Dna diagnostics of the marfan syndrome: application of amplifiable polymorphic markers
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT The diagnosis of Marfan syndrome (MFS) is still based on careful clinical examination. There are, however, many factors creating problems in the firm establishment of the correct
diagnosis. After the identification of the defective gene in MFS, fibrillin 1 (FBN1), several mutations in this gene have been reported. Since so far all but one of the mutations in FBN1
have been family specific, a common diagnostic DNA test for all MFS patients is not to be expected in the near future. Here, we have utilized four polymorphic markers in the diagnostics in
MFS families from different populations. Two of the markers, FBN1a and a novel FBN1b, are intragenic markers of FBN1 and two others, D15S103 (G113) and CYP19, are very close to and most
probably flank FBN1. The combined use of the multiallelic markers proved highly useful in MFS diagnostics providing informativeness in all analysed families. You have full access to this
article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS CLINICALLY RELEVANT VARIANTS IN A LARGE COHORT OF INDIAN PATIENTS WITH MARFAN SYNDROME AND RELATED DISORDERS
IDENTIFIED BY NEXT-GENERATION SEQUENCING Article Open access 12 January 2021 UNSUSPECTED SOMATIC MOSAICISM FOR _FBN1_ GENE CONTRIBUTES TO MARFAN SYNDROME Article Open access 25 January 2021
AN INTEGRATED CLINICAL AND MOLECULAR STUDY OF A COHORT OF TURKISH PATIENTS WITH MARFAN SYNDROME HARBORING KNOWN AND NOVEL _FBN1_ VARIANTS Article 22 January 2021 INTRODUCTION Marfan
syndrome (MFS) is one of the most common genetic disorders of the connective tissue with a prevalence of about 1/10,000 [1]. It is inherited as an autosomal dominant trait and about 15–30%
of the patients represent sporadic cases [2, 3]. MFS patients have abnormalities in their skeletal, cardiovascular and ocular systems. Skeletal manifestations include a tall stature,
arachnodactyly, dolichostenomelia, anterior chest deformity, vertebral column deformity and joint laxity. Ocular findings consist of lens dislocation, myopia, corneal flatness and increased
axial globe length. The most severe and often fatal manifestations are found in the cardiovascular system. They include dilation of the ascending aorta, aortic dissection, mitral valve
prolapse and regurgitation of mitral and aortic valves [2]. Although no specific therapy exists for MFS it is of great importance to confirm or firmly exclude the MFS diagnosis of the family
members of patients as early as possible because of the potential fatal complications of the disease. At present, diagnosis is still based on thorough clinical examination, including
measurement of body proportions, echocardiography of the aorta, slit-lamp ophthalmological evaluation and a chest radiograph [2]. A complete family history is also an essential part of the
diagnosis. The problem is that in some cases the manifestations are not evident until early adolescence and although penetrance is close to complete, the clinical expression of the disease
varies greatly between different families and also among the affected members of a single family [2, 4]. Furthermore, many single clinical features of MFS can also occur in the general
population and, by chance, two of them together [2]. Thus, even an experienced clinician cannot always be 100% sure about diagnosis of young family members if the patients demonstrate only
some features of MFS. Therefore, there is an absolute need for a more accurate diagnostic test especially for individuals with affected relatives. Recently, independent data obtained both
from the immunohistochemical analyses of the fibroblasts of MFS patients and from linkage analyses in MFS families have demonstrated that the defective gene in MFS encodes fibrillin, an
essential component of extracellular-matrix microfibrils [5–7]. To date several mutations in the gene coding for fibrillin (FBN1) have been published and it seems that every family carries a
unique mutation [8–13, 28]. The possibility of locus heterogeneity of the disease still exists and obligatory recombination events between a Marfan-like disorder and polymorphisms in and
close to the FBN1 gene have actually been reported in a large French family [14]. Immunofluorescence studies of cultured fibroblasts and skin sections of MFS patients using monoclonal
antibodies against fibrillin have revealed that the amount of fibrillin microfibrils in these samples is reduced [6]. Therefore, immunofluorescence analysis could be helpful in diagnostis,
but this method has not proven to be sufficiently sensitive or specific. Consequently, a definite need exists for a more specific diagnostic test for MFS, and the discovery of the MFS gene
has actually raised high hopes for a DNA test applicable in MFS families. Due to the high degree of heterogeneity in MFS mutations such a test must rely on polymorphic markers inside the
FBN1 gene or tightly linked to it. We report here a novel intragenic polymorphism of the FBN1 gene and the diagnostic use of DNA genotypes in MFS families from different Caucasian
populations. Four amplifiable polymorphisms, two intragenic to FBN1 [15], and two in the vicinity of this gene, D15S103 (G113) [16] and CYP19 [17], were analysed to build up the genotypes
which were informative in all analysed families, and facilitated early diagnosis of MFS with relatively high certainty. MATERIALS AND METHODS The family material consisted of 15 unrelated
MFS families from Finland, Belgium, Sweden, Switzerland, the United Kingdom and the USA. The total number of affected individuals was 82. The average family size was 11 individuals and there
were three or more affected individuals in every family. All affected individuals fulfilled the commonly used criteria for MFS [3]. Genomic DNA was extracted by standard procedures from
peripheral blood leucocytes [18]. DNA samples were amplified using primers specific for the polymorphisms: (1) FBN1a: 5′-CCTGGCTACCATTCAACTCCC-3′ and 5′-GAGTACATAGAGTGTTTTAGGG-3′ [15]; (2)
FBN1b: 5′-GACATTAACGAGTGTGAAACCC-3′ and 5′-CACATCTGTAGGAGCCATCAGT-3′ (5′ end biotinylated); (3) D15S103 (G113): 5′GTTCAAAAGGCTCATCATGTAGC-3′ and 5′-TTCCTGAGTCCTTATAGCTTCCA-3′ [16], and (4)
CYP19: 5′-GCAGGTACTTAGTTAGCTAC-3′ and 5′-AGTGAGCCAAGGTCGTGAG-3′ [17]. PCR was performed in a volume of 50 °l with 10 ng of template DNA, 1 µ_M_ primers, 0.2 m_M_ each of dATP, dCTP, dGTP and
dTTP, supplemented with 50 m_M_ Tris-HCl, pH 8.8, 15 m_M_ (NH4)2sO4 1.5 m_M_ MgCl2, 0.1% Tween 20, 0.01% gelatin and 0.8 U _Thermus aquaticus_ DNA polymerase (Promega). In the case of
FBN1a, D15S103 and CYP19, 1 µCi of [±-32P]dGTP (3,000 Ci/mmol; Amersham) was added to the reaction. PCR was carried out in a programmable heating block (Techne PHCI) using the following
programmes: FBN1a: 95°C 1 min, 58°C 1 min and 72°C 2 min; FBN1b and D15S103: 95°C 1 min, 60°C lmin and 72°C 1 min; CYP19: 94°C 30s, 5 5° C 30 s and 72° C 1 min; each cycle was repeated 30
times. The alleles of FBN1a, D15S103 and CYP19 were identified after amplification and separation of radio-labelled fragments by electrophoresis on a 5% denaturing Polyacrylamide sequencing
gel. The gel was fixed in 10% acetic acid and 10% methanol solution for 30 min, dried and exposed to X-ray film (Kodak, X-omat). The novel biallelic T/C polymorphism of FBN1, FBN1b, was
identified using the solid-phase mini-sequencing method under conditions previously described [19, 20]. The DNA fragment spanning the polymorphic base pair was amplified using one
bio-tinylated and one unbiotinylated primer. The amplified biotinylated DNA was then attached to the streptavidin-coated microtitre well and denaturated in alkali. A mini-sequencing primer
(5′-ACCCCTGGGATCTGCATGAA-3′) and Taq polymerase were used to carry out a one-step sequencing reaction. In this reaction the primer anneals next to the polymorphic base pair and Taq
polymerase incorporates only one radiolabelled 3H-dNTP, in this case either 3H-dCTP or 3H-dTTP, at the site of the polymorphism. The elongated primer with the incorporated radioactivity was
eluted by denaturation at high pH. The radioactivity was measured in a liquid scintillation counter and the ratio of the radioactive C and T was determined to test whether the individual was
heterozygous or homozygous for the polymorphism [for details see ref. 20]. The distances of the markers D15S103 and CYP19 from the FBN1 gene locus and their orientation to each other were
calculated from the data on their segregation in the CEPH families using the program designed for CEPH, version 6.0. Only 18 of the 40 CEPH families were informative with FBN1 a and a
further analysis of these families was carried out with markers D15S103 and CYP19. Computer programs MLINK and LINKMAP of the Linkage Package Version 5 [21, updated by Dr. J. Ott] were
applied to perform the linkage analyses in our MFS families. The risk calculations were carried out with the risk calculation option of the MLINK program. RESULTS In order to test their
diagnostic value, we analysed four amplifiable polymorphisms inside or in the vicinity of the fibrillin gene on chromosome 15 and followed their segregation in 15 representative MFS families
from Finland, Belgium, Sweden, Switzerland, the United Kingdom and the USA. All the families had a history of MFS in more than one generation and at least three living affected individuals
could be analysed in each family. Two of the analysed polymorphisms are located inside the FBN1 gene and two others, D15S103 and CYP19, are reported to be located very close to the FBN1
locus [22]. One of the intragenic polymorphisms is a novel one, representing a biallelic T/C polymorphism in the coding region of the FBN1 gene and is localized −820 bp from the 5′ end of
the published cDNA sequence [23]. This polymorphism was originally found in the sequence analysis of this region from several individuals, and when the mini-sequencing technique was
established to detect this polymorphism the heterozygosity of this marker in our MFS families was 0.35 (table 1). The other analysed intragenic polymorphism is the previously reported
4-allele polymorphism with allele sizes averaging from 150 to 180 base pairs [15], localised inside the intron between nucleotides 896 and 897 according to the cDNA sequence by Maslen et al.
[23]. In our MFS family material and in CEPH families, the heterozygosity of the 4-allele marker was 0.34 (table 1). No obligatory recombination events were detected between the disease and
either of the intragenic markers or between the two intragenic markers in either CEPH or MFS families. Two multiallelic markers have been assigned to the immediate vicinity of FBN1 in the
CEPH consensus map [22]. D15S103 represents a 10-allele polymorphism, the sizes of the alleles varying between 235 and 289 base pairs. CYP19 is a 6-allele tetranucleotide repeat with allele
sizes ranging from 154 to 178 base pairs. The heterozygosities of D15S103 and CYP19 were 0.74 and 0.65, respectively (table 1). We analysed the co-segregation of these markers and the
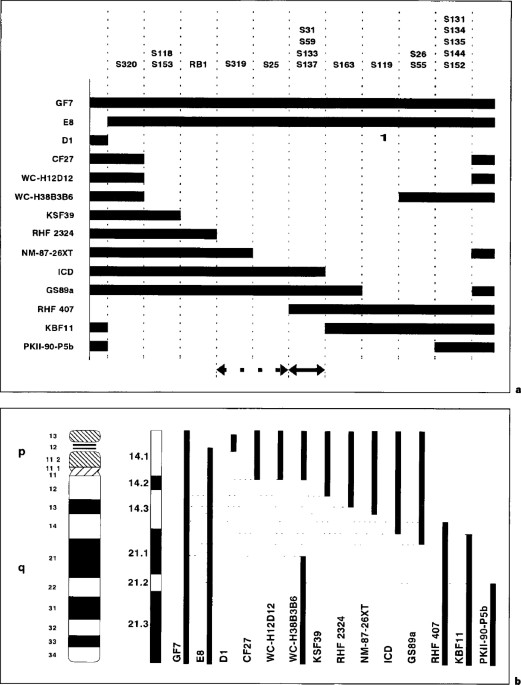
4-allele FBN1a intragenic polymorphism in CEPH families. The most likely order of these markers was cen-D15S103-FBN1a-CYP19-pter, the second-best order, cen-FBN1a-D15S103-CYP19-pter, was
6.4-fold less likely and all the other orders were over 1,000-fold less likely. In pairwise linkage analysis, D15S103 was assigned 2.7 cM from FBN1a and CYP19 3.3 cM from FBN1a, and in the
multipoint linkage analysis, assuming the order of the markers to be cen-D15S103-FBN1a-CYP19-pter, the corresponding distances were 3.2 and 4.7 cM (fig. 1). When the order of the markers was
assumed to be cen-FBN1a-D15S103-CYP19-pter the distances of D15S103 and CYP19 from FBN1a were 1.9 and 6.0 cM, respectively. In our MFS family material these polymorphisms were informative
as follows: FBN1a in 40%, FBN1b in 27%, D15S103 in 87% and CYP19 in 60% of the families (table 2). A family was considered as informative if at least half of the meioses were informative.
Consequently, in table 2 there are families which are marked as uninformative although a part of the family was fully informative. The combination of these four markers into a genotype and
segregation analyses in the 15 MFS families facilitated the follow-up of the MFS allele in each family. Examples of diagnostic application of these markers are demonstrated here in the case
of three families. The first case is a four-generation MFS family with a newborn boy (IV-1; fig. 2). The parents wanted to obtain information on the affection status of their son as early as
possible. The father (III-9) of the boy has classical MFS with a typical habitus, ectopia lentis and dilation of the ascending aorta. Both FBN1a and FBN1b were non-informative, but markers
D15S103 and CYP19 were informative, resulting in lod scores of 2.709 and 2.408 (θ = 0.000), respectively, in the pairwise analysis between each marker and MFS in this family. The information
of markers D15S103 and CYP19 suggested that the newborn boy had inherited the allele associated with MFS in all affected individuals of the family. The statistically calculated risk of the
newborn boy carrying the MFS allele was 99.9% assuming the order of the markers to be cen-D15S103-FBN1a-CYP19-pter and 98% with the order cen-FBN1a-D15S103-CYP19-pter. In genetic counselling
we informed the parents, the risk of incorrect prediction being less than 5%, taking into consideration laboratory errors. The second example is a three-generation MFS family in which there
was uncertainty about the diagnoses of the children in the third generation due to the variable expression of the disease in the family (fig. 3). The family was informative with marker
CYP19 and partially with marker FBN1b. The two-point lod scores obtained between each marker and MFS were 1.203 for CYP19 and 0.602 for FBN1b (θ = 0.000) when the status of the children,
whose diagnosis was uncertain (III-1, III-2, III-3, III-6, III-7, III-8 and III-9) was marked as ‘not known’. These lod scores support the linkage of MFS to chromosome 15 markers in the
family. The analysis of the CYP19 genotype suggested that children III-3, III-4, III-5, III-6 and III-7 had inherited the allele associated with MFS and children III-l, III-2, III-8 and
III-9 had inherited the other allele from their respective affected parent. Segregation of marker FBN1b could be followed from individuals II-3 and II-4 to their children, III-4, III-5 and
III-6, and suggested that all the children had inherited the allele associated with MFS, just as the analysis of CYP19 had indicated. The statistically calculated risks of being affected,
assuming the order of markers to be cen-D15S103-FBN1a-CYP19, among the children with the allele associated with MFS were 96% (III-3, III-6, III-7) and the corresponding risk of the children
who had inherited the other allele from their affected parent (III-l, III-2, III-8, III-9) was very low, only 4%. When the order of markers was assumed to be cen-FBN1a-D15S103-CYP19 the
risks to the children were 92% (III-3, III-6, III-7), and 8% (III-l, III-2, III-8, III-9). In this family we actually identified a specific mutation resulting in a 366-bp deletion in the
fibrillin cDNA in affected individuals [9]. Direct analysis of this mutation confirmed the diagnoses of uncertain cases and was in complete agreement with the results obtained from the
segregation analysis of the two informative polymorphic markers. The third example represents a small MFS family with affected individuals in three generations (fig. 4). All of our four
markers were informative in the family and two-point lod scores between each marker and MFS were 0.806 for D15S103, 0.648 for FBN1b, 0.839 for FBN1a and 0.824 for CYP19 (θ = 0.000) which are
quite low because of the small size of the family. In this family also the markers clearly co-segregate with the disease in the family, although the small size of the family sets some
restrictions on definitive ascertainment of a diagnosis. DISCUSSION Nowadays, diagnosis for MFS is based on careful clinical examination and is often hampered by the highly variable
expression of the disease and the fact that the manifestations sometimes do not occur until early adolescence [2]. Since the complications of MFS, such as rupturing of the aortic wall, can
be life-threatening, presymptomatic identification of the patients is extremely important. When diagnosis is made in a presymptomatic state of the disease the patient can be followed more
accurately and the major complications more efficiently prevented. Most, if not all, classical Marfan as well as ectopia lentis cases are caused by mutations in the FBN1 gene on chromosome
15 [24, 29]. On the other hand, other disorders sharing features with MFS such as congenital contractural arachnodactyly, annulo-aortic ectasia and mitral-valve prolapse have not been
unequivocally assigned to this chromosomal region or have been assigned to a fibrillin gene in another chromosome [24]. To date, specific mutations in the FBN1 gene have been identified in
only 10–20% of analysed MFS patients [8–13, 28]. The FBN1 gene is large and complex, consisting of numerous repetitive regions and, additionally, the structure of the 5′ end of the gene is
still unknown [23]. All these features create technical problems for the identification of the gene defects found in the heterozygote form in MFS patients. Since all but one reported MFS
mutations have been family specific and are found spread over the entire cDNA, this rules out the possibility of a generally applicaple diagnostic DNA test to identify MFS patients. In
families with several affected individuals, diagnosis can, however, be made quite reliably by identification of the MFS allele using polymorphisms inside and in the vicinity of the FBN1
gene. In this study we tested the diagnostic value of four such polymorphic markers in representative families from several populations. The DNA genotypes formed by the four studied
polymorphic markers proved to be highly valuable in the diagnosis of the individual MFS families. In our family material at least one of the markers was informative in each family (table 2).
The markers could be applied to confirm the diagnoses in presymptomatic children, as in our first example (fig. 2) and in young subjects presenting a mild phenotype resulting in diagnostic
problems, as our second example shows (fig. 3). These markers are of course also applicable to prenatal diagnosis in MFS families. Of the families we have described here in more detail the
first two (fig. 2, 3) represent ideal examples of the usefulness of polymorphic markers in MFS diagnostics. They are large families with several affected individuals. At least one of the
markers is informative, suggesting that the disease co-segregates with chromosome 15 markers, giving impressively high certainties in the risk calculations. Our third example represents a
family which is not optimal for this kind of diagnostic approach because of its small size and the small but still existing possibility of locus heterogeneity underlying MFS. Nontheless,
this family is applicable if the individuals are ready to accept a certain degree of uncertainty in the predicted risk. The advantage of the polymorphic markers in diagnostics as compared
with the immunofluorescence technique, which is used to detect the decreased amount of microfibrils [6], is the rapid analysis directly from blood samples; no skin biopsy or cell culture is
needed. The results of the marker analysis are easy to interpret even by inexperienced personnel, whereas experts are needed to detect abnormalities in immunofluorescence staining.
Additionally, marker analysis in families reveals precise individual risks, whereas the immunofluorescence test reveals a cellular phenotype which can also be caused by defects in genes
other than FBN1. On the other hand, the disadvantage of marker analysis is the requirement for DNA samples from several family members. In addition, the use of polymorphic markers in the
diagnostics of MFS does not eliminate the diagnostic problem in sporadic cases and in small families. In these cases, for the diagnostic analysis to be reliable, identification of the
mutation is necessary. The remaining possibility of locus heterogeneity in MFS must also be borne in mind; if another MFS locus exists, the segregation analysis of the polymorphic markers in
and around the fibrillin gene will lead to misdiagnosis. Technically, the analyses of these polymorphic markers are not very demanding, they are quite rapid to perform and are relatively
inexpensive. However, the electrophoresis-based identification of the amplified products is not always ideal for clinical laboratories. The solid-phase mini-sequencing method [20] applied
here to identify the biallelic FBN1b polymorphism is a prototype for DNA diagnostics suitable for clinical-laboratory use. No electrophoretic separation step is needed, the results are
obtained in numerical format and they unequivocally identify the heterozygous individuals. Additionally, the results are easy to store and the whole analysis can be easily automated. The
single biallelic polymorphism reported here is not alone informative enough for diagnostics but when more biallelic polymorphisms are found it will be possible to build up a diagnostic kit
to detect several intragenic polymorphisms simultaneously with the rapid and technically easy solid-phase mini-sequencing method. The use of polymorphic markers has previously been described
in prenatal diagnosis of osteogenesis imperfecta (OI), which, like MFS, is also highly heterogeneous in mutations [25]. Although the diagnosis of OI is complicated because of the two
disease loci it is possible to identify the OI allele with certainty especially in large OI families. To our knowledge, the present paper describes the first systematic trial aimed at DNA
diagnostics in MFS families, and the results show how a DNA test can considerably assist in the presymptomatic identification of patients. As expected, the multiallelic markers were the most
useful due to their high informativeness, but the combined use of several intragenic biallelic markers would also be quite applicable, especially due to the possibility for their rapid
identification by the solid-phase mini-sequencing. REFERENCES * McKusick VA: The defect in Marfan syndrome. Nature 1991;352:279–281 Article CAS Google Scholar * Pyeritz RE, McKusick VA:
The Marfan syndrome: Diagnosis and management. N Engl J Med 1979;300:772–777 Article CAS Google Scholar * Brighton P, de Paepe A, Danks D, Finidori G, Gedde-Dahl T, Goodman R, Hall JG,
Hollister DW, Horton W, McKusick VA, Opitz JM, Pope FM, Pyeritz RE, Rimoin DL, Sillence D, Spranger JW, Thompson E, Tsipouras P, Viljoen D, Winship I, Young I: International nosology of
heritable disorders of connective tissue, Berlin, 1986. Am J Med Genet 1988;29:581–594 Article Google Scholar * Pyeritz RE: Clinical variability in the Marfan syndrome. Birth Defects
1979;15:155–178 CAS PubMed Google Scholar * Sakai LY, Keene DR, Engvall E: Fibrillin, a new 350-kD glycoprotein is a component of extracellular microfibrils. J Cell Biol 1986,
103:2499–2509. Article CAS Google Scholar * Hollister DW, Godfrey M, Sakai LY, Pyeritz RE: Immunohistologic abnormalities of the microfibrillarfiber system in the Marfan syndrome. N Engl
J Med 1990;323:152–159 Article CAS Google Scholar * Kainulainen K, Pulkkinen L, Savolainen A, Kaitila I, Peltonen L: Location on chromosome 15 of the gene defect causing Marfan syndrome.
N Engl J Med 1990;323:935–939 Article CAS Google Scholar * Dietz HC, Cutting GR, Pyeritz RE, Maslen CL, Sakai LY, Corson GM, Puffenberger EG, Hamosh A, Nanthakumar EJ, Curristin SM,
Stetten G, Meyers DA, Francomano CA: Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 1991;352:337–339 Article CAS Google Scholar *
Kainulainen K, Sakai LY, Child A, Pope M, Puhakka L, Ryhänen L, Palotie A, Kaitila I, Peltonen L: Two unique mutations in Marfan syndrome resulting in truncated polypeptide chains of
fibrillin. Proc Natl Acad Sci USA 1992;89:5917–5921 Article CAS Google Scholar * Dietz HC, Pyeritz RE, Puffenberger EG, Kendzior RJ Jr, Corson GM, Maslen CL, Sakai LY, Francomano CA,
Cutting GR: Marfan phenotype variability in a family segregating a missense mutation in the epidermal growth factor-like motif of the fibrillin gene. J Clin Invest 1992;89:1674–1680 Article
CAS Google Scholar * Dietz HC, Saraiva JM, Pyeritz RE, Cutting GR, Franomano CA: Clustering of fibrillin (FBN1) missense mutations in Marfan syndrome patients at cysteine residues in
EGF-like domains. Hum Mutat 1992;1:366–374 Article CAS Google Scholar * Dietz HC, Valle D, Francomano CA, Kendzior RJ Jr, Pyeritz RE, Cutting GR: The skipping of constitutive exons in
vivo induced by nonsense mutations. Science 1993;259:680–683 Article CAS Google Scholar * Hewett DR, Lynch JR, Smith R, Sykes BC: A novel fibrillin mutation in the Marfan syndrome which
could disrupt calcium binding of the epidermal growth factor-like module. Hum Mol Genet 1993;2:475–477 Article CAS Google Scholar * Boileau C, Jondeau G, Babron MC, Coulon M, Alexandre
JA, Sakai L, Melki J, Delorme G, Dubourg O, Bonaïti-Pellié C, Bourdarias JP, Junien C: Autosomal dominant Marfan-like connective-tissue disorder with aortic dilation and skeletal anomalies
not linked to the fibrillin genes. Am J Hum Genet 1993;53:46–54 CAS PubMed PubMed Central Google Scholar * Lee B, Godfrey M, Vitale E, Hori H, Mattei MG, Sarfarazi M, Tsipouras P,
Ramirez F, Hollister DW: Linkage of Marfan syndrome and a phenotypically related disorder to two different fibrillin genes. Nature 1991;352:330–334 Article CAS Google Scholar * Hudson T,
Engelstein M, Lee MK, Ho EC, Rubenfield MJ, Adams CP, Housman DE, Dracopoli NC: Isolation and chromosomal assignment of 100 highly informative human simple sequence repeat polymorphisms.
Genomics 1992;13:622–629 Article CAS Google Scholar * Polymeropoulos MH, Xiao H, Rath DS, Merril CR: Tetranucleotide repeat polymorphism at the human aromatase cytochrome P-450 gene (CYP
19). Nucleic Acids Res 1991; 19:195. Article CAS Google Scholar * Vandenplas S, Wiid I, Grobler-Rabie A, Brebner K, Ricketts M, Wallis G, Bester A, Boyd C, Mathew C: Blot hybridization
analysis of genomic DNA. J Med Genet 1984;21:164–172 Article CAS Google Scholar * Syvänen AC, Aalto-Setälä K, Harju L, Kontula K, Söderlund H: A primer-guided nucleotide incorporation
assay in the genotyping of apolipo-protein E. Genomics 1990;8:684–692 Article Google Scholar * Syvänen AC, Ikonen E, Manninen T, Bengtström M, Söderlund H, Aula P, Peltonen L: Convenient
and quantitative determination of the frequency of a mutant allele using solid-phase minisequencing: Application to aspartylglucosaminuria in Finland. Genomics 1992;12:590–595 Article
Google Scholar * Lathrop GM, Lalouel JM, Julier C, Ott J: Strategies for multilocus linkage analysis in humans. Proc Natl Acad Sci 1984;81:3443–3446 Article CAS Google Scholar * Bowcock
AM, Barnes RI, White RL, Kruse TA, Tsipouras P, Sarfarazi M, Jenkins T, Viljoen C, Litt M, Kramer PL, Murray JC, Vergnaud G: The CEPH consortium linkage map of human chromosome 15q. Genomics
1992;14:833–840 Article CAS Google Scholar * Maslen CL, Corson GM, Maddox BK, Glanville RW, Sakai LY: Partial sequence of a candidate gene for the Marfan syndrome. Nature
1991;352:334–337 Article CAS Google Scholar * Tsipouras P, Del Mastro R, Sarfarazi M, Lee B, Vitale E, Child AH, Godfrey M, Devereux RB, Hewett D, Steinmann B, Viljoen D, Sykes BC,
Kilpatrick M, Ramirez F, and the International Marfan Syndrome Collaborative Study: Genetic linkage of the Marfan syndrome, ectopia lentis, and congenital contractural arachnodactyly to the
fibrillin genes on chromosomes 15 and 5. N Engl J Med 1992;326:905–909 Article CAS Google Scholar * Lynch JR, Ogilvie D, Priestley L, Baigrie C, Smith R, Farndon P, Sykes B: Prenatal
diagnosis of osteogenesis imperfecta by identification of the concordant collagen 1 allele. J Med Genet 1991;28:145–150 Article CAS Google Scholar * Magenis RE, Maslen CL, Smith L, Allen
L, Sakai LY: Localization of the fibrillin (FBN) gene to chromosome 15, band q21.1. Genomics 1991;11:346–351 Article CAS Google Scholar * Haidane JBS: The combination of linkage values,
and the calculation of distances between the loci of linked factors. J Genet 1919;8:299–309 Google Scholar * Kainulainen K, Karttunen L, Puhakka L, Sakai L, Peltonen L: Ten novel mutations
of the FBN1 resulting in a wide variety of clinical phenotypes. Nature Genetics, in press. * Lönnqvist L, Child A, Kainulainen K, Davidson R, Puhakka L, Peltonen L: A novel mutation of the
fibrillin gene causing Ectopia Lentis. Genomics, in press. Download references ACKNOWLEDGEMENTS We wish to thank Drs. D.J.H. Brock, A. Child, F. Collins, H. Lenko, I. Kaitila, M. Keston, U.
Kristofferson, A. de Paepe, M. Salo, A. Savolainen and B. Steinmann for DNA samples of MFS patients. We are grateful to Dr. L.Y. Sakai for unpublished sequence information on FBN1 cDNA. The
financial support of the European Concerted Action on Heritable Disorders of Connective Tissue, the National Marfan Foundation of the USA, and the Academy of Finland is gratefully
acknowledged. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Human Molecular Genetics, National Public Health Institute, Mannerheimintie 166, FIN-00300, Helsinki, Finland T.
Rantamäki, L. Lönnqvist, L. Karttunen, K. Kainulainen & L. Peltonen MD, PhD Authors * T. Rantamäki View author publications You can also search for this author inPubMed Google Scholar *
L. Lönnqvist View author publications You can also search for this author inPubMed Google Scholar * L. Karttunen View author publications You can also search for this author inPubMed Google
Scholar * K. Kainulainen View author publications You can also search for this author inPubMed Google Scholar * L. Peltonen MD, PhD View author publications You can also search for this
author inPubMed Google Scholar RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Rantamäki, T., Lönnqvist, L., Karttunen, L. _et al._ DNA Diagnostics of
the Marfan Syndrome: Application of Amplifiable Polymorphic Markers. _Eur J Hum Genet_ 2, 66–75 (1994). https://doi.org/10.1159/000472343 Download citation * Received: 03 May 1993 * Revised:
04 August 1993 * Accepted: 14 October 1993 * Issue Date: January 1994 * DOI: https://doi.org/10.1159/000472343 SHARE THIS ARTICLE Anyone you share the following link with will be able to
read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative KEY WORDS * Connective tissue disease * Chromosome 15 * PCR-based polymorphism
