5 things to know about the alzheimer’s drug aducanumab
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

Insurers are still deciding whether to cover aducanumab. Medicare would likely bear the biggest burden, since most of the 6.2 million Americans living with Alzheimer's disease are 65
and older. If just 500,000 beneficiaries went on the drug, total spending for aducanumab in one year would be nearly $29 billion, a Kaiser Family Foundation (KFF) analysis found. That amount
“far exceeds spending on any other drug” covered under Medicare Part B (which accounts for prescription drugs given in a doctor's office or hospital outpatient setting) or Part D
(prescription drugs you can take yourself), the KFF report states. “To put this $29 billion amount in context, total Medicare spending for all Part B drugs was $37 billion in 2019,” the
authors add. If 1 million beneficiaries receive aducanumab, spending will exceed $57 billion a year. Even if Medicare takes on aducanumab, patients, including those with supplemental
insurance, could be left with thousands of dollars in out-of-pocket expenses. And other factors will likely add to that bill, including imaging scans. Patients in the clinical trials
underwent positron emission tomography (PET) scans to establish evidence of the amyloid plaques that the drug targets, and these scans are often not covered by insurance. Routine MRIs are
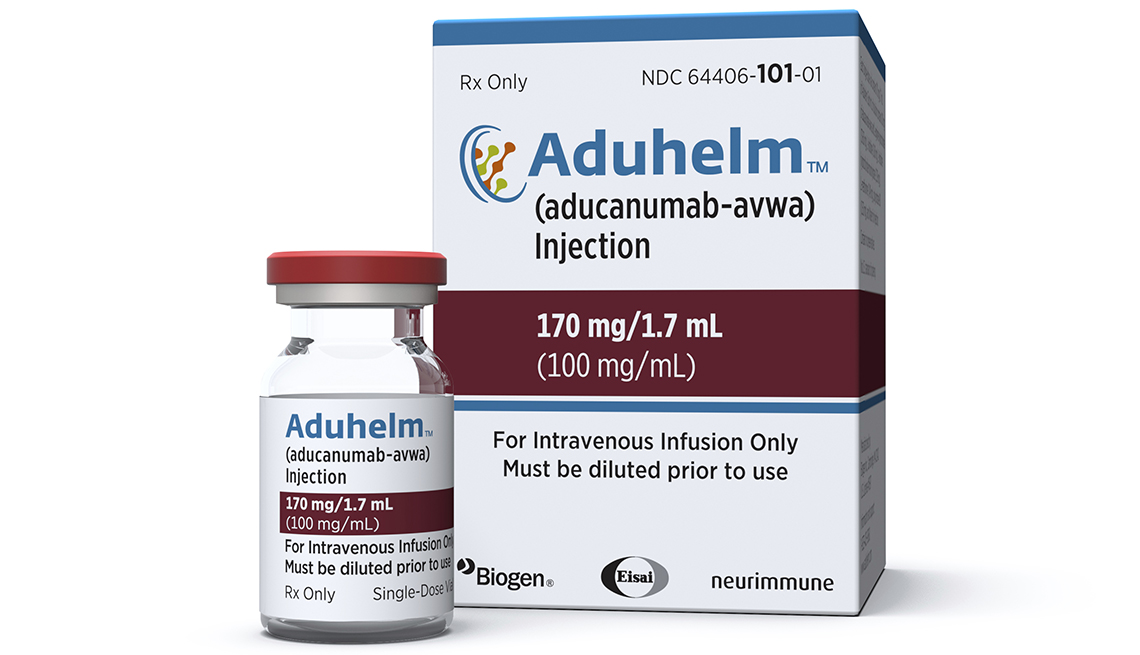
also needed to monitor for side effects. 5. ADUCANUMAB CAN COME WITH SIDE EFFECTS … _But are the risks worth it for a drug that still needs to prove its effectiveness?_ Like all drugs,
aducanumab can come with side effects. The most common observed during clinical trials were brain swelling and tiny brain bleeds. Headaches, falls, diarrhea and confusion were also reported.
In most cases, these microscopic brain bleeds are asymptomatic, “but they need to be closely monitored,” Galvin says. The drug's label calls for MRIs before the seventh infusion and
12th infusion to do just that. If the bleeds go undetected and worsen, they could lead to cognitive complications. "These are the types of questions that I think a patient and their
loved ones should think about and consider and discuss with their providers to determine whether Aduhelm is the right choice for them,” Galvin says about the risks. BOTTOM LINE: IT'S
GOING TO BE ‘CASE-BY-CASE’ The excitement that patients and their loved ones are feeling in light of aducanumab's approval is understandable, but it's going to require “a very
frank discussion” about the risks, the costs, the commitment and the clinical trial data before anything is prescribed, Isaacson warns. “The approach I've been taking is that each
decision about whether or not to offer this as a treatment has to be made on a case-by-case basis,” he adds. Another option for people with Alzheimer's disease is to consider enrolling
in a clinical trial testing another anti-amyloid drug — and there are several, some of which are producing promising data, Karlawish adds. This is also a decision that patients should make
with their doctors. And when it comes to scheduling these conversations? “Patients have to have patience, family members have to have patience,” Isaacson says. “This is new. We're all
still trying to figure it out together.”
