In this Issue | Mucosal Immunology
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

IGA: THE CURRENT STATE OF PLAY As is befitting the launch of a journal dedicated to mucosal immunology, there are three items in this issue that focus on quite different aspects of one of
the most historically rich areas of this discipline: the field of IgA biology. First there is a review article from two of the seminal contributors to both the “old” and the “new”
literature, Per Brandtzaeg and Andrew Macpherson, and their colleagues. The authors describe the evolution of discoveries that have shaped our current understanding of the immunological
sites and mechanisms important for IgA B-cell differentiation and IgA production and secretion. Furthermore, they present an insightful perspective on the critical functionality of IgA
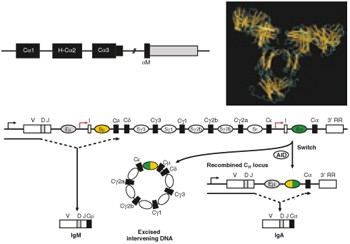
antibodies in host defense and control of commensal bacteria. See pages 11 and 31 IGA SWITCHING IN THE LAMINA PROPRIA? Complementing the review article on IgA is a Commentary from Andrea
Cerutti on the recent, and somewhat controversial, reports of the lamina propria as a site for IgA class switching—a process formerly thought to be restricted to traditional inductive sites
in the mucosa, such as the Peyer's patch. Cerutti eloquently weighs the supporting evidence for this new observation in the context of challenging existing dogma. See page 8 “WHITE
PAPER” ON TERMINOLOGY The final IgA-related article in this issue is a “white paper” that serves to recommend and standardize terminology for describing the molecules and tissues associated
with providing immune protection at mucosal surfaces. It is intended to bring consistency to the nomenclature used in publications and discussions, and to be of guidance to investigators new
to this field. The accompanying figures brilliantly describe the key compartments and components important for mediating and regulating mucosal immunity—and also provide a great teaching
tool for anyone lecturing in the field. See page 31 PEYER'S PATCH DENDRITIC CELLS ON THE MOVE Peyer's patches are small intestinal lymphoid tissues commonly used as a portal of
entry by numerous oral pathogens. Understanding the initiation of an immune response at this particular anatomic location should therefore assist the development of vaccines and therapeutics
against some of the most deadly infectious diseases. Previous studies have demonstrated that bacterial products such as cholera toxin induce dendritic cells at the external epithelial layer
to migrate more deeply into the Peyer's patch, where pathogen-specific T cells are found. In an important new study, Anosova _et al._ demonstrate that at much earlier time points
Peyer's patch dendritic cells actually migrate toward the epithelial layer in response to bacterial products. This rapid transit of dendritic cells to the external surface of the
Peyer's patch probably promotes rapid capture of antigens and microorganisms, which may serve to enhance protective immunity to pathogens and improve the efficacy of mucosal vaccines.
See page 59 MUCOSAL SITE–DEPENDENT CD4+ T-CELL DEPLETION IN HIV INFECTION An understanding of how HIV is controlled by T cells at mucosal sites is important for the development of effective
vaccines. Brenchley and colleagues describe how the immune response to HIV differs at different mucosal effector sites and document how CD4+ T-cell loss differs between compartments such as
the terminal ileum and lung (in bronchoalveolar lavage samples). T-cell loss was greatest in the gut, and the authors report that virus levels were highest in this locale. Measurements of
interleukin-2, tumor necrosis factor-α, and interferon-γ produced by HIV-specific T cells suggest a greater breadth of response in the bronchoalveolar lavage than in blood or gut. Thus,
differences in the quality of the immune responses to HIV and in the extent of CD4+ T-cell depletion are not equivalent at different mucosal sites. See page 49 BREAKING BARRIERS WITH HIV
INFECTION The ability of HIV to cause CD4 depletion and intestinal enteropathy have long been known, although the mechanisms responsible for these effects remain unclear. Here Brenchley and
Douek review the potential means by which epithelial integrity may be compromised in HIV infection and discuss how resulting inflammation and bacterial translocation may exacerbate CD4
depletion via local and systemic immune activation. The authors conclude that, when considering new therapeutic approaches for HIV, the importance of restoring both the immunologic and
epithelial integrity of the gut should be borne in mind. See page 23 RECOMBINANT ADENOVIRUS PROTECTS AGAINST RECTAL AND VAGINAL HSV-2 INFECTION Despite extensive efforts over many years,
identification of the most effective route(s) and vectors for inducing immune responses at mucosal surfaces remains to be determined. Zhu and colleagues used colorectal immunization with
recombinant replication-deficient adenovirus to successfully induce antigen-specific CD8 T cells and IgA-specific antibodies that protect against colorectal challenge of herpes simplex virus
type 2 in the large intestine and vagina. Of particular interest in this study is the finding that a single dose of vaccine gives rise to both cellular and humoral immune responses.
Previous studies using the mouse model have shown that the effects of vaginal immunization without the appropriate adjuvant are limited and are confined to the site of immunization. The
ability of the authors to vaccinate the large intestine to confer protection in the lower genital tract has the potential—if the technique is transferable to humans—to lead to an innovative
strategy that protects at multiple levels against viral pathogens, including HIV. See page 78 MUCOSAL TRAFFIC CONTROLS FOR DISTAL IGA RESPONSES Both selectins and integrin receptors have
roles in lymphocyte trafficking. For homing to the gastrointestinal compartment, lymphocyte expression of α4β7 is critical, with mucosal addressin cell adhesion molecule-1 being the
intestinal ligand. Pascual and co-workers indicate the possible contribution of an alternative integrin αEβ7 in sustaining IgA responses in the upper respiratory tract following oral
immunization. These observations may be used to better design future vaccines targeted to non-intestinal mucosal tissues. See page 68 GUT DENDRITIC CELLS, RETINOIC ACID, AND CD8+ T-CELL
TRAFFICKING There has recently been significant interest in the role of CD103+ dendritic cells and retinoic acid in imprinting T cells with homing receptors specific for directing
trafficking to intestinal tissues. In this report, Svensson and coauthors use a novel transgenic mouse system to further delineate the pathways involved in the induction of the gut homing
receptors α4β7 and CCR9 on CD8+ T cells and identify retinoic acid signaling and antigen dose as important contributing factors in driving gut tropism. See page 38 RIGHTS AND PERMISSIONS
Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE In this Issue. _Mucosal Immunol_ 1, 1–2 (2008). https://doi.org/10.1038/mi.2007.12 Download citation * Published: 11 December
2007 * Issue Date: January 2008 * DOI: https://doi.org/10.1038/mi.2007.12 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link
Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
