Intraoral hair removal on skin graft using nd:yag laser
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

KEY POINTS * Of value to both oral surgeons and proponents of intra-oral laser use. * Demonstrates the efficacy of laser hair removal on an intra-oral graft site. * Documents the innovative
use of laser energy within a dental setting, to the prime benefi t of the patient. ABSTRACT This case report is a demonstration of the effi cacy of laser hair removal on a graft site
intraorally. A Polaris Long Pulse Nd:YAG laser was used for the procedures. You have full access to this article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS
COMPREHENSIVE EXAMINATION OF TATTOO REMOVAL USING A 150 PS ND:YAG LASER IN A PORCINE MODEL Article Open access 11 August 2023 TREATMENT OF HYPERTROPHIC SCARS AND KELOIDS USING AN
INTRALESIONAL 1470 NM BARE-FIBRE DIODE LASER: A NOVEL EFFICIENT MINIMALLY-INVASIVE TECHNIQUE Article Open access 10 December 2020 COMPARISON OF THE EFFICACY AND ADVERSE EFFECTS OF LONG
PULSED 1064 NM ND: YAG LASER AND SCLEROTHERAPY IN THE TREATMENT OF PYOGENIC GRANULOMA IN CHILDREN: A RETROSPECTIVE STUDY Article Open access 22 January 2025 LASER HAIR REMOVAL The demand for
a non-invasive method for hair removal has led to the development of various light source technologies for the process. These include ruby, alexandrite, diode, and Nd:YAG lasers and intense
pulsed light sources. The pulsed Nd:YAG laser produces a light energy at a wavelength of 1,064 nm and targets the chromophore of melanin in the hair follicle. The light energy produced by
each type of system varies, as do the results of treatment. However, a number of papers conclude that the evidence from controlled clinical trials favours the use of lasers for the removal
of unwanted hair.1,2,3 Trials and clinical experience have demonstrated that: * I epilation with lasers induces a partial short-term hair reduction (six1 and 122 months) * II efficacy is
improved when repeated treatments are given1 as a single treatment can reduce hair by 10 to 40% with repeated treatments providing reductions of up to 90%2 * III laser treatments are more
effective than conventional treatments (shaving, wax epilation, electrolysis)1,2 * IV while very few side effects are reported, the patient should be advised of possible temporary problems
caused by laser treatments which include: hyperpigmentation, hypopigmentation, erythema, peri-follicular oedema, folliculitis, blistering or scabbing.1,2 CASE REPORT In November 2005 a male
patient in his forties was referred for laser hair removal by his maxillofacial surgeon. The patient had been diagnosed with a squamous cell carcinoma intraorally distal to his lower first
molar and extending to the retromolar pad area. Surgery had been undertaken and included local resection, level IV neck dissection and reconstruction with radial forearm free flap.6 The
graft took well and healing was uneventful, however after several weeks the patient returned to see his surgeon as the graft had begun to grow hair very extensively.7 The patient was a
Fitzpatrick's skin type 4 and of swarthy Mediterranean complexion with thick dark hair. A Polaris Long Pulse Nd:YAG laser3,4,5 was used for the hair removal procedures. This laser has
the following specifications: Wavelength 1,064 nm: Pulse Duration 10 ms: Output Energy 40J per pulse @ 1Hz: Spot sizes 10.0 mm and 4.0 mm. Beam Delivery by Fibre Optic and focussing
hand-piece including sacrificial window. Aiming Beam Laser diode operating at 635 nm. Following a test patch at manufacturer recommended settings for the patient's skin type (10 mm spot
size at 21.5 J: fluence 27.3 J/cm) to reduce the chances of any adverse skin reaction and to establish the fluence and energy levels to start the treatment, the patient attended clinic on
four further occasions with approximately five-week intervals between each treatment allowing for the hair growth cycle. Great caution was exercised particularly at the graft junction with
the epithelial tissues. Pain relief was provided using Lignocaine spray and cooling with ice cubes wrapped in gauze. The hair was trimmed, where possible, using a scalpel and tweezers prior
to treatments. Access to the treatment site was difficult due to the limited opening the patient could achieve. Two treatments were carried out using the hair removal handpiece with a spot
size of 10 mm (25.5 J/28.5 J) (max fluence 36.4 J/cm). Subsequently, two further treatments were carried out with a 4 mm handpiece normally used for vascular work, but at a reduced energy
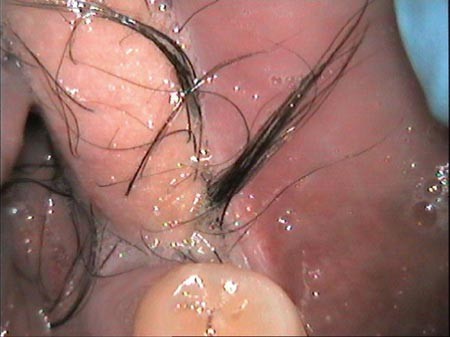
level (9.5 J). Photographs taken with a Vistacam wireless intraoral camera are provided here (Figs 1, 2, 3, 4) and show the progressive improvement in hair reduction during the course of
four treatments, which lasted approximately six months. The final photograph (Fig. 4) shows well the distinct difference in appearance between the keratinised graft area and the
non-keratinised buccal mucosa. At a review appointment in September 2006 there was very little growth. The remaining hair was positioned at the graft junction that was difficult to access.
This Nd:YAG laser treatment has been clinically successful and has met patient expectations. COMMENTS The difficult nature of treating skin that has been grafted into the mouth should not be
underemphasised. Treatment energy levels are critical to ensure that the graft is not destabilised, but enough to effectively remove the hair. Several treatments are required at four to six
week periods due to the hair growth cycle. Selection of the donor site is usually based on the features wanted at the recipient site; this is more important in full-thickness grafts where
more of the characteristics of the donor site skin will be retained by the grafted material in its new location. Where hair growth is undesirable but the graft area contains hair follicles,
it would be preferable (time and other factors permitting) to reduce or eradicate hair from the donor site using an Nd:YAG or other appropriate laser, prior to grafting to the recipient
site. HAZARDS Laser safety and treatment policies and procedures are designed to ensure patient and operator safety at all times. Particular attention must be given by the operator to beam
hazard to skin and eyes and also to fire risk. REFERENCES * Haedersdal M, Wulf H C . Evidence-based review of hair removal using lasers and light sources. _J Eur Acad Dermatol Venereol_
2006; 20: 9–20. Article Google Scholar * Lepselter J, Elman M. Biological and clinical aspects in laser hair removal. _J Dermatol Treatment_ 2004; 15: 72–83. Article Google Scholar *
Littler C M. Hair removal using an Nd:YAG laser system. _Dermatol Clin_ 1999; 17: 401–430. Article Google Scholar * Bencini P L, Luci A, Galimberti M et al. Long-term epilation with
long-pulsed neodimium: YAG laser. _Dermatol Surg_ 1999; 25: 175–178. Article Google Scholar * Levy J L, Trelles M A, De Ramecourt A. Epilation with a long-pulse 1,064 nm Nd:YAG laser in
facial hirsutism. _J Cosmet Laser Ther_ 2001; 3: 175–179. Article Google Scholar * Belli E. Cicconetti A. Valentini V. Intraoral reconstruction with radial forearm flap. _Acta
Otorhinolaryngol_ 1994 Nov-Dec: 14(6): 587–602 Google Scholar * Endo T. Nakayama Y. Kikuchi M. Oral-cavity hair growth after free-flap transfer: case report. _J Reconstr Microsurg_ 2001;
17: 37–38. Article Google Scholar Download references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * The Lumley Dental Practice, 6 Argyle Road Sevenoaks, Kent TN13 1HJ, C. Lumley Authors *
C. Lumley View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to C. Lumley. ADDITIONAL INFORMATION REFEREED PAPER RIGHTS
AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Lumley, C. Intraoral hair removal on skin graft using Nd:YAG laser. _Br Dent J_ 203, 141–142 (2007).
https://doi.org/10.1038/bdj.2007.683 Download citation * Accepted: 24 January 2007 * Published: 11 August 2007 * Issue Date: 11 August 2007 * DOI: https://doi.org/10.1038/bdj.2007.683 SHARE
THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to
clipboard Provided by the Springer Nature SharedIt content-sharing initiative
