Emergency use of pilocarpine and pupil block glaucoma in ectopia lentis
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

Sir, Pupillary block glaucoma secondary to ectopia lentis is well described, as is its potential exacerbation with the application of topical miotics.1 However, miotics can still be used in
association with ectopia lentis in two situations: to either confine a dislocated or severely subluxated lens to the posterior chamber pending vitreolensectomy or to confine a dislocated
lens to the anterior chamber pending urgent lens extraction via an anterior approach.2 Both indications are not without risk. We would like to present a short case series to demonstrate the
risks of miosing patients with ectopia lentis in emergency situations and to recommend alternative strategies to pilocarpine. CASE REPORTS CASE 1 A male patient with Marfan's syndrome
and inferiorly subluxated microspherophakic lenses presented to eye casualty in 1994 with the microspherophakic left lens incarcerated in the pupil, endothelial touch, and an intraocular
pressure of 62 mmHg secondary to pupil block. The lens returned to the posterior segment with posturing, oral acetazolamide, and tropicamide mydriasis. The patient was commenced on
pilocarpine 4% qds to the left eye awaiting surgical intervention. The pupil was noted to be well miosed. However, 2 days later he reported increasing pain. Examination revealed the
microspherophakic lens again incarcerated in the pupil and an intraocular pressure of 48 mmHg. The lens returned to the posterior pole with mydriasis and posturing, and a vitreo-lensectomy
was performed the following day. The eye settled and his vision was corrected to 6/9 with an aphakic contact lens. CASE 2 A 27-year-old female with Marfan's syndrome and bilateral
inferiorly subluxated lenses complained of a change of vision in her left eye. She had long experienced an aberration in her left eye due to the margin of her lens encroaching upon the
visual axis and consequently wore aphakic spectacles over homatropine 2% mydriasis. The aberration disappeared 5 days previously, and on examination it was noted that the lens had
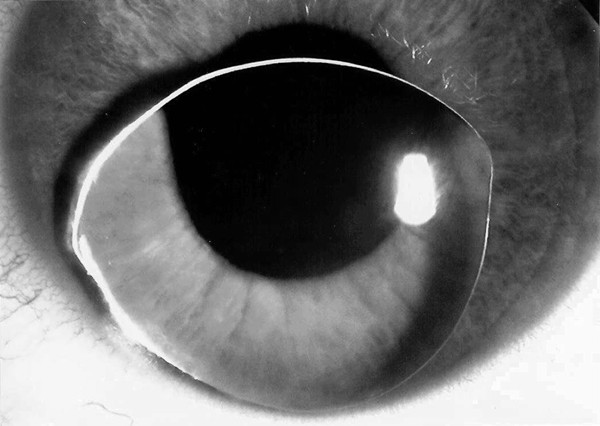
spontaneously dislocated onto the posterior pole. Over the next 3 days, however, the aberration returned and was more prominent. Examination of her left eye revealed that the lens had
completely dislocated into the anterior chamber (Figure 1). The intraocular pressure in the left eye was 16 mmHg. She was immediately commenced on topical pilocarpine 4% qds, in order to
prevent the lens prolapsing back into the posterior segment prior to surgical removal. The following morning, the patient complained of severe pain in her left eye. On examination, the eye
was injected and the lens was completely incarcerated within the pupil. The intraocular pressure was recorded at 50 mmHg. A diagnosis of secondary pupil-block glaucoma was made. The cornea
was markedly oedematous and the view was too compromised to perform laser iridotomy. Topical atropine 1% and intravenous mannitol were administered, which normalized the intraocular pressure
and the patient was taken to theatre. The lens was removed using a bimanual lensectomy technique with a limited anterior vitrectomy and a peripheral iridectomy. No intraocular lens implant
was inserted, as the patient was happy using her aphakic spectacles. At 1 week postoperatively, the vision in the left eye was 6/6. CASE 3 A 51-year-old male was referred to a local eye
clinic by his optometrist who noted deteriorating vision and increasing myopic astigmatism. As part of the examination, his pupils were dilated with tropicamide 1% at which point, inferior
subluxation of the right lens and marked left phacodonesis was noted. He was therefore, given pilocarpine 4% to both eyes to reverse the mydriasis and sent home pending referral for
management of his subluxated lenses and systemic investigations. He returned to his local eye unit that same day with increasing discomfort in the right eye and deteriorating vision. The
crystalline lens in the right eye had dislocated into the anterior chamber leading to pupil block glaucoma and an intraocular pressure of 62 mmHg. He was referred to the teaching unit where
subconjunctival Mydricaine No.2 (Moorfields Eye Hospital Pharmacy), supine posturing, and intravenous diamox followed by intravenous mannitol failed to return the lens to the posterior
segment. As with Case 2, marked corneal oedema prevented the safe placement of a patent iridotomy. Lens ballotment was attempted by corneal massage, but was abandoned due to patient
discomfort. A minimal surgical intervention was therefore performed, in which 0.5 ml of fluid vitreous was aspirated via a 23-gauge needle through the pars plana. The lens was then balloted
through the cornea until it reposited behind the iris. At 1 week postoperatively, the visual acuity was still reduced at 1/60 in the right eye due to persistent corneal oedema. Intraocular
pressure was 8 mmHg bilaterally. He was referred back to his local ophthalmic unit for continuing management and systemic investigation with regard to his ectopia lentis. COMMENT There are
three types of lens-related pupillary block glaucomas in the context of ectopia lentis. The first is pupillary block by a subluxating lens posterior to the iris. The loose zonules allow the
lens to move forward, increasing its contact with the iris. Iris bombé and angle closure glaucoma then develop.1 Treatment with pilocarpine makes the block worse by stimulating ciliary
muscle contraction, thereby loosening the zonules and further increasing anterior lens displacement. Mydriatics tighten the zonules and can break the attack. This has therefore been termed
‘inverse glaucoma’ and occurs only in eyes with some remaining zonular support to the lens. The second type of pupil block is due to incarceration of the lens directly within the pupil.
Increasing aqueous pressure behind a subluxated lens and increasing relative pupillary block leads to further lens movement anteriorly with eventual incarceration within the iris sphincter.
Microspherophakic lenses are particularly prone to this complication, as in Case 1. The third type follows complete dislocation of the lens into the anterior chamber. The posterior surface
of the lens in contact with the iris then induces an anterior pupil block. Anterior dislocation can occur either following pupillary block with posterior aqueous pressure forcing the lens to
dislocate into the anterior chamber, or following dilation, either physiological or iatrogenic, as in Cases 2 and 3. The use of miotics has been suggested in the past for ectopia lentis to
prevent lens dislocation into the anterior chamber but in association with iridectomies to reduce the risk of pupillary block and progressive anterior lens movement. However, Elkington _et
al_3 described a case series of 5 homocystinuria patients on long-term miotics (pilocarpine 4% or ecothiopate 0.125%), who continued to suffer lens dislocations and in which one of the
patients already had a patent iridectomy. Harrison _et al_4 concluded that iridectomies failed to prevent lens dislocation in their group of 45 patients with homocystinuria. The use of
miosis without an iridectomy either long term or while awaiting surgery will increase the risk of pupil block recurring with a subluxated lens and could thereby encourage lens dislocation
anteriorly with subsequent recurrence of incarceration, as in Case 1. This may have been exacerbated by the use of 4% pilocarpine, which can lead to such zonular laxity as to aggravate pupil
block in association with primary angle closure glaucoma.5 Case 1 was noted to be well miosed, which would support this. However, this mechanism would be less pertinent for Cases 2 and 3 in
who the lenses were completely free of zonular support. Jaffe _et al_2 recommends constricting the pupil with a lens dislocated into the anterior chamber, trapping the lens, and allowing
extraction anteriorly. However, without an iridectomy the risk of inducing a pupil block in an otherwise quiet eye with the crystalline lens anterior is significant. As in Case 2, the lens
had presumably been within the anterior chamber for 3 days, but pupil block glaucoma was precipitated only after the initiation of pilocarpine treatment. Nonsurgical management of an
anteriorly dislocated lens includes mydriasis with the patient supine. If this fails, central corneal pressure with a cotton tip swab to reposition the lens manually is recommended.4
Although in both Cases 2 and 3 the cornea was already too oedematous at presentation to allow attempts at iridotomy, the corneal ballotment required by Case 3 (as per cited protocol)
probably contributed to the persistent corneal oedema at discharge. Although a lens completely free of zonular support should have a reduced risk of inducing pupillary block, the lens can
still dislocate into the anterior chamber with the patient on pilocarpine, as in Elkington's series. And a miosed pupil will not only increase the risk of pupillary block from an
anteriorly dislocated lens but also complicate any attempt to reposit the lens back to the posterior pole, as in Case 3. We would therefore like to recommend that if the lens is to be kept
anterior or posterior pending surgery, that posturing the patient either face down or supine, respectively, is a much safer and more effective technique than the use of miosis. Although we
have not reviewed surgical techniques for lens extraction in ectopia lentis, we would suggest that repositioning of the lens posteriorly is associated with less endothelial trauma. The risks
of a posterior approach with a pars plana vitreolensectomy can be reduced in Marfan's patients with intraoperative laser retinopexy to areas of lattice.6 If miosis is to be attempted,
then a laser iridotomy is also advisable not only to prevent pupil block from subluxating lenses in the posterior chamber but also to protect against pupil block if the lens dislocates
anteriorly. Our case series demonstrates the significant risk of precipitating pupil block glaucoma and potentially delaying surgery for ectopia lentis by the emergency use of pilocarpine
without iridotomy. REFERENCES * Ritch R, Shields MB . _The Secondary Glaucomas_. Mosby: St Louis, MO, 1982, pp 136–146. Google Scholar * Jaffe NS, Jaffe MS, Jaffe GF . _Cataract Surgery and
its Complications_, 6th ed. Mosby: St Louis, Missouri, 1997, pp 210. Google Scholar * Elkington AR, Freedman SS, Jay B, Wright P . Anterior dislocation of the lens in homocystinuria. _Br J
Ophthalmol_ 1973; 57: 325–329. Article CAS Google Scholar * Harrison DA, Mullaney PB, Mesfer SA, Awad AH, Dhindsa H . Management of ophthalmic complications of homocystinuria.
_Ophthalmology_ 1998; 105: 1886–1890. Article CAS Google Scholar * American Academy of Ophthalmology. _Basic and Clinical Science Course Section 10: Glaucoma_. American Academy of
Ophthalmology: San Francisco, CA, 1997, p 110. * Hubbard AD, Charteris DG, Cooling RJ . Vitreolensectomy in Marfan's syndrome. _Eye_ 1998; 12: 412–416. Article Google Scholar Download
references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Eye Unit, Queen Alexandra Hospital, Portsmouth, PO6 3LY, UK S A Madill * Manchester Royal Eye Hospital, Oxford Road, Manchester, M13
9WH, UK K E Bain * Princess Alexandra Eye Pavillion, Chalmers Street, Edinburgh, EH3 9HA, UK N Patton, H Bennett & J Singh Authors * S A Madill View author publications You can also
search for this author inPubMed Google Scholar * K E Bain View author publications You can also search for this author inPubMed Google Scholar * N Patton View author publications You can
also search for this author inPubMed Google Scholar * H Bennett View author publications You can also search for this author inPubMed Google Scholar * J Singh View author publications You
can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to S A Madill. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS
ARTICLE Madill, S., Bain, K., Patton, N. _et al._ Emergency use of pilocarpine and pupil block glaucoma in ectopia lentis. _Eye_ 19, 105–107 (2005). https://doi.org/10.1038/sj.eye.6701417
Download citation * Published: 16 April 2004 * Issue Date: 01 January 2005 * DOI: https://doi.org/10.1038/sj.eye.6701417 SHARE THIS ARTICLE Anyone you share the following link with will be
able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative
