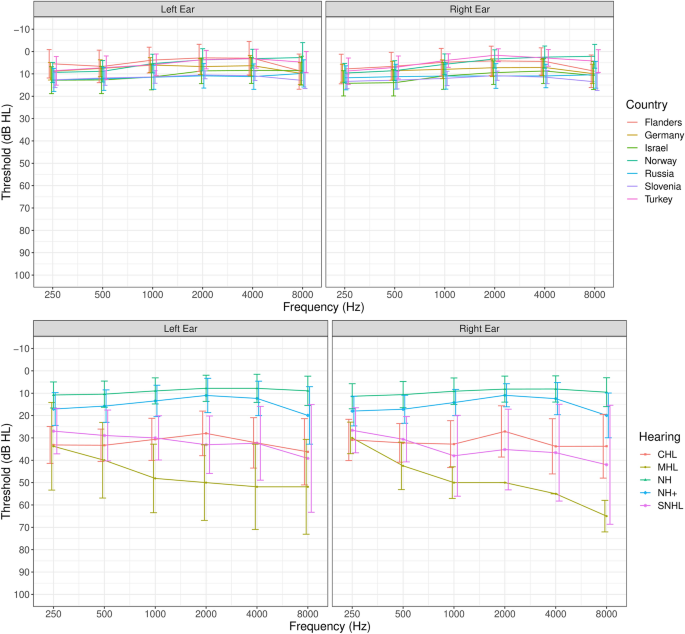
different mother tongue was spoken by the child than the official language of the country where they were living. In 101 of these cases, the child was NH. The average audiogram and SD for
the different hearing groups and the average audiogram of NH ears per country are presented in Fig. 1. MATERIALS All audiometers used were calibrated according to ISO standards. The
following audiometers were used: Madsen Orbiter 922 (_Flanders_), Madsen Midimate 622 (_Flanders_), Auritec AT-1000 (_Germany_), Auritec AT-900 (_Germany_), GSI Audiostar PRO (_Turkey_),
Maico MA 52 (_Israel_), Interacoustics AD 229e (_Israel_), Entomed SA-201 (_Norway_), Interacoustics Clinical AC40 (_Slovenia_), AD226 (_Russia_), and a GSI-61 audiometer (_Russia_).
Transducers similar or equal to RadioEar DD65 embedded in peltor caps were used when testing outside of an audio booth. Transducers similar or equal to Telephonics TDH39 were used for
testing inside of an audio booth. The SEC was performed on a 7-inch Samsung Galaxy Tab A tablet connected to RadioEar DD65 transducers embedded in Peltor caps. RadioEar DD65 transducers
yield a damping of ~ 30–40 dB SPL on the frequencies important for speech understanding. The test setup was calibrated with SWN at 80 dB Sound Pressure Level (SPL) with a Brüel & Kjaer
Sound level meter 2260 and a Brüel & Kjaer 4153 artificial ear using the flat plate. The study was designed and conducted according to the Declaration of Helsinki. This study was
approved by the Ethics Committee Research UZ/KU Leuven. All methods were performed in accordance with the relevant guidelines and regulations. SOUND EAR CHECK VERSIONS Three different test
procedures were used. The interface of the SEC was the same for all procedures (Fig. 2). All SEC versions used seven sounds presented in sound-weighted noise (SWN), i.e., noise with a
spectrum identical to the average spectrum of the test materials22. Seven animated drawings, chosen based on recognizability, were shown on the tablet screen (Fig. 2). The sounds, including
barking of a dog, honking of a car, a ringing phone, a playing piano, ringing bells, mewing of a cat, and chirping of a bird, were chosen based on recognizability and spectral and temporal
features, which were kept as close as possible to the features of natural speech22. All procedures consisted of three subsequent phases. The first phase, the acclimatization phase, was the
same for all procedures. In this phase, the sounds were presented diotically at a fixed SNR of 0 dB SNR and the noise fixed at 65 dB SPL. Each sound was presented in random order until
identified correctly, after which the image disappeared from the screen as a sign that the sound-image mapping was correct. The fixed SNR of 0 dB SNR was chosen so that children can get used
to more challenging, but most likely not impossible, SNRs before the start of the actual training and test phases. During these phases the images did not disappear after a correct answer,
so the participant did not receive direct feedback. A fixed SNR of 0 dB SNR can be too challenging for children with more severe hearing loss. However, as the SEC is meant to be a screening
test, it does not target children with severe hearing loss but children with undetected hearing loss, and this is most likely not severe. Additionally, in the case of an undetected severe
hearing loss, the inability to perform the test indicates hearing loss with a referral for diagnostics as a result. For SECREF, the second phase was a diotic training phase consisting of 21
trials with every sound played three times (3 × 7 sounds) in random order. The training phase used an adaptive procedure in which the stimuli were adapted in steps of 2 dB, and the noise was
fixed at 65 dB SPL. A fixed noise level of 65 dB SPL can be challenging for participants with severe hearing loss. However, as the SEC is designed to be a screening test, it targets people
with undetected, and therefore most likely mild to moderate hearing loss. For these people, 65 dB SPL is still suprathreshold. In the case of an undetected severe hearing loss, the inability
to perform the test will again result in a referral for diagnostics. For the first seven trials, a 1-up-1-down procedure was used to converge fast to the SoRT. A 1-up-2-down procedure was
used for the subsequent trials, targeting a recognition probability of 71% correct29. The third phase was the actual test phase, which used 21 trials per ear and the same procedure as the
training phase but with monaural stimulus presentation, first testing the left ear, then the right ear. The contralateral ear was not masked during the test phase to avoid binaural
unmasking, which could cause additional, unwanted variability in the SRT-values. The SoRT was calculated by averaging the SNR of the last 15 trials, including a non-presented (imaginary)
22nd trial, of which the SNR was calculated based on the identification response of the final presented item. A SECREF result was considered reliable when the SD of the 15 trials used for
the calculation of the SoRT-value was < 2.5 dB SNR. The SECAPH presented antiphasic stimuli, i.e. with a phase difference of 180° between ears, in in-phase noise. This presentation mode
relied on binaural unmasking or Binaural Masking Level Differences (BMLD), which is an improvement of the SoRT or speech reception threshold in noise due to a phase difference of the stimuli
between both ears. BMLDs are reported to be poorer for listeners with all types of hearing loss than for NH controls, which makes the difference in performance between NH and HoH
participants larger30. For the SECAPH, the acclimatization phase was followed by two dichotic training phases with 21 trials and one dichotic test phase with 21 trials, as previous research
suggested that a longer training phase was needed when testing children dichotically31. The training and the test phases used the same adaptive procedure as described for the SECREF but with
a starting SNR of − 10 dB SNR and noise fixed at 70 dB SPL because a BMLD of ± 10 dB SNR was expected26,27,31. The SECAPH result and its reliability were calculated as described for the
SECREF. The SECFIX used two short binaural training phases with a variable number of trials (max. seven trials per phase) and two monaural test phases with a variable number of trials (max.
21 trials per ear). The noise was fixed at 65 dB SPL. The stopping rule calculated a preliminary proportion correct for each trial. The proportion-correct was compared to a predefined
proportion of 90%. The test was stopped when either the pass or fail proportion was higher than the predefined value or when the maximal number of trials was reached. The result was no
longer an SoRT but a pass/fail classification. The SNR used during the first training phase was − 4 dB SNR, and the SNR used during the second training phase was − 7.8 dB SNR, the optimal
cut-off value to differentiate between NH children and children with CHL > 30 dB HL and SNHL > 20 dB HL with the SECREF31. In the training phases, the stopping rule could only result
in an early fail result, and NH children who performed well would always complete the entire training needed to avoid motivation loss for children that do not hear any of the sounds at this
SNR but still give NH children enough training to proceed to the test phase. After the training phase, a monaural test phase was performed for each ear with the stopping rule described
above, but this time the test could result in both an early fail and an early pass. During the test phase, the SNR was again − 7.8 dB SNR, the optimal cut-off to differentiate between NH
children and children with CHL > 30 dB HL and SNHL > 20 dB HL as estimated in previous research31. The contralateral ear was not masked during the test phase to avoid binaural
unmasking, which could cause additional, unwanted variability in the SRT-values. PROTOCOL All children were tested in a quiet room (at home or in school) or an audio booth (at the hospital).
Noise floors in quiet rooms were not measured as the used headphones (RadioEar DD65) give enough damping (~ 30–40 dB SPL) to attenuate the average noise levels in quiet rooms (~ 30 dB SPL).
The total protocol (audiometry + two SEC versions + 5-min break) took 40 to 50 min. Most children started with the SEC tests unless the circumstances did not allow it. Every child did the
SECREF, combined with the SECFIX or the SECAPH. All SEC tests were done as a self-test, meaning the child performed the test autonomously. The order in which the SEC tests were done was
randomized, resulting in four possible sequences, named ‘RA’, ‘AR’, ‘RF’, and ‘FR’, which consist respectively of the SECREF and SECAPH, the SECAPH and SECREF, the SECREF and SECFIX, and the
SECFIX and SECREF. When the time was available, the protocol could be extended with the third test version that was not done yet. If, due to circumstances such as a time restriction, a
reliable second test was not possible, only one SEC version was done/included. The hearing thresholds (250–8000 Hz) were measured using the Hughson-Westlake method. If an AC threshold was
worse than 20 dB HL at one or more frequencies, the BC thresholds for those frequencies were measured. Masking was used according to standardized guidelines32. STATISTICAL ANALYSES
Statistical analyses were performed using R and R Studio33. For the general analyses and the analyses on the cultural dependence of the SEC, only the data of NH children was used. Values of
children/ears with a PTA0.5–4 kHz < 20dB HL but one or more thresholds worse than 20 dB HL (NH+) were not included in the analyses described below unless specified differently. The
analyses done with the data of children with NH+ were described separately in the last part of the paragraph of the statistical analyses section. GENERAL ANALYSES A possible age effect on
the SoRT-values obtained with the SECAPH was estimated with a simple linear model (LM) with 'age' as the independent variable and 'SoRT-value' as the dependent variable.
For the SECREF this effect was estimated with a Linear Mixed Effect Model (LMEM) as two values were obtained per person (left and right ear). The model included 'age' as the
independent variable, 'SoRT-value' as the dependent variable and 'ID' as the random effect. For the SECFIX, this effect was estimated with a mixed logistic regression
model with 'age' as the independent variable, ‘score’ on the SECFIX as the dependent variable and ID added as a random effect. The same type of model with 'sex' as the
independent variable was used to estimate the effect of ‘sex’ on the SoRT-values obtained with the SECREF, the SECAPH and SECFIX. If an age effect was present, 'age' was added as
an additional independent variable. Differences in SoRT-values on the SECAPH obtained in different sequences were estimated with LMs, with ‘SoRT-value’ as the dependent variable and
'sequence’ as the independent variable. For the SoRT-values obtained with the SECREF, an LMEM was used with the same variables, but 'ID' was added as a random effect, and the
sequences were grouped based on whether the SECREF was done first (RA & RF) or last in the sequence (FR or AR). For the SECFIX, a log-linear regression was used with ‘sequence' as
the independent variable, 'ID' as the random effect and ‘score’ on the SECFIX as the dependent variable. The analyses on the effect of ‘sequence’ did not include the results of the
extra tests done as an additional third test (see Protocol). CULTURAL- AND LANGUAGE-DEPENDENCE OF THE SEC Differences in SoRT-values on the SECREF and their SDs obtained in different
countries were estimated with an LMEM, with ‘SoRT-value’ or ‘SD’ as the dependent variable and ‘country’ as the independent variable, 'ID' as a random effect. If an age effect was
present, 'age' was added as the additional independent variable. The SD of the SoRT-values was used as a measure for the stability of the test. The same type of model with
'mother tongue' instead of 'country' as an independent variable was used to estimate the effect of mother tongue on the SoRT-values obtained with the SECREF.
Stimulus–response confusion matrices were made for every country with the values of the SECREF to estimate the familiarity of the sounds used in different countries. The overall recognition
coefficient was compared between countries using a chi-squared test. Differences between countries in specific diagonal scores of the confusion matrices per sound were analyzed with a
loglinear regression model with 'country' and 'sound' as independent variables and 'identification' as the dependent variable. SENSITIVITY AND SPECIFICITY OF
THE OPTIMIZED SEC-PROCEDURES. The correlation between the PTA0.5–4 kHz and the SoRT-values of the SECREF was determined with an LMEM with ‘SoRT-values’ as the dependent variable and
‘PTA0.5–4 kHz’ as independent variables. ‘ID’ was added as a random effect, and 'age' was added as an additional independent variable if an effect of age was present. The
correlation between the PTA0.5–4 kHz and the SoRT-values of the SECAPH was calculated with an LM with ‘SoRT-values’ as the dependent variable and ‘PTA0.5–4 kHz’ as the independent variable.
A possible interaction effect between the type of hearing loss and the PTA0.5–4 kHz on the SoRT-values of the SECREF was estimated with a LMEM including only the SoRT-values of the HoH
children with the interaction effect between ‘hearing loss type’ and ‘PTA0.5–4 kHz’ as independent variable and ‘SoRT-values’ as the dependent variable. ‘ID’ was added as a random effect,
and 'age' was added as an additional independent variable in case an age effect was present. For the SoRT-values of the SECAPH, the same variables were used in an MLM without ‘ID’
as a random effect. In this analysis, the results of the child with MHL in one ear and NH+ in the other were not considered, as the model does not allow single-value groups. Sensitivity and
specificity to detect hearing losses with a PTA0.5–4 kHz > 20dBHL, > 30dB HL, and > 40 dB HL with the SECREF and SECAPH were estimated with Receiver Operating Characteristic (ROC)
analyses, constructed for CHL and SNHL separately, and for CHL, SNHL and MHL together. ROC curves and the associated sensitivity and specificity were classified according to the principles
of Metz34. For the SECAPH, the hearing type of the worse ear was used to define the overall hearing. No independent analyses were done for MHL, as only a limited number of children with MHL
were tested. The assumptions of ROC analyses, namely that the measurement of interest is continuous with an independent diagnosis, that the state variable is independent of the measurement
of interest and that the cases are a random sample, were all met. Sensitivity and specificity to detect CHL > 30 dB HL or SNHL > 20 dB HL with the SECFIX were investigated as simple
percentages of correct classification as both values are factors. Symmetric and asymmetric hearing losses were considered together to determine optimal pass-fail criteria for both hearing
loss types. MINIMAL HEARING LOSS The results of children with NH+ were analyzed separately to get an overview of how the SEC captures these types of minimal hearing loss. The results of the
SECREF and SECFIX of children with NH+ could have been obtained by children with NH+ in one ear and a more severe hearing loss in the other ear. However, the better ear of these participants
was analyzed (the ear with NH+). Therefore, crossover hearing is unlikely to have influenced the results of the ears with NH+. The percentage of pass and fail results based on the ROC
analyses described above was calculated to analyze the results of the children in the NH+ group. Afterward, these children were divided into groups based on their results on the SECREF,
SECAPH, and SECFIX. Possible differences in the audiograms of children with fail results on each test were compared using t-tests. For the SECREF and the SECFIX, ears were considered
separately. For the SECAPH, the worst and the best threshold at a certain frequency were considered in separate groups. RESULTS The average SoRT-values per sequence for NH children for the
SECREF and the SECAPH are given in Fig. 3. Figure 3 does not include age as a variable, which results in slight deviations in the differences between the tests done in different sequences
from what is estimated with the statistical analyses. The average SoRT-values for NH children for the SECREF and the SECAPH were − 7.9 ± 2.4 dB SNR and − 14.4 ± 3.7 dB SNR, respectively. A
significant age effect was present on the results of NH on the SECREF (t (478.0) = − 5.9, _p_ < 0.001) but not on the SECFIX (z = 1.0, _p_ = 0.318) or on the SECAPH (t (3.7, 223) = − 1.3,
_p_ = 0.208). The regression coefficients indicated that the SoRT-values of the SECREF decreased with ± 0.7 dB SNR per year. No effect of sex was present on the results of the SECREF (t
(411.7) = − 0.3, _p_ = 0.783), on the SECAPH (t (3.8, 192) = − 1.9, _p_ = 0.066) or on the SECFIX (z = − 0.5, _p_ = 0.617). For the SECREF and the SECFIX, results estimated in different
sequences did not differ significantly (SECREF: t (488,1) = 0.07, _p_ = 0.942, SECFIX: z = 1.9, _p_ = 0.056), but for the SECAPH, a significant difference of 2.0 dB SNR was present between
the SECAPH done first and the SECAPH done second (t (3.5, 221) = − 4.3, _p_ < 0.001). CULTURAL- AND LANGUAGE-DEPENDENCE OF THE SEC The average SoRT-values per country on the SECREF are
given in Table 2 and shown in Fig. 4. The average values given in Table 2 and shown in Fig. 4 are not taking age into account, which results in slight deviations from the differences between
the tests done in different countries estimated with the statistical analyses. Significant differences were determined between SoRTs collected in Flanders and Israel. SoRTs on the SECREF
collected in Israel were significantly poorer than SoRTs collected in Flanders (t (484.8) = 2.3, _p_ = 0.021). The difference, corrected for age, was 0.8 dB SNR. None of the other countries
showed significant differences with respect to the SoRTs measured (p-values between 0.073 and 0.777). No differences between countries were present in the average SD of the SoRT-values
(p-values between 0.096 and 0.666), which was 1.7 ± 0.3 dB SNR in all countries. No difference was determined between children with a different mother tongue compared to children with the
country's official language as their mother tongue (t (473.7) = − 1.0, _p_ = 0.313). Figure 5 shows the confusion matrices per country. The average across-sound recognition coefficient
was 74 ± 5%. The bells were recognized correctly least often (67 ± 10%). The telephone was recognized most often (87 ± 3%). No significant differences were present in the sound-specific
recognition scores between countries (p-values between 0.057 and 0.903), except for the bells, which were significantly more difficult in Israel than in other countries (z (8339.4, 18,984) =
− 3.4, _p_ < 0.001). No significant differences were present between countries in the overall recognition coefficient (χ2 (6, N = 18,816) = 3.1, _p_ = 0.801). SENSITIVITY AND SPECIFICITY
OF THE OPTIMIZED SEC-PROCEDURES. The relation between the SoRT-values on the SECAPH and SECREF and the PTA0.5–4 kHz is visualized in Fig. 6. PTAs0.5–4 kHz were significantly related to the
SoRT-values obtained with the SECREF (r = 0.07, t (1169) = 9.1, _p_ < 0.001) and the SECAPH (r = 0.16, t (3.8, 311) = 7.3, _p_ < 0.001). No significant interaction effects were present
between the PTA0.5–4 kHz and the type of hearing loss on the SoRT-values obtained with the SECREF (p-values between 0.210 and 0.820) or the SECAPH (p-values between 0.282 and 0.924). The
area under the curve (AUC), optimal pass, fail criteria and sensitivity and specificity are given in Table 3. Both the SECREF and the SECAPH had very good sensitivity and specificity to
detect hearing losses > 40 dB HL. For milder SNHL, the sensitivity and specificity of both tests remained good. SoRT-values obtained with mild CHL showed more variation, visible in Fig.
6, and a slightly lower sensitivity and specificity for mild CHL was obtained (Table 3). The results of the SECFIX are visualized together with the SoRT-values of the SECREF in function of
the PTA0.5–4 kHz in Fig. 7. The SECFIX had a sensitivity and specificity of 71% to pick up the children with either CHL > 30 dB HL and children with MHL/SNHL > 20 dB HL, the hearing
loss degrees for which the cut-off was set initially. This was slightly higher than the sensitivity and specificity of the SECREF for the same hearing loss (Table 3). When comparing the
results of the SECREF and the SECFIX, an SoRT-value of − 7.1 dB SNR on the SECREF differentiated the best between a pass and a fail result on the SECFIX. Sixty-eight percent of the children
scoring poorer SoRT-values than − 7.1 dB SNR on the SECREF obtained a fail result on the SECFIX, and 76% of the children with SoRT-values lower than − 7.1 dB SNR on the SECREF, obtained a
pass result on the SECFIX. MINIMAL HEARING LOSS Of the 164 ears classified as NH+ tested with the SECREF, 84 (51%) had an SoRT on the SECREF = < − 7.8 dB SNR, the optimal cut-off SoRT
estimated to detect hearing loss > 20 dB HL. The SoRTs obtained in 80 ears (49%) were > − 7.8 dB SNR. Forty children with NH+ in their worse ear did the SECAPH. Twenty-eight children
(70%) had an SoRT = < − 13.3 dB SNR and 12 (30%) had an SoRT > − 13.3 dB SNR on the SECAPH, the optimal cut-off SoRT estimated to detect hearing loss > 20 dB HL with the SECAPH.
Sixty-one ears with NH+ were tested with the SECFIX, in which 21 (34%) a fail-result was obtained and in 40 (66%) a pass result was obtained the SECFIX. The average audiograms of these
children, divided into two groups based on their results on the different SEC tests, are given in Fig. 8. For the children who did the SECREF, a significant difference in the thresholds on
frequencies 250 Hz (t (142.1) = 2.8, _p_ = 0.016) and 500 Hz (t (135.4) = 2.4, _p_ = 0.019) was determined between the children with a pass and with a fail result on the SECREF. For the
SECFIX, only the threshold at 250 Hz differed significantly (t (44.7) = 2.3, _p_ = 0.029). No significant difference in pure tone thresholds was determined between the children with a pass
and a fail result on the SECAPH (p-values between 0.075 and 0.960). DISCUSSION The main objective of this study was twofold. The first objective was to investigate whether the test, designed
to be culture and language-independent, is truly cultural and language-independent. The second objective was to investigate the sensitivity and specificity of three versions of the SEC, a
closed-set tablet-based signal-in-noise self-test, to detect various degrees of CHL, SNHL and MHL in children at school entry. CULTURAL- AND LANGUAGE-DEPENDENCE OF THE SEC SoRT-values
collected in different countries did agree. The values collected in Israel were 0.8 dB SNR higher than the results collected in Flanders, which was a statistically significant difference.
However, compared to the measurement error, which is 1.3 dB SNR31, the difference is small and, therefore, clinically not relevant. The confusion matrices, constructed for different
countries, showed no differences in overall recognition percentage, indicating that the overall recognizability of the sounds is comparable in all countries. Differences in recognition
percentages of the individual sounds were minimal and these differences did not seem to cause clinically relevant changes in SoRT-values or overall recognition percentages. Therefore,
adapting the sounds seems unnecessary. No significant differences were determined in the stability of the test, and SoRT-values could be determined with a high stability of 1.3 dB SNR on
average in all countries. SENSITIVITY AND SPECIFICITY OF THE OPTIMIZED SEC-PROCEDURES. The original SEC with a monaural adaptive procedure before optimization showed high sensitivity and
specificity to detect different grades of CHL and SNHL (70–90%)31. For hearing loss > 30 dB HL, the sensitivity and specificity of the SECREF in the current research (70–90%) were
comparable with these previous findings. The sensitivity and specificity of the SECREF for CHL > 30 dB HL (0.67–0.68) were slightly lower than for SNHL (0.80–0.80). However, analyses
showed no difference in how different types of hearing loss affect the SoRT-values obtained with the SECREF. Therefore, this difference in sensitivity and specificity was most likely due to
differences in the distribution of the PTA0.5–4 kHz -values, in which the average PTA0.5–4 kHz of CHL > 30 dB HL (37.5 ± 7.3 dB HL) was lower than for SNHL/MHL (44.5 ± 10.9 dB HL). For
CHL, MHL and SNHL < 30 dB HL, the sensitivity and specificity were slightly lower than what was determined in previous research. Additionally, the pass-fail criteria for the SoRT-values
to detect these hearing losses were higher than determined by previous research31 indicating that the lower sensitivity and specificity was rather due to NH children scoring worse than
expected than due to children with hearing loss scoring better than expected. This may be because of the different circumstances in which the test was conducted. First of all, more children
were recruited and tested in hospitals during their already planned visits to the ENT department. It is not unlikely that these children, even though their audiograms were within normal
limits, still experienced some hearing difficulties related to the reason for which they initially had their appointments in the ENT department. Moreover, some children were recruited in a
private practice for pediatric audiology that sees a lot of children with learning problems in school, which could have complicated the test. As too little quantitative data was collected on
the performance of children with developmental disabilities and learning differences to give a substantiated opinion about the usage of the SEC for these children, and this study did not
perform any follow-up assessment of the children with pure tone thresholds within normal limits who scored worse than expected on the SEC tests, no conclusion can be made about the reason
for their deviating results. Moreover, it is important to note that a normal audiogram does not always mean that functional hearing is normal as well. Therefore, diagnostics and follow-up
after a failed SPIN or signal-in-noise test should go beyond performing pure tone audiometry. For the SECAPH, the sensitivity and specificity were similar to slightly lower than the
sensitivity and specificity of the SECREF. This contrasts with previous research, where the sensitivity and specificity were higher for antiphasic procedures than for diotic procedures26. A
possible reason why we did not find higher sensitivity and specificity with the SECAPH than with the SECREF could be the long training needed for the SECAPH when done by children. Previous
research with the SEC indicated that children needed more training when performing an antiphasic test than a monaural test31. Therefore, in this study, an extra training phase with 21 trials
was provided before the test phase. However, our results indicate that children who performed the SECREF before the SECAPH still scored better on the SECAPH, showing that the extra training
phase was still insufficient. As the results obtained with the SECAPH as the first in the sequence were 2 dB SNR worse than those obtained with the SECAPH done second in the sequence, extra
variance was induced, possibly reducing the sensitivity and specificity. However, even if higher sensitivity and specificity would be obtained when only considering SoRT-values of SECAPH
performed as the second test in the sequence, this is somewhat irrelevant as it would practically be almost impossible to perform an even longer training phase for the SECAPH when using it
as a systematic screening test. Previous research with antiphasic procedures done with adults does not report the length of the training done26,27. Therefore, it is unclear whether longer
training is only needed when testing children. Another possible reason for the high number of children with normal audiograms but with high SoRTs on the SECAPH is the development of binaural
hearing during childhood35. Research shows that the binaural processing of temporal fine structure is not fully developed in children aged 5 years, 6 months to 9 years, 4 months, which can
limit the binaural unmasking needed to pass the SECAPH35. Developmental effects on the SoRT-values of the SECAPH can cause additional variance in these results, which can lower the
sensitivity and specificity of the test for children, explaining why an antiphasic procedure is less suitable for children than for adults. The sensitivity and specificity of the SECFIX to
detect CHL > 30 dB HL and MHL and SNHL > 20 dB HL were slightly higher than the sensitivity of the SECREF and the SECAPH for the same type of hearing loss. However, when comparing the
results on the SECREF and the SECFIX, it is important to notice that, even though the SECFIX presented all the sounds at an SNR of − 7.8 dB SNR, the best cut-off SoRT to differentiate with
the SECREF between children obtaining a pass and a fail result on the SECFIX, was − 7.1 dB SNR. This indicates that the SECFIX was slightly more difficult than the SECREF. A possible reason
is that when a child has an SoRT close to the SNR used for the SECFIX, all the sounds played were challenging and required full attention. Moreover, the SECFIX allows for very few accidental
mistakes, as when one sound is answered wrongly, the chance to get a pass result already drops by at least 5% (1/21). Therefore, the SECFIX can be more sensitive to attention dwells, which
can result in more fail results, especially for the children with SoRTs close to the SNR used in the SECFIX. Within this research, supplementary analyses were performed on children with
PTA0.5–4 kHz < 20 dB HL but with one or more elevated thresholds. In our research, around 30–50% of these children failed on the different versions of the SEC when using the optimal
cut-offs to differentiate NH children from children with mild CHL, SNHL or MHL ≥ 20 dB HL, which indicates functional hearing problems. For the SECREF, this percentage was higher than the
percentage of fail results in the NH group when using the same cutoff-value (NH+: 49%, NH: 42%), for the SECAPH and the SECFIX, this percentage was in line with the percentage of fail
results obtained for the NH group when using the same cutoff-value (± 30%). The frequencies at which the thresholds were elevated did not seem to be related to whether or not they failed the
SEC tests. The relation determined between minimal hearing loss and functional hearing problems aligns with previous research showing that even minimal hearing loss can affect functional
hearing abilities6, which, again, favors qualitative follow-up after failing a functional hearing test, even though the problems determined with only pure tone audiometry are minimal.
CONCLUSION High sensitivity and specificity of the SECREF, SECFIX and SECAPH for mild hearing loss were determined. 30–50% of the children with one or more elevated thresholds, but a
PTA0.5–4 kHz within normal limits were detected with the SEC tests as well. For the SECAPH, children seemed to need more than twice the length of the training needed for monaural tests
before stable SoRT-values could be obtained. For that reason, this research favors the use of monaural test procedures for children, such as the SECREF and the SECFIX. Previous research
showed a significantly shorter test duration for the SECFIX than for the SECREF31. Therefore, the SECFIX can be particularly useful for screening children when test efficiency is of major
importance, while the SECREF can be useful when an SoRT-value needs to be obtained. Differences determined between countries were negligible, indicating cultural and language independence.
Therefore, the SEC has great potential to be used as an international hearing screening test for young children at school entry, regardless of the resources available to develop and
implement hearing screening programs. Consequently, the SEC can assist in the early detection of late-onset, acquired or progressive hearing loss in children internationally. DATA
AVAILABILITY The data that support the findings of this study are available from the corresponding author, E.V.d.B., upon reasonable request. REFERENCES * Butcher, E., Dezateux, C.,
Cortina-Borja, M. & Knowles, R. L. Prevalence of permanent childhood hearing loss detected at the universal newborn hearing screen: Systematic review and metaanalysis. _PLoS ONE_ 14,
1–21 (2019). Article Google Scholar * Fortnum, H., Summerfield, A. Q., Marshall, D. H., Davis, A. C. & Bamford, J. M. Prevalence of permanent childhood hearing impairment in the United
Kingdom and implications for universal neonatal hearing screening: questionnaire based ascertainment study. _BMJ_ 323, 1–6 (2001). Article Google Scholar * Bess, F. H., Dodd-Murphy, J.
& Parker, R. A. Children with Minimal sensorineural hearing loss; Prevalence, educational performance, and functional status. _Ear Hear._ 19, 339–354 (1998). Article CAS PubMed Google
Scholar * Porter, H., Sladen, D. P., Ampah, S. B., Rothpletz, A. & Bess, F. H. Developmental outcomes in early school-age children with minimal hearing loss. _Am. J. Audiol._ 22,
263–271 (2013). Article PubMed Google Scholar * Winiger, A., Alexander, J. & Diefendorf, A. Minimal hearing loss: from a failure-based approach to evidence-based practice. _Am. J.
Audiol._ 25, 1–15 (2016). Article Google Scholar * Moore, D. R., Zobay, O. & Ferguson, M. A. Minimal and mild hearing loss in children._Ear Hear._ 41(4), 720–732.
https://doi.org/10.1097/AUD.0000000000000802 (2020). Article PubMed PubMed Central Google Scholar * Briscoe, J., Bishop, D. V. M. & Norbury, C. F. Phonological processing, language,
and literacy: A comparison of children with mild-to-moderate sensorineural hearing loss and those with specific language impairment. _J. Child Psychol._ 42, 329–340 (2001). Article CAS
Google Scholar * Lewis, D. E., Valente, D. L. & Spalding, J. L. Effect of minimal/mild hearing loss on children’s speech understanding in a simulated classroom. _Ear Hear._ 36, 136–144
(2015). Article PubMed PubMed Central Google Scholar * Yoshinaga-itano, C., Coulter, D. & Thomson, V. Developmental outcomes of children with hearing loss born in Colorado hospitals
with and without universal newborn hearing screening programs. _Semin. Neonatal._ 6, 521–529 (2001). Article CAS Google Scholar * McCann, D. C. _et al._ Reading and communication skills
after universal newborn screening for permanent childhood hearing impairment. _Arch. Dis. Child._ 94, 293–297 (2009). Article CAS PubMed Google Scholar * Kennedy, C. _et al._ Language
ability after early detection of permanent childhood hearing impairment. _Community Ear Hear. Health_ 4, 9 (2007). Article Google Scholar * Pimperton, H. & Kennedy, C. R. The impact of
early identification of permanent childhood hearing impairment on speech and language outcomes. _Arch. Dis. Child._ 97, 648–653 (2012). Article PubMed Google Scholar * Cupples, L. _et
al._ Spoken language and everyday functioning in 5-year-old children using hearing aids or cochlear implants. _Int. J. Audiol._ 57, S55–S69 (2018). Article PubMed Google Scholar * Yong,
M. _et al._ Cost-effectiveness of school hearing screening programs: A scoping review. _Am. J. Otolaryngol. Head Neck Med. Surg._ 162, 826–838 (2019). Article Google Scholar * World Health
Organization. Hearing screening: considerations for implementation. In _Licence: CC BY-NC-SA 3.0 IGO_ (2021). * Sharma, R. _et al._ An economic evaluation of Australia’s Newborn hearing
screening program: A within-study cost-effectiveness analysis. _Ear Hear._ 43, 972–983 (2022). Article PubMed PubMed Central Google Scholar * Neumann, K., Mathmann, P., Chadha, S.,
Euler, H. A. & White, K. R. Newborn hearing screening benefits children, but global disparities persist. _J. Clin. Med._ 11, 271 (2022). Article PubMed PubMed Central Google Scholar
* Wouters, J. _et al._ EFAS Working Group on school age hearing screening. In _EFAS Working Group on school age hearing screening_ (2017). * Mehra, S. & Eavey, R. D. The epidemiology of
hearing impairment in the United States: Newborns, children, and adolescents. _Otolaryngol. Neck Surg._ 140, 461–472 (2009). Article Google Scholar * Fletcher, H. & Galt, R. H. The
perception of speech and its relation to telephony. _J. Acoust. Soc. Am._ 22, 89–151 (1950). Article ADS Google Scholar * French, N. R. & Steinberg, J. C. Factors governing the
intelligibility of speech sounds. _J. Acoust. Soc. Am._ 19, 90–119 (1947). Article ADS Google Scholar * Denys, S. _et al._ Language-independent hearing screening based on masked
recognition of ecological sounds. _Trends Hear._ 23, 1–16 (2019). Google Scholar * Smits, C., Kapteyn, T. S. & Houtgast, T. Development and validation of an automatic speech-in-noise
screening test by telephone. _Int. J. Audiol._ 43, 15–28 (2004). Article PubMed Google Scholar * Smits, C., Goverts, S. & Festen, J. M. The digits-in-noise test: Assessing auditory
speech recognition abilities in noise. _J. Acoust. Soc. Am._ 133, 1693–1706 (2013). Article ADS PubMed Google Scholar * Smits, C. Improving the efficiency of speech-in-noise hearing
screening tests. _Ear Hear._ 38, e386–e388 (2017). Google Scholar * de Sousa, K. C., Swanepoel, D. W., Moore, D. R. & Myburgh, H. C. Improving sensitivity of the digits-in-noise test
using antiphasic stimuli. _Ear Hear._ 41, 442–450 (2020). Article PubMed PubMed Central Google Scholar * Smits, C., Watson, C. S., Kidd, G. R., Moore, D. R. & Goverts, S. T. A
comparison between the Dutch and American- English digits-in-noise (DIN) tests in normal-hearing listeners. _Int. J. Audiol._ 55, 358–365 (2016). Article PubMed Google Scholar * Plomp, R.
Auditory handicap of hearing impairment and the limited benefit of hearing aids. _J. Acoust. Soc. Am._ 63, 533–549 (1978). Article ADS CAS PubMed Google Scholar * Levitt, H.
Transformed up-down methods in psychoacoustics. _J. Acoust. Soc. Am._ 49, 467–477 (1971). Article ADS Google Scholar * George, E. L. J., Festen, J. M. & Goverts, T. S. Effects of
reverberation and masker fluctuations on binaural unmasking of speech. _J. Acoust. Soc. Am._ 132, 1581–1591 (2012). Article ADS PubMed Google Scholar * Van den Borre, E. _et al._
Language-independent hearing screening—Increasing the feasibility of a hearing screening self-test at school-entry. _Trends Hear._ 26, 1–15 (2022). Google Scholar * Perkins, E. _et al._
Further evidence for the expansion of adult cochlear implant candidacy criteria. _Otol. Neurotol._ 42, 815–823 (2021). Article PubMed PubMed Central Google Scholar * RStudio. RStudio:
Integrated Development for R. (2020). * Metz, C. E. Basic principles of ROC analysis. _Semin. Nucl. Med._ VIII, 283–298 (1978). Article Google Scholar * Flanagan, S. A. _et al._
Development of binaural temporal fine structure sensitivity in children. _J. Acoust. Soc. Am._ 150, 2967–2976 (2021). Article ADS PubMed Google Scholar Download references
ACKNOWLEDGEMENTS The authors want to thank Karsten Plotz, Katharina Schmidt, and Andrea Decker from Pädaudiologie in Oldenburg (paezo), Germany, for data collection. FUNDING This work was
supported by the TBM-FWO Grant—Research Foundation- Flanders grant number (T002216N), Legaat Ghislaine Heylen (Tyberghein). Contributions from Germany for this paper were supported by the
governmental funding initiative SPRUNG of the Lower Saxony Ministry for Science and Culture, project “Data-driven health (DEAL)”. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of
Neurosciences, Research Group ExpORL, KU Leuven, Herestraat 49 Bus 721, 3000, Leuven, Belgium Elien Van den Borre, Sam Denys, Astrid van Wieringen & Jan Wouters * Center of Pediatric
Audiology, St Petersburg, Russia Gaziz Tufatulin * North-Western State Medical University Named After I.I.Mechnikov, St Petersburg, Russia Gaziz Tufatulin * Scientific Research Institute of
Ear, Nose, Throat and Speech, St Petersburg, Russia Gaziz Tufatulin * Department of Ear, Nose, and Throat, General Hospital Celje, Celje, Slovenia Lea Zupan * Department of
Otorhinolaryngology and Cervicofacial Surgery, University Medical Centre Ljubljana, Ljubljana, Slovenia Nina Božanić Urbančič * Faculty of Medicine, Department of Otorhinolaryngology,
University of Ljubljana, Ljubljana, Slovenia Nina Božanić Urbančič * Department of Communication Sciences and Disorders, University of Haifa, Haifa, Israel Limor Lavie * Institute of Hearing
Technology and Audiology, Jade University of Applied Sciences, Oldenburg, Germany Inga Holube * Audiology Group, Department of Neuromedicine and Movement Sciences, Norwegian University of
Science and Technology, Trondheim, Norway Vinay Swarnalatha Nagaraj * Department of Audiology, Faculty of Health Science, Hacettepe University, Ankara, Turkey Emre Gurses * Department of
Otorhinolaryngology-Head and Neck Surgery, Multidisciplinary University Center for Speech-Language Pathology and Audiology, University Hospitals of Leuven, Leuven, Belgium Sam Denys Authors
* Elien Van den Borre View author publications You can also search for this author inPubMed Google Scholar * Gaziz Tufatulin View author publications You can also search for this author
inPubMed Google Scholar * Lea Zupan View author publications You can also search for this author inPubMed Google Scholar * Nina Božanić Urbančič View author publications You can also search
for this author inPubMed Google Scholar * Limor Lavie View author publications You can also search for this author inPubMed Google Scholar * Inga Holube View author publications You can also
search for this author inPubMed Google Scholar * Vinay Swarnalatha Nagaraj View author publications You can also search for this author inPubMed Google Scholar * Emre Gurses View author
publications You can also search for this author inPubMed Google Scholar * Sam Denys View author publications You can also search for this author inPubMed Google Scholar * Astrid van
Wieringen View author publications You can also search for this author inPubMed Google Scholar * Jan Wouters View author publications You can also search for this author inPubMed Google
Scholar CONTRIBUTIONS This research was an initiative from the EFAS Working Group for School Hearing Screening. KU Leuven (E.V.d.B., S.D., A.v.W. and J.W.) had a leading role in this
project. All other authors collected a significant amount of data and participated and contributed to monthly meetings discussing the project and preliminary results. E.V.d.B. conducted the
statistical analyses and wrote the manuscript. All authors have reviewed the analyses and the final manuscript. CORRESPONDING AUTHOR Correspondence to Elien Van den Borre. ETHICS
DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims
in published maps and institutional affiliations. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits
use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the
Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless
indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory
regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Van den Borre, E., Tufatulin, G., Zupan, L. _et al._ A language-independent hearing
screening self-test at school-entry. _Sci Rep_ 14, 2582 (2024). https://doi.org/10.1038/s41598-024-53026-y Download citation * Received: 06 July 2023 * Accepted: 26 January 2024 *
Published: 31 January 2024 * DOI: https://doi.org/10.1038/s41598-024-53026-y SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link
Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
