Hypoxemia in infants with trisomy 21 in the neonatal intensive care unit
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

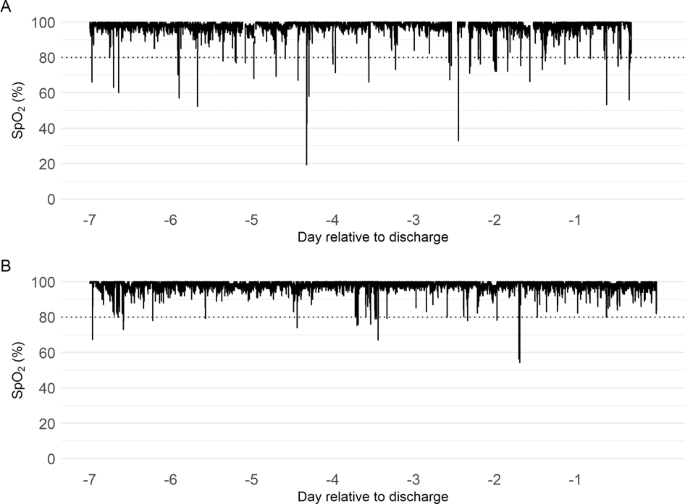
ABSTRACT OBJECTIVE Newborns with trisomy 21 (T21) often require NICU hospitalization. Oxygen desaturations are frequently observed in these infants, even in the absence of congenital heart
defects (CHD). We hypothesized that NICU patients with T21 have more hypoxemia than those without T21. DESIGN All infants with T21 without significant CHD discharged home from the NICU
between 2009 and 2018 were included (_n_ = 23). Controls were matched 20:1 for gestational age and length of stay. We compared daily severe hypoxemia events (SpO2 < 80% for ≥10 s) for the
whole NICU stay and the pre-discharge week. RESULTS Infants with T21 showed significantly more daily hypoxemia events during their entire NICU stay (median 10 versus 7, _p_ = 0.0064), and
more so in their final week (13 versus 7, _p_ = 0.0008). CONCLUSION NICU patients with T21 without CHD experience more severe hypoxemia events than controls, particularly in the week before
discharge. Whether this hypoxemia predicts or contributes to adverse outcomes is unknown. Access through your institution Buy or subscribe This is a preview of subscription content, access
via your institution ACCESS OPTIONS Access through your institution Subscribe to this journal Receive 12 print issues and online access $259.00 per year only $21.58 per issue Learn more Buy
this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: *
Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS MORTALITY AND MORBIDITY OF INFANTS WITH TRISOMY 21,
WEIGHING 1500 GRAMS OR LESS, IN JAPAN Article 05 July 2022 PREGNANCY OUTCOMES AMONG PATIENTS WITH COMPLEX CONGENITAL HEART DISEASE Article Open access 17 September 2024 CRITICAL CONGENITAL
HEART DISEASE BEYOND HLHS AND TGA: NEONATAL BRAIN INJURY AND EARLY NEURODEVELOPMENT Article 13 February 2023 REFERENCES * Boghossian NS, Hansen NI, Bell EF, Stoll BJ, Murray JC, Laptook AR,
et al. Survival and morbidity outcomes for very low birth weight infants with down syndrome. Pediatrics. 2010;126:1132–40. Article Google Scholar * Martin T, Smith A, Breatnach CR, Kent E,
Shanahan I, Boyle M, et al. Infants born with down syndrome: burden of disease in the early neonatal period. J Pediatr. 2018;193:21–26. Article Google Scholar * Mann JP, Statnikov E, Modi
N, Johnson N, Springett A, Morris JK. Management and outcomes of neonates with down syndrome admitted to neonatal units. Birth Defects Res Part A Clin Mol Teratol. 2016;106:468–74. Article
CAS Google Scholar * Ergaz-Shaltiel Z, Engel O, Erlichman I, Naveh Y, Schimmel MS, Tenenbaum A. Neonatal characteristics and perinatal complications in neonates with down syndrome. Am J
Med Genet A. 2017;173:1279–86. Article CAS Google Scholar * McAndrew S, Acharya K, Nghiem-Rao TH, Leuthner S, Clark R, Lagatta J. NICU management and outcomes of infants with trisomy 21
without major anomalies. J Perinatol. 2018;38:1068–73. Article Google Scholar * Waters KA, Castro C, Chawla J. The spectrum of obstructive sleep apnea in infants and children with down
syndrome. Int J Pediatr Otorhinolaryngol. 2020;129:109763. Article Google Scholar * Wong W, Rosen D. Isolated mild sleep-associated hypoventilation in children with down syndrome. Arch Dis
Child. 2017;102:821–4. Article Google Scholar * Colvin KL, Yeager ME. What people with down syndrome can teach us about cardiopulmonary disease. Eur Respir Rev. 2017;26:1–16. * Stanley
MA, Shepherd N, Duvall N, Jenkinson SB, Jalou HE, Givan DC, et al. Clinical identification of feeding and swallowing disorders in 0–6 month old infants with down syndrome. Am J Med Genet A.
2019;179:177–82. Article Google Scholar * Nagraj VP, Sinkin RA, Lake DE, Moorman JR, Fairchild KD. Recovery from bradycardia and desaturation events at 32 weeks corrected age and NICU
length of stay: an indicator of physiologic resilience? Pediatr Res. 2019;86:622–7. Article Google Scholar * Fairchild KD, Nagraj VP, Sullivan BA, Moorman JR, Lake DE. Oxygen desaturations
in the early neonatal period predict development of bronchopulmonary dysplasia. Pediatr Res. 2019;85:987–93. Article Google Scholar * Poets CF. Intermittent hypoxia and long-term
neurological outcome: How are they related? Semin Fetal Neonatal Med. 2020;25:101072. Article Google Scholar * Bush D, Galambos C, Ivy DD, Abman SH, Wolter-Warmerdam K, Hickey F. Clinical
characteristics and risk factors for developing pulmonary hypertension in children with down syndrome. J Pediatr. 2018;202:212–19. e2 Article Google Scholar * Shah PS, Hellmann J, Adatia
I. Clinical characteristics and follow up of down syndrome infants without congenital heart disease who presented with persistent pulmonary hypertension of newborn. J Perinat Med.
2004;32:168–70. Article Google Scholar * Galambos C, Minic AD, Bush D, Nguyen D, Dodson B, Seedorf G, et al. Increased lung expression of anti-angiogenic factors in down syndrome:
potential role in abnormal lung vascular growth and the risk for pulmonary hypertension. PLoS ONE. 2016;11:e0159005. Article Google Scholar * Weijerman ME, van Furth AM, van der Mooren MD,
van Weissenbruch MM, Rammeloo L, Broers CJ, et al. Prevalence of congenital heart defects and persistent pulmonary hypertension of the neonate with down syndrome. Eur J Pediatr.
2010;169:1195–9. Article Google Scholar * Cua CL, Blankenship A, North AL, Hayes J, Nelin LD. Increased incidence of idiopathic persistent pulmonary hypertension in down syndrome neonates.
Pediatr Cardiol. 2007;28:250–4. Article CAS Google Scholar * Ramani M, Bradley WE, Dell’Italia LJ, Ambalavanan N. Early exposure to hyperoxia or hypoxia adversely impacts cardiopulmonary
development. Am J Respir Cell Mol Biol 2015;52:594–602. Article CAS Google Scholar * Horne RSC, Sakthiakumaran A, Bassam A, Thacker J, Walter LM, Davey MJ, et al. Children with down
syndrome and sleep disordered breathing have altered cardiovascular control. Pediatr Res. 2020. * Martin RJ, Di Fiore JM, Macfarlane PM, Wilson CG. Physiologic basis for intermittent hypoxic
episodes in preterm infants. Adv Exp Med Biol. 2012;758:351–8. Article CAS Google Scholar * Das D, Medina B, Baktir MA, Mojabi FS, Fahimi A, Ponnusamy R, et al. Increased incidence of
intermittent hypoxemia in the Ts65Dn mouse model of down syndrome. Neurosci Lett. 2015;604:91–96. Article CAS Google Scholar * Cooney TP, Thurlbeck WM. Pulmonary hypoplasia in down’s
syndrome. N Engl J Med. 1982;307:1170–3. Article CAS Google Scholar * Bush D, Abman SH, Galambos C. Prominent intrapulmonary bronchopulmonary anastomoses and abnormal lung development in
infants and children with down syndrome. J Pediatr. 2017;180:156–62. e1 Article Google Scholar * Simpson R, Oyekan AA, Ehsan Z, Ingram DG. Obstructive sleep apnea in patients with down
syndrome: current perspectives. Nat Sci Sleep. 2018;10:287–93. Article Google Scholar * Lee C-F, Lee C-H, Hsueh W-Y, Lin M-T, Kang K-T. Prevalence of obstructive sleep apnea in children
with down syndrome: a meta-analysis. J Clin Sleep Med. 2018;14:867–75. Article Google Scholar * Southall DP, Stebbens VA, Mirza R, Lang MH, Croft CB, Shinebourne EA. Upper airway
obstruction with hypoxaemia and sleep disruption in down syndrome. Dev Med Child Neurol. 1987;29:734–42. Article CAS Google Scholar * Goffinski A, Stanley MA, Shepherd N, Duvall N,
Jenkinson SB, Davis C, et al. Obstructive sleep apnea in young infants with down syndrome evaluated in a down syndrome specialty clinic. Am J Med Genet A. 2015;167A:324–30. Article Google
Scholar * Coverstone AM, Bird M, Sicard M, Tao Y, Grange DK, Cleveland C, et al. Overnight pulse oximetry for evaluation of sleep apnea among children with trisomy 21. J Clin Sleep Med.
2014;10:1309–15. Article Google Scholar * Siriwardhana LS, Nixon GM, Davey MJ, Mann DL, Landry SA, Edwards BA, et al. Children with down syndrome and sleep disordered breathing display
impairments in ventilatory control. Sleep Med. 2020;77:161–9. Article Google Scholar * O’Driscoll DM, Horne RSC, Davey MJ, Hope SA, Anderson V, Trinder J, et al. Cardiac and sympathetic
activation are reduced in children with down syndrome and sleep disordered breathing. Sleep. 2012;35:1269–75. PubMed PubMed Central Google Scholar * Breslin J, Spanò G, Bootzin R, Anand
P, Nadel L, Edgin J. Obstructive sleep apnea syndrome and cognition in down syndrome. Dev Med Child Neurol. 2014;56:657–64. Article Google Scholar * Lott IT. Antioxidants in down syndrome.
Biochim Biophys Acta. 2012;1822:657–63. Article CAS Google Scholar * Huggard D, Kelly L, Ryan E, McGrane F, Lagan N, Roche E, et al. Increased systemic inflammation in children with down
syndrome. Cytokine. 2020;127:154938. Article CAS Google Scholar * Pecze L, Randi EB, Szabo C. Meta-analysis of metabolites involved in bioenergetic pathways reveals a pseudohypoxic state
in down syndrome. Mol Med. 2020;26:102. Article Google Scholar Download references FUNDING NICHD R01HD072071. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Medicine,
Division of Cardiology, University of Virginia, Charlottesville, VA, USA Katy N. Krahn & Amanda M. Zimmet * Department of Pediatrics, Division of Neonatology, University of Virginia,
Charlottesville, VA, USA V. Peter Nagraj & Karen D. Fairchild * Department of Pediatrics, Division of Cardiology, University of Virginia, Charlottesville, VA, USA Michael A. McCulloch
Authors * Katy N. Krahn View author publications You can also search for this author inPubMed Google Scholar * V. Peter Nagraj View author publications You can also search for this author
inPubMed Google Scholar * Michael A. McCulloch View author publications You can also search for this author inPubMed Google Scholar * Amanda M. Zimmet View author publications You can also
search for this author inPubMed Google Scholar * Karen D. Fairchild View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence
to Karen D. Fairchild. ETHICS DECLARATIONS CONFLICT OF INTEREST The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with
regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Krahn, K.N., Nagraj,
V.P., McCulloch, M.A. _et al._ Hypoxemia in infants with trisomy 21 in the neonatal intensive care unit. _J Perinatol_ 41, 1448–1453 (2021). https://doi.org/10.1038/s41372-021-01105-7
Download citation * Received: 26 January 2021 * Revised: 26 April 2021 * Accepted: 10 May 2021 * Published: 25 May 2021 * Issue Date: June 2021 * DOI:
https://doi.org/10.1038/s41372-021-01105-7 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
