Harnessing cancer immunotherapy during the unexploited immediate perioperative period
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

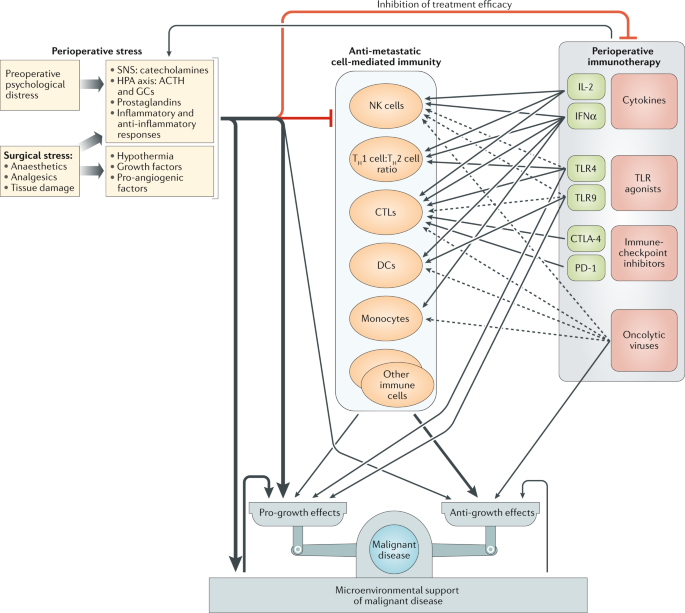
ABSTRACT The immediate perioperative period (days before and after surgery) is hypothesized to be crucial in determining long-term cancer outcomes: during this short period, numerous
factors, including excess stress and inflammatory responses, tumour-cell shedding and pro-angiogenic and/or growth factors, might facilitate the progression of pre-existing micrometastases
and the initiation of new metastases, while simultaneously jeopardizing immune control over residual malignant cells. Thus, application of anticancer immunotherapy during this critical time
frame could potentially improve patient outcomes. Nevertheless, this strategy has rarely been implemented to date. In this Perspective, we discuss apparent contraindications for the
perioperative use of cancer immunotherapy, suggest safe immunotherapeutic and other anti-metastatic approaches during this important time frame and specify desired characteristics of such
interventions. These characteristics include a rapid onset of immune activation, avoidance of tumour-promoting effects, no or minimal increase in surgical risk, resilience to stress-related
factors and minimal induction of stress responses. Pharmacological control of excess perioperative stress–inflammatory responses has been shown to be clinically feasible and could
potentially be combined with immune stimulation to overcome the direct pro-metastatic effects of surgery, prevent immune suppression and enhance immunostimulatory responses. Accordingly, we
believe that certain types of immunotherapy, together with interventions to abrogate stress–inflammatory responses, should be evaluated in conjunction with surgery and, for maximal
effectiveness, could be initiated before administration of adjuvant therapies. Such strategies might improve the overall success of cancer treatment. Access through your institution Buy or
subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Access Nature and 54 other Nature Portfolio journals Get
Nature+, our best-value online-access subscription $29.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12 print issues and online access $209.00 per year only
$17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which are calculated during checkout
ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS THE CANCER-IMMUNE DIALOGUE IN
THE CONTEXT OF STRESS Article 13 October 2023 STRESS AND CANCER: MECHANISMS, SIGNIFICANCE AND FUTURE DIRECTIONS Article 10 September 2021 THERAPY RESISTANCE: OPPORTUNITIES CREATED BY
ADAPTIVE RESPONSES TO TARGETED THERAPIES IN CANCER Article 09 March 2022 REFERENCES * Pudner, R. in _Nursing the Surgical Patient_ 3rd edn 17–34 (Elsevier, 2010). * Horowitz, M., Neeman, E.,
Sharon, E. & Ben-Eliyahu, S. Exploiting the critical perioperative period to improve long-term cancer outcomes. _Nat. Rev. Clin. Oncol._ 12, 213–226 (2015). CAS PubMed PubMed Central
Google Scholar * Hiller, J. G., Perry, N. J., Poulogiannis, G., Riedel, B. & Sloan, E. K. Perioperative events influence cancer recurrence risk after surgery. _Nat. Rev. Clin. Oncol._
15, 205–218 (2018). PubMed Google Scholar * Weitz, J. et al. Dissemination of tumor cells in patients undergoing surgery for colorectal cancer. _Clin. Cancer Res._ 4, 343–348 (1998). CAS
PubMed Google Scholar * Sughrue, M. E., Chang, E. F., Gabriel, R. A., Aghi, M. K. & Blevins, L. S. Excess mortality for patients with residual disease following resection of
pituitary adenomas. _Pituitary_ 14, 276–283 (2011). PubMed Google Scholar * Caprotti, R. et al. Free-from-progression period and overall short preoperative immunotherapy with IL-2
increases the survival of pancreatic cancer patients treated with macroscopically radical surgery. _Anticancer Res._ 28, 1951–1954 (2008). CAS PubMed Google Scholar * Badwe, R. et al.
Single-injection depot progesterone before surgery and survival in women with operable breast cancer: a randomized controlled trial. _J. Clin. Oncol._ 29, 2845–2851 (2011). CAS PubMed
Google Scholar * Brivio, F. et al. Pre-operative immunoprophylaxis with interleukin-2 may improve prognosis in radical surgery for colorectal cancer stage B–C. _Anticancer Res._ 26, 599–603
(2006). CAS PubMed Google Scholar * Haldar, R. & Ben-Eliyahu, S. Reducing the risk of post-surgical cancer recurrence: a perioperative anti-inflammatory anti-stress approach. _Future
Oncol._ 14, 1017–1021 (2018). CAS PubMed Google Scholar * Ricon, I., Hanalis-Miller, T., Haldar, R., Jacoby, R. & Ben-Eliyahu, S. Perioperative biobehavioral interventions to prevent
cancer recurrence through combined inhibition of β-adrenergic and cyclooxygenase 2 signaling. _Cancer_ 125, 45–56 (2019). CAS PubMed Google Scholar * Neeman, E., Zmora, O. &
Ben-Eliyahu, S. A new approach to reducing postsurgical cancer recurrence: perioperative targeting of catecholamines and prostaglandins. _Clin. Cancer Res._ 18, 4895–4902 (2012). CAS PubMed
PubMed Central Google Scholar * Sorski, L. et al. Reducing liver metastases of colon cancer in the context of extensive and minor surgeries through β-adrenoceptors blockade and COX2
inhibition. _Brain Behav. Immun._ 58, 91–98 (2016). CAS PubMed Google Scholar * Seth, R. et al. Surgical stress promotes the development of cancer metastases by a coagulation-dependent
mechanism involving natural killer cells in a murine model. _Ann. Surg._ 258, 158–168 (2013). PubMed Google Scholar * Tai, L. H. et al. Preventing postoperative metastatic disease by
inhibiting surgery-induced dysfunction in natural killer cells. _Cancer Res._ 73, 97–107 (2013). CAS PubMed Google Scholar * Hogan, B. V., Peter, M. B., Shenoy, H. G., Horgan, K. &
Hughes, T. A. Surgery induced immunosuppression. _Surgeon_ 9, 38–43 (2011). PubMed Google Scholar * Greenfeld, K. et al. Immune suppression while awaiting surgery and following it:
dissociations between plasma cytokine levels, their induced production, and NK cell cytotoxicity. _Brain Behav. Immun._ 21, 503–513 (2007). CAS PubMed Google Scholar * Madden, K. S.,
Sanders, V. M. & Felten, D. L. Catecholamine influences and sympathetic neural modulation of immune responsiveness. _Annu. Rev. Pharmacol. Toxicol._ 35, 417–448 (1995). CAS PubMed
Google Scholar * Padgett, D. A. & Glaser, R. How stress influences the immune response. _Trends Immunol._ 24, 444–448 (2003). CAS PubMed Google Scholar * Forget, P. et al.
Neutrophil:lymphocyte ratio and intraoperative use of ketorolac or diclofenac are prognostic factors in different cohorts of patients undergoing breast, lung, and kidney cancer surgery.
_Ann. Surg. Oncol._ 20, S650–S660 (2013). PubMed Google Scholar * Cata, J. P., Guerra, C. E., Chang, G. J., Gottumukkala, V. & Joshi, G. P. Non-steroidal anti-inflammatory drugs in the
oncological surgical population: beneficial or harmful? A systematic review of the literature. _Br. J. Anaesth._ 119, 750–764 (2017). CAS PubMed Google Scholar * Ben-Eliyahu, S.,
Shakhar, G., Rosenne, E., Levinson, Y. & Beilin, B. Hypothermia in barbiturate-anesthetized rats suppresses natural killer cell activity and compromises resistance to tumor metastasis: a
role for adrenergic mechanisms. _Anesthesiology_ 91, 732–740 (1999). CAS PubMed Google Scholar * Beilin, B. et al. Effects of mild perioperative hypothermia on cellular immune responses.
_Anesthesiology_ 89, 1133–1140 (1998). CAS PubMed Google Scholar * Aibiki, M. et al. Effect of moderate hypothermia on systemic and internal jugular plasma IL-6 levels after traumatic
brain injury in humans. _J. Neurotrauma_ 16, 225–232 (1999). CAS PubMed Google Scholar * Nielsen, H. J. Detrimental effects of perioperative blood-transfusion. _Br. J. Surg._ 82, 582–587
(1995). CAS PubMed Google Scholar * Landers, D. F., Hill, G. E., Wong, K. C. & Fox, I. J. Blood transfusion-induced immunomodulation. _Anesth. Analg._ 82, 187–204 (1996). CAS PubMed
Google Scholar * Heaney, A. & Buggy, D. J. Can anaesthetic and analgesic techniques affect cancer recurrence or metastasis? _Br. J. Anaesth._ 109, i17–i28 (2012). PubMed Google
Scholar * Filipazzi, P., Huber, V. & Rivoltini, L. Phenotype, function and clinical implications of myeloid-derived suppressor cells in cancer patients. _Cancer Immunol. Immunother._
61, 255–263 (2012). CAS PubMed Google Scholar * Mantovani, A., Marchesi, F., Malesci, A., Laghi, L. & Allavena, P. Tumour-associated macrophages as treatment targets in oncology.
_Nat. Rev. Clin. Oncol._ 14, 399–416 (2017). CAS PubMed PubMed Central Google Scholar * Lindau, D., Gielen, P., Kroesen, M., Wesseling, P. & Adema, G. J. The immunosuppressive tumour
network: myeloid-derived suppressor cells, regulatory T cells and natural killer T cells. _Immunology_ 138, 105–115 (2013). CAS PubMed PubMed Central Google Scholar * Lorusso, G. &
Rugg, C. The tumor microenvironment and its contribution to tumor evolution toward metastasis. _Histochem. Cell Biol._ 130, 1091–1103 (2008). CAS PubMed Google Scholar * Lopez-Novoa, J.
M. & Nieto, M. A. Inflammation and EMT: an alliance towards organ fibrosis and cancer progression. _EMBO Mol. Med._ 1, 303–314 (2009). CAS PubMed PubMed Central Google Scholar * Yu,
H., Pardoll, D. & Jove, R. STATs in cancer inflammation and immunity: a leading role for STAT3. _Nat. Rev. Cancer_ 9, 798–809 (2009). CAS PubMed PubMed Central Google Scholar *
Mantovani, A., Sozzani, S., Locati, M., Allavena, P. & Sica, A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. _Trends
Immunol._ 23, 549–555 (2002). CAS PubMed Google Scholar * Cole, S. W., Nagaraja, A. S., Lutgendorf, S. K., Green, P. A. & Sood, A. K. Sympathetic nervous system regulation of the
tumour microenvironment. _Nat. Rev. Cancer_ 15, 563–572 (2015). CAS PubMed PubMed Central Google Scholar * Shaashua, L. et al. Perioperative COX-2 and β-adrenergic blockade improves
metastatic biomarkers in breast cancer patients in a phase-II randomized trial. _Clin. Cancer Res._ 23, 4651–4661 (2017). CAS PubMed PubMed Central Google Scholar * Aguirre-Ghiso, J. A.
Models Mechanisms and clinical evidence for cancer dormancy. _Nat. Rev. Cancer_ 7, 834–846 (2007). CAS PubMed PubMed Central Google Scholar * Jones, P. A. & Baylin, S. B. The
fundamental role of epigenetic events in cancer. _Nat. Rev. Genet._ 3, 415–428 (2002). CAS PubMed Google Scholar * Lambert, A. W., Pattabiraman, D. R. & Weinberg, R. A. Emerging
biological principles of metastasis. _Cell_ 168, 670–691 (2017). CAS PubMed PubMed Central Google Scholar * Drake, C. G., Jaffee, E. & Pardoll, D. M. Mechanisms of immune evasion by
tumors. _Adv. Immunol._ 90, 51–81 (2006). CAS PubMed Google Scholar * McArdle, C. S., McMillan, D. C. & Hole, D. J. Impact of anastomotic leakage on long-term survival of patients
undergoing curative resection for colorectal cancer. _Br. J. Surg._ 92, 1150–1154 (2005). CAS PubMed Google Scholar * Erinjeri, J. P. et al. Timing of administration of bevacizumab
chemotherapy affects wound healing after chest wall port placement. _Cancer_ 117, 1296–1301 (2011). CAS PubMed Google Scholar * Payne, W. G. et al. Wound healing in patients with cancer.
_Eplasty_ 8, e9 (2008). PubMed PubMed Central Google Scholar * Guan, M., Zhou, Y. P., Sun, J. L. & Chen, S. C. Adverse events of monoclonal antibodies used for cancer therapy. _Biomed
Res. Int._ 2015, 428169 (2015). PubMed PubMed Central Google Scholar * Cohen, S. C., Gabelnick, H. L., Johnson, R. K. & Goldin, A. Effects of cyclophosphamide and adriamycin on the
healing of surgical wounds in mice. _Cancer_ 36, 1277–1281 (1975). CAS PubMed Google Scholar * Engelmann, U., Grimm, K., Gronniger, J., Burger, R. & Jacobi, G. H. Influence of
_cis_-platinum on healing of enterostomies in the rat. _Eur. Urol._ 9, 45–49 (1983). CAS PubMed Google Scholar * Newcombe, J. F. & Chir, M. Effect of intra-arterial nitrogen mustard
infusion on wound healing in rabbits—formation of granulation tissue and wound contraction. _Ann. Surg._ 163, 319–329 (1966). CAS PubMed PubMed Central Google Scholar * Nissen-Meyer, R.,
Kjellgren, K., Malmio, K., Mansson, B. & Norin, T. Surgical adjuvant chemotherapy: results with one short course with cyclophosphamide after mastectomy for breast cancer. _Cancer_ 41,
2088–2098 (1978). CAS PubMed Google Scholar * Arikan, A. Y., Senel, F. M., Akman, R. Y. & Can, C. Comparison of the effects of various anticancer agents on intestinal anastomosis
after intraperitoneal administration. _Surg. Today_ 29, 741–746 (1999). CAS PubMed Google Scholar * Garfield, J. & Dayan, A. D. Postoperative intracavitary chemotherapy of malignant
gliomas—preliminary study using methotrexate. _J. Neurosurg._ 39, 315–322 (1973). CAS PubMed Google Scholar * Cohn, I., Slack, N. H. & Fisher, B. Complications and toxic
manifestations of surgical adjuvant chemotherapy for breast cancer. _Surg. Gynecol. Obstet._ 127, 1201–1209 (1968). PubMed Google Scholar * Rasmussen, L. & Arvin, A.
Chemotherapy-induced immunosuppression. _Environ. Health Perspect._ 43, 21–25 (1982). CAS PubMed PubMed Central Google Scholar * Harris, J., Sengar, D., Stewart, T. & Hyslop, D. The
effect of immunosuppressive chemotherapy on immune function in patients with malignant disease. _Cancer_ 37, 1058–1069 (1976). CAS PubMed Google Scholar * Galluzzi, L., Buque, A., Kepp,
O., Zitvogel, L. & Kroemer, G. Immunological effects of conventional chemotherapy and targeted anticancer agents. _Cancer Cell_ 28, 690–714 (2015). CAS PubMed Google Scholar *
Zitvogel, L., Apetoh, L., Ghiringhelli, F. & Kroemer, G. Immunological aspects of cancer chemotherapy. _Nat. Rev. Immunol._ 8, 59–73 (2008). CAS PubMed Google Scholar * Ding, Z. C. et
al. Immunosuppressive myeloid cells induced by chemotherapy attenuate antitumor CD4+ T-cell responses through the PD-1–PD-L1 axis. _Cancer Res._ 74, 3441–3453 (2014). CAS PubMed PubMed
Central Google Scholar * Tsang, Y. W. et al. Chemotherapy-induced immunosuppression is restored by a fermented soybean extract: a proof of concept clinical trial. _Nutr. Res._ 27, 679–684
(2007). CAS Google Scholar * Kang, D. H. et al. Significant impairment in immune recovery after cancer treatment. _Nurs. Res._ 58, 105–114 (2009). PubMed PubMed Central Google Scholar *
Verma, R. et al. Lymphocyte depletion and repopulation after chemotherapy for primary breast cancer. _Breast Cancer Res._ 18, 10 (2016). PubMed PubMed Central Google Scholar *
Couzin-Frankel, J. Breakthrough of the year 2013. Cancer immunotherapy. _Science_ 342, 1432–1433 (2013). CAS PubMed Google Scholar * Lee, S. & Margolin, K. Cytokines in cancer
immunotherapy. _Cancers_ 3, 3856–3893 (2011). CAS PubMed PubMed Central Google Scholar * Kaczanowska, S., Joseph, A. M. & Davila, E. TLR agonists: our best frenemy in cancer
immunotherapy. _J. Leukoc. Biol._ 93, 847–863 (2013). CAS PubMed PubMed Central Google Scholar * Pardoll, D. M. The blockade of immune checkpoints in cancer immunotherapy. _Nat. Rev.
Cancer_ 12, 252–264 (2012). CAS PubMed PubMed Central Google Scholar * Mastrangelo, M. J. & Lattime, E. C. Virotherapy clinical trials for regional disease: in situ immune modulation
using recombinant poxvirus vectors. _Cancer Gene Ther._ 9, 1013–1021 (2002). CAS PubMed Google Scholar * Gelderman, K. A., Tomlinson, S., Ross, G. D. & Gorter, A. Complement function
in mAb-mediated cancer immunotherapy. _Trends Immunol._ 25, 158–164 (2004). CAS PubMed Google Scholar * Sippel, T. R. et al. Neutrophil degranulation and immunosuppression in patients
with GBM: restoration of cellular immune function by targeting arginase I. _Clin. Cancer Res._ 17, 6992–7002 (2011). CAS PubMed Google Scholar * Brahmer, J. et al. Nivolumab versus
docetaxel in advanced squamous-cell non-small-cell lung cancer. _N. Engl. J. Med._ 373, 123–135 (2015). CAS PubMed PubMed Central Google Scholar * Herbst, R. S. et al. Pembrolizumab
versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. _Lancet_ 387, 1540–1550 (2016). CAS PubMed Google
Scholar * Coppin, C. et al. Immunotherapy for advanced renal cell cancer. _Cochrane Database Syst. Rev._ 12, CD001425 (2005). Google Scholar * Robert, C. et al. Pembrolizumab versus
ipilimumab in advanced melanoma. _N. Engl. J. Med._ 372, 2521–2532 (2015). CAS PubMed Google Scholar * Schmid, P. et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast
cancer. _N. Engl. J. Med._ 379, 2108–2121 (2018). CAS PubMed Google Scholar * Kojima, T. et al. Pembrolizumab versus chemotherapy as second-line therapy for advanced esophageal cancer:
phase III KEYNOTE-181 study. _J. Clin. Oncol_. 37 (Suppl. 4), 2-2 (2019). Google Scholar * Borghaei, H. et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer.
_N. Engl. J. Med._ 373, 1627–1639 (2015). CAS PubMed PubMed Central Google Scholar * Carlino, M. S. & Long, G. V. Is chemotherapy still an option in the treatment of melanoma? _Ann.
Oncol._ 26, 2203–2204 (2015). CAS PubMed Google Scholar * Hamid, O. et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. _N. Engl. J. Med._ 369, 134–144 (2013).
CAS PubMed PubMed Central Google Scholar * Cohen, J. & Carlet, J. INTERSEPT: an international, multicenter, placebo-controlled trial of monoclonal antibody to human tumor necrosis
factor-α in patients with sepsis. International Sepsis Trial Study Group. _Crit. Care Med._ 24, 1431–1440 (1996). CAS PubMed Google Scholar * Castro, J. E., Sandoval-Sus, J. D., Bole, J.,
Rassenti, L. & Kipps, T. J. Rituximab in combination with high-dose methylprednisolone for the treatment of fludarabine refractory high-risk chronic lymphocytic leukemia. _Leukemia_ 22,
2048–2053 (2008). CAS PubMed PubMed Central Google Scholar * Wolters, U., Wolf, T., Stützer, H. & Schröder, T. ASA classification and perioperative variables as predictors of
postoperative outcome. _Br. J. Anaesth._ 78, 228–228 (1997). Google Scholar * National Cancer Institute. Find NCI-supported clinical trials. _NCI_
https://www.cancer.gov/about-cancer/treatment/clinical-trials/search (2020). * US National Library of Medicine._ ClinicalTrials.gov_ https://clinicaltrials.gov/ (2020). * Pollard, J. W.
Tumour-educated macrophages promote tumour progression and metastasis. _Nat. Rev. Cancer_ 4, 71–78 (2004). CAS PubMed Google Scholar * Young, M. R. & Knies, S. Prostaglandin E
production by Lewis lung carcinoma: mechanism for tumor establishment in vivo. _J. Natl Cancer Inst._ 72, 919–922 (1984). CAS PubMed Google Scholar * Beatty, G. L. & Gladney, W. L.
Immune escape mechanisms as a guide for cancer immunotherapy. _Clin. Cancer Res._ 21, 687–692 (2015). CAS PubMed Google Scholar * Dunn, G. P., Bruce, A. T., Ikeda, H., Old, L. J. &
Schreiber, R. D. Cancer immunoediting: from immunosurveillance to tumor escape. _Nat. Immunol._ 3, 991–998 (2002). CAS PubMed Google Scholar * Quail, D. F. & Joyce, J. A.
Microenvironmental regulation of tumor progression and metastasis. _Nat. Med._ 19, 1423–1437 (2013). CAS PubMed PubMed Central Google Scholar * Steeg, P. S. Tumor metastasis: mechanistic
insights and clinical challenges. _Nat. Med._ 12, 895–904 (2006). CAS PubMed Google Scholar * Rashid, O. M. et al. Resection of the primary tumor improves survival in metastatic breast
cancer by reducing overall tumor burden. _Surgery_ 153, 771–778 (2013). PubMed Google Scholar * Hodi, F. S. et al. Improved survival with ipilimumab in patients with metastatic melanoma.
_N. Engl. J. Med._ 363, 711–723 (2010). CAS PubMed PubMed Central Google Scholar * Lasek, W., Zagozdzon, R. & Jakobisiak, M. Interleukin 12: still a promising candidate for tumor
immunotherapy? _Cancer Immunol. Immunother._ 63, 419–435 (2014). CAS PubMed PubMed Central Google Scholar * Kanzler, H., Barrat, F. J., Hessel, E. M. & Coffman, R. L. Therapeutic
targeting of innate immunity with Toll-like receptor agonists and antagonists. _Nat. Med._ 13, 552–559 (2007). CAS PubMed Google Scholar * Marano, L. et al. Clinical and immunological
impact of early postoperative enteral immunonutrition after total gastrectomy in gastric cancer patients: a prospective randomized study. _Ann. Surg. Oncol._ 20, 3912–3918 (2013). PubMed
Google Scholar * Link, B. K. et al. Oligodeoxynucleotide CpG 7909 delivered as intravenous infusion demonstrates immunologic modulation in patients with previously treated non-Hodgkin
lymphoma. _J. Immunother._ 29, 558–568 (2006). CAS PubMed Google Scholar * Reinartz, S. et al. Evaluation of immunological responses in patients with ovarian cancer treated with the
anti-idiotype vaccine ACA125 by determination of intracellular cytokines—a preliminary report. _Hybridoma_ 18, 41–45 (1999). CAS PubMed Google Scholar * Goldfarb, Y. et al. Improving
postoperative immune status and resistance to cancer metastasis: a combined perioperative approach of immunostimulation and prevention of excessive surgical stress responses. _Ann. Surg._
253, 798–810 (2011). PubMed Google Scholar * Glasner, A. et al. Improving survival rates in two models of spontaneous postoperative metastasis in mice by combined administration of a
β-adrenergic antagonist and a cyclooxygenase-2 inhibitor. _J. Immunol._ 184, 2449–2457 (2010). CAS PubMed Google Scholar * Matzner, P. et al. Perioperative treatment with the new
synthetic TLR-4 agonist GLA-SE reduces cancer metastasis without adverse effects. _Int. J. Cancer_ 138, 1754–1764 (2016). CAS PubMed Google Scholar * Park, C. G. et al. Extended release
of perioperative immunotherapy prevents tumor recurrence and eliminates metastases. _Sci. Transl Med._ 10, eaar1916 (2018). PubMed Google Scholar * Tai, L. H. et al. Perioperative
influenza vaccination reduces postoperative metastatic disease by reversing surgery-induced dysfunction in natural killer cells. _Clin. Cancer Res._ 19, 5104–5115 (2013). CAS PubMed Google
Scholar * Tai, L. H., Zhang, J. Q. & Auer, R. C. Preventing surgery-induced NK cell dysfunction and cancer metastases with influenza vaccination. _Oncoimmunology_ 2, e26618 (2013).
PubMed PubMed Central Google Scholar * Zou, W. Regulatory T cells, tumour immunity and immunotherapy. _Nat. Rev. Immunol._ 6, 295–307 (2006). CAS PubMed Google Scholar * Basith, S.,
Manavalan, B., Yoo, T. H., Kim, S. G. & Choi, S. Roles of Toll-like receptors in cancer: a double-edged sword for defense and offense. _Arch. Pharm. Res._ 35, 1297–1316 (2012). CAS
PubMed Google Scholar * Hong, I. S. Stimulatory versus suppressive effects of GM-CSF on tumor progression in multiple cancer types. _Exp. Mol. Med._ 48, e242 (2016). CAS PubMed PubMed
Central Google Scholar * He, W. et al. TLR4 signaling promotes immune escape of human lung cancer cells by inducing immunosuppressive cytokines and apoptosis resistance. _Mol. Immunol._
44, 2850–2859 (2007). CAS PubMed Google Scholar * Kelly, M. G. et al. TLR-4 signaling promotes tumor growth and paclitaxel chemoresistance in ovarian cancer. _Cancer Res._ 66, 3859–3868
(2006). CAS PubMed Google Scholar * Berdel, W. E., Danhauserriedl, S., Steinhauser, G. & Winton, E. F. Various human hematopoietic growth-factors (interleukin-3, GM-CSF, G-CSF)
stimulate clonal growth of nonhematopoietic tumor-cells. _Blood_ 73, 80–83 (1989). CAS PubMed Google Scholar * Dedhar, S., Gaboury, L., Galloway, P. & Eaves, C. Human
granulocyte–macrophage colony-stimulating factor is a growth factor active on a variety of cell types of nonhemopoietic origin. _Proc. Natl Acad. Sci. USA_ 85, 9253–9257 (1988). CAS PubMed
PubMed Central Google Scholar * Ninck, S. et al. Expression profiles of angiogenic growth factors in squamous cell carcinomas of the head and neck. _Int. J. Cancer_ 106, 34–44 (2003).
CAS PubMed Google Scholar * Levi, B. et al. Stress impairs the efficacy of immune stimulation by CpG-C: potential neuroendocrine mediating mechanisms and significance to tumor metastasis
and the perioperative period. _Brain Behav. Immun._ 56, 209–220 (2016). CAS PubMed PubMed Central Google Scholar * Nagato, T. & Celis, E. A novel combinatorial cancer immunotherapy
poly-IC and blockade of the PD-1/PD-L1 pathway. _Oncoimmunology_ 3, e28440 (2014). PubMed PubMed Central Google Scholar * Matzner, P. et al. Deleterious synergistic effects of distress
and surgery on cancer metastasis: abolishment through an integrated perioperative immune-stimulating stress-inflammatory-reducing intervention. _Brain Behav. Immun._ 80, 170–178 (2019).
PubMed Google Scholar * Zambouri, A. Preoperative evaluation and preparation for anesthesia and surgery. _Hippokratia_ 11, 13–21 (2007). CAS PubMed PubMed Central Google Scholar *
Fleisher, L. A. et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of
Cardiology/American Heart Association Task Force on practice guidelines. _J. Am. Coll. Cardiol._ 64, e77–e137 (2014). PubMed Google Scholar * Kwon, S. et al. Importance of perioperative
glycemic control in general surgery: a report from the surgical care and outcomes assessment program. _Ann. Surg._ 257, 8–14 (2013). PubMed Google Scholar * Ge, P. L., Du, S. D. & Mao,
Y. L. Advances in preoperative assessment of liver function. _Hepatobiliary Pancreat. Dis. Int._ 13, 361–370 (2014). PubMed Google Scholar * King, M. S. Preoperative evaluation. _Am. Fam.
Physician_ 62, 387–396 (2000). CAS PubMed Google Scholar * Tinker, J. H. et al. _Recommendations and Guidelines for Preoperative Evaluation of the Surgical Patient with Emphasis on the
Cardiac Patient for Non-Cardiac Surgery_ (University of Nebraska Medical Center, 2006). * Fry, D. E. Sepsis, systemic inflammatory response, and multiple organ dysfunction: the mystery
continues. _Am. Surg._ 78, 1–8 (2012). PubMed Google Scholar * Marik, P. E. & Flemmer, M. The immune response to surgery and trauma: implications for treatment. _J. Trauma Acute Care_
73, 801–808 (2012). CAS Google Scholar * Lee, J. et al. Maintenance of colonic homeostasis by distinctive apical TLR9 signalling in intestinal epithelial cells. _Nat. Cell Biol._ 8,
1327–1336 (2006). CAS PubMed Google Scholar * Chen, G. Y. & Nunez, G. Sterile inflammation: sensing and reacting to damage. _Nat. Rev. Immunol._ 10, 826–837 (2010). CAS PubMed
PubMed Central Google Scholar * Atzpodien, J. et al. IL-2 in combination with IFN-α and 5-FU versus tamoxifen in metastatic renal cell carcinoma: long-term results of a controlled
randomized clinical trial. _Br. J. Cancer_ 85, 1130–1136 (2001). CAS PubMed PubMed Central Google Scholar * Manegold, C. et al. Randomized phase II trial of a Toll-like receptor 9
agonist oligodeoxynucleotide, PF-3512676, in combination with first-line taxane plus platinum chemotherapy for advanced-stage non-small-cell lung cancer. _J. Clin. Oncol._ 26, 3979–3986
(2008). CAS PubMed Google Scholar * Gridelli, C. et al. Immunotherapy of non-small cell lung cancer: report from an international experts panel meeting of the Italian Association of
Thoracic Oncology. _Expert Opin. Biol. Ther._ 16, 1479–1489 (2016). CAS PubMed Google Scholar * Bertrand, A., Kostine, M., Barnetche, T., Truchetet, M. E. & Schaeverbeke, T. Immune
related adverse events associated with anti-CTLA-4 antibodies: systematic review and meta-analysis. _BMC Med._ 13, 211 (2015). PubMed PubMed Central Google Scholar * Desborough, J. P. The
stress response to trauma and surgery. _Br. J. Anaesth._ 85, 109–117 (2000). CAS PubMed Google Scholar * Goldfarb, Y., Levi, B., Sorski, L., Frenkel, D. & Ben-Eliyahu, S. CpG-C
immunotherapeutic efficacy is jeopardized by ongoing exposure to stress: potential implications for clinical use. _Brain Behav. Immun._ 25, 67–76 (2011). CAS PubMed Google Scholar *
Biesmans, S. et al. Effect of stress and peripheral immune activation on astrocyte activation in transgenic bioluminescent Gfap-luc mice. _Glia_ 63, 1126–1137 (2015). PubMed Google Scholar
* Menard, C., Pfau, M. L., Hodes, G. E. & Russo, S. J. Immune and neuroendocrine mechanisms of stress vulnerability and resilience. _Neuropsychopharmacology_ 42, 62–80 (2017). CAS
PubMed Google Scholar * Benbenishty, A. et al. Prophylactic TLR9 stimulation reduces brain metastasis through microglia activation. _PLoS Biol._ 17, e2006859 (2019). CAS PubMed PubMed
Central Google Scholar * Haldar, R. et al. Perioperative inhibition of β-adrenergic and COX2 signaling in a clinical trial in breast cancer patients improves tumor Ki-67 expression, serum
cytokine levels, and PBMCs transcriptome. _Brain Behav. Immun._ 73, 294–309 (2018). CAS PubMed Google Scholar * Bhatia, S., Tykodi, S. S. & Thompson, J. A. Treatment of metastatic
melanoma: an overview. _Oncology_ 23, 488–496 (2009). PubMed Google Scholar * Hayley, S., Merali, Z. & Anisman, H. Stress and cytokine-elicited neuroendocrine and neurotransmitter
sensitization: implications for depressive illness. _Stress_ 6, 19–32 (2003). CAS PubMed Google Scholar * Anisman, H., Poulter, M. O., Gandhi, R., Merali, Z. & Hayley, S. Interferon-α
effects are exaggerated when administered on a psychosocial stressor backdrop: cytokine, corticosterone and brain monoamine variations. _J. Neuroimmunol._ 186, 45–53 (2007). CAS PubMed
Google Scholar * Pollak, Y. & Yirmiya, R. Cytokine-induced changes in mood and behaviour: implications for “depression due to a general medical condition”, immunotherapy and
antidepressive treatment. _Int. J. Neuropsychopharmacol._ 5, 389–399 (2002). CAS PubMed Google Scholar * Lissoni, P. et al. Inhibitory effect of interleukin-3 on interleukin-2-induced
cortisol release in the immunotherapy of cancer. _J. Biol. Regul. Homeost. Agents_ 6, 113–115 (1992). CAS PubMed Google Scholar * Lenczowski, M. J. et al. Central administration of rat
IL-6 induces HPA activation and fever but not sickness behavior in rats. _Am. J. Physiol._ 276, R652–R658 (1999). CAS PubMed Google Scholar * Bernabe, D. G., Tamae, A. C., Biasoli, E. R.
& Oliveira, S. H. Stress hormones increase cell proliferation and regulates interleukin-6 secretion in human oral squamous cell carcinoma cells. _Brain Behav. Immun._ 25, 574–583 (2011).
CAS PubMed Google Scholar * Saphier, D. Neuroendocrine effects of interferon-α in the rat. _Adv. Exp. Med. Biol._ 373, 209–218 (1995). CAS PubMed Google Scholar * Saphier, D., Welch,
J. E. & Chuluyan, H. E. α-Interferon inhibits adrenocortical secretion via Mu 1-opioid receptors in the rat. _Eur. J. Pharmacol._ 236, 183–191 (1993). CAS PubMed Google Scholar *
Goebel, M. U. et al. Acute interferon β1b administration alters hypothalamic–pituitary–adrenal axis activity, plasma cytokines and leukocyte distribution in healthy subjects.
_Psychoneuroendocrinology_ 27, 881–892 (2002). CAS PubMed Google Scholar * Holsboer, F. et al. Acute adrenocortical stimulation by recombinant γ-interferon in human controls. _Life Sci._
42, 1–5 (1988). CAS PubMed Google Scholar * Lepelletier, Y. et al. Toll-like receptor control of glucocorticoid-induced apoptosis in human plasmacytoid predendritic cells (pDCs). _Blood_
116, 3389–3397 (2010). CAS PubMed Google Scholar * Santini-Oliveira, M. et al. Schistosomiasis vaccine candidate Sm14/GLA-SE: phase 1 safety and immunogenicity clinical trial in healthy,
male adults. _Vaccine_ 34, 586–594 (2016). CAS PubMed Google Scholar * Treanor, J. J. et al. Evaluation of safety and immunogenicity of recombinant influenza hemagglutinin
(H5/Indonesia/05/2005) formulated with and without a stable oil-in-water emulsion containing glucopyranosyl-lipid A (SE plus GLA) adjuvant. _Vaccine_ 31, 5760–5765 (2013). CAS PubMed
Google Scholar * Krieg, A. M. CpG still rocks! Update on an accidental drug. _Nucleic Acid. Ther._ 22, 77–89 (2012). CAS PubMed Google Scholar * Zhang, Y., Gu, Y. H., Guo, T. K., Li, Y.
P. & Cai, H. Perioperative immunonutrition for gastrointestinal cancer: a systematic review of randomized controlled trials. _Surg. Oncol._ 21, E87–E95 (2012). PubMed Google Scholar *
Calder, P. C. & Kew, S. The immune system: a target for functional foods? _Br. J. Nutr._ 88, S165–S176 (2002). CAS PubMed Google Scholar * Nestlé Health Science. Impact. _Nestlé_
https://www.nestlehealthscience.com/brands/impact/impact (2019). * Caglayan, K. et al. The impact of preoperative immunonutrition and other nutrition models on tumor infiltrative lymphocytes
in colorectal cancer patients. _Am. J. Surg._ 204, 416–421 (2012). PubMed Google Scholar * Sorensen, L. D., McCarthy, M., Baumgartner, M. B. & Demars, C. S. Perioperative
immunonutrition in head and neck cancer. _Laryngoscope_ 119, 1358–1364 (2009). CAS PubMed Google Scholar * Turnock, A. et al. Perioperative immunonutrition in well-nourished patients
undergoing surgery for head and neck cancer: evaluation of inflammatory and immunologic outcomes. _Nutrients_ 5, 1186–1199 (2013). CAS PubMed PubMed Central Google Scholar * Braga, M. et
al. Perioperative immunonutrition in patients undergoing cancer surgery—results of a randomized double-blind phase 3 trial. _Arch. Surg._ 134, 428–433 (1999). CAS PubMed Google Scholar *
Mazzone, P. J. & Arroliga, A. C. Lung cancer: preoperative pulmonary evaluation of the lung resection candidate. _Am. J. Med._ 118, 578–583 (2005). PubMed Google Scholar * Epstein, S.
K., Faling, L. J., Daly, B. D. T. & Celli, B. R. Predicting complications after pulmonary resection —preoperative exercise testing vs a multifactorial cardiopulmonary risk index.
_Chest_ 104, 694–700 (1993). CAS PubMed Google Scholar * Smith, T. B., Stonell, C., Purkayastha, S. & Paraskevas, P. Cardiopulmonary exercise testing as a risk assessment method in
non cardio-pulmonary surgery: a systematic review. _Anaesthesia_ 64, 883–893 (2009). CAS PubMed Google Scholar * West, M. A. et al. Cardiopulmonary exercise variables are associated with
postoperative morbidity after major colonic surgery: a prospective blinded observational study. _Br. J. Anaesth._ 112, 665–671 (2014). CAS PubMed Google Scholar * West, M. A. et al.
Validation of preoperative cardiopulmonary exercise testing-derived variables to predict in-hospital morbidity after major colorectal surgery. _Br. J. Surg._ 103, 744–752 (2016). CAS PubMed
Google Scholar * Morikawa, T. et al. Association of CTNNB1 (β-catenin) alterations, body mass index, and physical activity with survival in patients with colorectal cancer. _JAMA_ 305,
1685–1694 (2011). CAS PubMed PubMed Central Google Scholar * Meyerhardt, J. A. et al. Physical activity and survival after colorectal cancer diagnosis. _J. Clin. Oncol._ 24, 3527–3534
(2006). PubMed Google Scholar * Haydon, A. M. M., MacInnis, R. J., English, D. R. & Giles, G. G. Effect of physical activity and body size on survival after diagnosis with colorectal
cancer. _Gut_ 55, 62–67 (2006). CAS PubMed PubMed Central Google Scholar * Galvao, D. A. & Newton, R. U. Review of exercise intervention studies in cancer patients. _J. Clin. Oncol._
23, 899–909 (2005). PubMed Google Scholar * Wang, J. et al. Effect of exercise training intensity on murine T-regulatory cells and vaccination response. _Scand. J. Med. Sci. Sports_ 22,
643–652 (2012). CAS PubMed Google Scholar * Ho, R. T. et al. The effect of t’ai chi exercise on immunity and infections: a systematic review of controlled trials. _J. Altern. Complement.
Med._ 19, 389–396 (2013). PubMed Google Scholar * Bote, M. E., Garcia, J. J., Hinchado, M. D. & Ortega, E. Fibromyalgia: anti-inflammatory and stress responses after acute moderate
exercise. _PLoS One_ 8, e74524 (2013). CAS PubMed PubMed Central Google Scholar * Dranoff, G. Cytokines in cancer pathogenesis and cancer therapy. _Nat. Rev. Cancer_ 4, 11–22 (2004). CAS
PubMed Google Scholar * Lotze, M. T. et al. In vivo administration of purified human interleukin 2. II. Half life, immunologic effects, and expansion of peripheral lymphoid cells in vivo
with recombinant IL 2. _J. Immunol._ 135, 2865–2875 (1985). CAS PubMed Google Scholar * Jiang, T., Zhou, C. & Ren, S. Role of IL-2 in cancer immunotherapy. _Oncoimmunology_ 5,
e1163462 (2016). PubMed PubMed Central Google Scholar * Deehan, D. J., Heys, S. D., Ashby, J. & Eremin, O. Interleukin-2 (IL-2) augments host cellular immune reactivity in the
perioperative period in patients with malignant disease. _Eur. J. Surg. Oncol._ 21, 16–22 (1995). CAS PubMed Google Scholar * Klatte, T. et al. Perioperative immunomodulation with
interleukin-2 in patients with renal cell carcinoma: results of a controlled phase II trial. _Br. J. Cancer_ 95, 1167–1173 (2006). CAS PubMed PubMed Central Google Scholar * Nichols, P.
H., Ramsden, C. W., Ward, U., Sedman, P. C. & Primrose, J. N. Perioperative immunotherapy with recombinant interleukin-2 in patients undergoing surgery for colorectal-cancer. _Cancer
Res._ 52, 5765–5769 (1992). CAS PubMed Google Scholar * Sedman, P. C., Ramsden, C. W., Brennan, T. G., Giles, G. R. & Guillou, P. J. Effects of low-dose perioperative interferon on
the surgically induced suppression of antitumour immune-responses. _Br. J. Surg._ 75, 976–981 (1988). CAS PubMed Google Scholar * Klatte, T. et al. Pretreatment with interferon-α2a
modulates perioperative immunodysfunction in patients with renal cell carcinoma. _Onkologie_ 31, 28–34 (2008). CAS PubMed Google Scholar * Nagano, H. et al. Hepatic resection followed by
IFN-α and 5-FU for advanced hepatocellular carcinoma with tumor thrombus in the major portal branch. _Hepatogastroenterology_ 54, 172–179 (2007). CAS PubMed Google Scholar * Cascinu, S.
et al. Cytokinetic effects of interferon in colorectal-cancer tumors—implications in the design of the interferon/5-fluorouracil combinations. _Cancer Res._ 53, 5429–5432 (1993). CAS PubMed
Google Scholar * Rajala, P. et al. Perioperative single dose instillation of epirubicin or interferon-α after transurethral resection for the prophylaxis of primary superficial bladder
cancer recurrence: a prospective randomized multicenter study—Finnbladder III long-term results. _J. Urol._ 168, 981–985 (2002). CAS PubMed Google Scholar * Schneider, C. et al.
Perioperative recombinant human granulocyte colony-stimulating factor (Filgrastim) treatment prevents immunoinflammatory dysfunction associated with major surgery. _Ann. Surg._ 239, 75–81
(2004). PubMed PubMed Central Google Scholar * Mels, A. K. et al. Immune-stimulating effects of low-dose perioperative recombinant granulocyte–macrophage colony-stimulating factor in
patients operated on for primary colorectal carcinoma. _Br. J. Surg._ 88, 539–544 (2001). CAS PubMed Google Scholar * Licht, A. K., Schinkel, C., Zedler, S., Schinkel, S. & Faist, E.
Effects of perioperative recombinant human IFN-γ (rHuIFN-γ) application in vivo on T cell response. _J. Interferon Cytokine Res._ 23, 149–154 (2003). CAS PubMed Google Scholar * Badwe, R.
A. et al. Timing of surgery during menstrual cycle and survival of premenopausal women with operable breast cancer. _Lancet_ 337, 1261–1264 (1991). CAS PubMed Google Scholar * Wheeldon,
N. M. et al. Influence of sex-steroid hormones on the regulation of lymphocyte β2-adrenoceptors during the menstrual cycle. _Br. J. Clin. Pharmacol._ 37, 583–588 (1994). CAS PubMed PubMed
Central Google Scholar * Ben-Eliyahu, S., Page, G. G., Shakhar, G. & Taylor, A. N. Increased susceptibility to metastasis during pro-oestrus/oestrus in rats: possible role of
oestradiol and natural killer cells. _Br. J. Cancer_ 74, 1900–1907 (1996). CAS PubMed PubMed Central Google Scholar * Shakhar, K., Shakhar, G., Rosenne, E. & Ben-Eliyahu, S. Timing
within the menstrual cycle, sex, and the use of oral contraceptives determine adrenergic suppression of NK cell activity. _Br. J. Cancer_ 83, 1630–1636 (2000). CAS PubMed PubMed Central
Google Scholar * Ben-Eliyahu, S., Shakhar, G., Shakhar, K. & Melamed, R. Timing within the oestrous cycle modulates adrenergic suppression of NK activity and resistance to metastasis:
possible clinical implications. _Br. J. Cancer_ 83, 1747–1754 (2000). CAS PubMed PubMed Central Google Scholar * Page, G. G. & Ben-Eliyahu, S. Increased surgery-induced metastasis
and suppressed natural killer cell activity during proestrus/estrus in rats. _Breast Cancer Res. Treat._ 45, 159–167 (1997). CAS PubMed Google Scholar * Neeman, E. & Ben-Eliyahu, S.
Surgery and stress promote cancer metastasis: new outlooks on perioperative mediating mechanisms and immune involvement. _Brain Behav. Immun._ 30, S32–S40 (2013). PubMed Google Scholar *
Haldar, R., Ricon, I., Cole, S., Zmora, O. and Ben-Eliyahu, S. Perioperative β-adrenergic blockade and COX2 inhibition in colorectal cancer patients improves pro-metastatic indices in the
excised tumor: EMT, tumor infiltrating lymphocytes (TILs), and gene regulatory pathways. Presented at the PNIRS 24th Annual Scientific Meeting (2017). * Hazut, O. et al. The effect of
β-adrenergic blockade and COX-2 inhibition on healing of colon, muscle, and skin in rats undergoing colonic anastomosis. _Int. J. Clin. Pharmacol. Ther._ 49, 545–554 (2011). CAS PubMed
PubMed Central Google Scholar * Benjamin, B. et al. Effect of β blocker combined with COX-2 inhibitor on colonic anastomosis in rats. _Int. J. Colorectal Dis._ 25, 1459–1464 (2010). PubMed
Google Scholar * Karagiannis, G. S. et al. Neoadjuvant chemotherapy induces breast cancer metastasis through a TMEM-mediated mechanism. _Sci. Transl Med._ 9, eaan0026 (2017). PubMed
PubMed Central Google Scholar * Avraham, R. et al. Synergism between immunostimulation and prevention of surgery-induced immune suppression: an approach to reduce post-operative tumor
progression. _Brain Behav. Immun._ 24, 952–958 (2010). CAS PubMed PubMed Central Google Scholar * Elenkov, I. J., Papanicolaou, D. A., Wilder, R. L. & Chrousos, G. P. Modulatory
effects of glucocorticoids and catecholamines on human interleukin-12 and interleukin-10 production: clinical implications. _Proc. Assoc. Am. Physicians_ 108, 374–381 (1996). CAS PubMed
Google Scholar * Whalen, M. M. & Bankhurst, A. D. Effects of β-adrenergic receptor activation, cholera toxin and forskolin on human natural killer cell function. _Biochem. J._ 272,
327–331 (1990). CAS PubMed PubMed Central Google Scholar * Ben-Eliyahu, S., Shakhar, G., Page, G. G., Stefanski, V. & Shakhar, K. Suppression of NK cell activity and of resistance to
metastasis by stress: a role for adrenal catecholamines and β-adrenoceptors. _Neuroimmunomodulation_ 8, 154–164 (2000). CAS PubMed Google Scholar * Diamantstein, T. & Ulmer, A.
Antagonistic action of cyclic-GMP and cyclic-AMP on proliferation of B and T lymphocytes. _Immunology_ 28, 113–119 (1975). CAS PubMed PubMed Central Google Scholar * Sternberg, E. M.
Neural regulation of innate immunity: a coordinated nonspecific host response to pathogens. _Nat. Rev. Immunol._ 6, 318–328 (2006). CAS PubMed PubMed Central Google Scholar * Sacedon,
R., Vicente, A., Varas, A., Jimenez, E. & Zapata, A. G. Early differentiation of thymic dendritic cells in the absence of glucocorticoids. _J. Neuroimmunol._ 94, 103–108 (1999). CAS
PubMed Google Scholar * Shaashua, L. et al. Plasma IL-12 levels are suppressed in vivo by stress and surgery through endogenous release of glucocorticoids and prostaglandins but not
catecholamines or opioids. _Psychoneuroendocrinology_ 42, 11–23 (2014). CAS PubMed PubMed Central Google Scholar * Scheinman, R. I., Cogswell, P. C., Lofquist, A. K. & Baldwin, A. S.
Role of transcriptional activation of IκBαin mediation of immunosuppression by glucocorticoids. _Science_ 270, 283–286 (1995). CAS PubMed Google Scholar * Matyszak, M. K., Citterio, S.,
Rescigno, M. & Ricciardi-Castagnoli, P. Differential effects of corticosteroids during different stages of dendritic cell maturation. _Eur. J. Immunol._ 30, 1233–1242 (2000). CAS PubMed
Google Scholar * Baratelli, F. et al. Prostaglandin E-2 induces FOXP3 gene expression and T regulatory cell function in human CD4+ T cells. _J. Immunol._ 175, 1483–1490 (2005). CAS
PubMed Google Scholar * Sharma, S. et al. Tumor cyclooxygenase-2/prostaglandin E-2-dependent promotion of FOXP3 expression and CD4+CD25+ T regulatory cell activities in lung cancer.
_Cancer Res._ 65, 5211–5220 (2005). CAS PubMed Google Scholar * Stolina, M. et al. Specific inhibition of cyclooxygenase 2 restores antitumor reactivity by altering the balance of IL-10
and IL-12 synthesis. _J. Immunol._ 164, 361–370 (2000). CAS PubMed Google Scholar * Sica, A., Schioppa, T., Mantovani, A. & Allavena, P. Tumour-associated macrophages are a distinct
M2 polarised population promoting tumour progression: potential targets of anti-cancer therapy. _Eur. J. Cancer_ 42, 717–727 (2006). CAS PubMed Google Scholar * Yang, L. et al.
Cancer-associated immunodeficiency and dendritic cell abnormalities mediated by the prostaglandin EP2 receptor. _J. Clin. Invest._ 111, 727–735 (2003). CAS PubMed PubMed Central Google
Scholar * Melamed, R., Bar-Yosef, S., Shakhar, G., Shakhar, K. & Ben-Eliyahu, S. Suppression of natural killer cell activity and promotion of tumor metastasis by ketamine, thiopental,
and halothane, but not by propofol: mediating mechanisms and prophylactic measures. _Anesth. Analg._ 97, 1331–1339 (2003). CAS PubMed Google Scholar * Markovic, S. N., Knight, P. R. &
Murasko, D. M. Inhibition of interferon stimulation of natural killer cell activity in mice anesthetized with halothane or isoflurane. _Anesthesiology_ 78, 700–706 (1993). CAS PubMed
Google Scholar * Siddiqui, R. A. et al. Anticancer properties of propofol-docosahexaenoate and propofol-eicosapentaenoate on breast cancer cells. _Breast Cancer Res._ 7, R645–R654 (2005).
CAS PubMed PubMed Central Google Scholar * Sakaguchi, M., Kuroda, Y. & Hirose, M. The antiproliferative effect of lidocaine on human tongue cancer cells with inhibition of the
activity of epidermal growth factor receptor. _Anesth. Analg._ 102, 1103–1107 (2006). CAS PubMed Google Scholar * Mammoto, T. et al. Infiltration anesthetic lidocaine inhibits cancer cell
invasion by modulating ectodomain shedding of heparin-binding epidermal growth factor-like growth factor (HB-EGF). _J. Cell. Physiol._ 192, 351–358 (2002). CAS PubMed Google Scholar *
Martinsson, T. Ropivacaine inhibits serum-induced proliferation of colon adenocarcinoma cells in vitro. _J. Pharmacol. Exp. Ther._ 288, 660–664 (1999). CAS PubMed Google Scholar *
Sessler, D. I., Ben-Eliyahu, S., Mascha, E. J., Parat, M. O. & Buggy, D. J. Can regional analgesia reduce the risk of recurrence after breast cancer? Methodology of a multicenter
randomized trial. _Contemp. Clin. Trials_ 29, 517–526 (2008). PubMed Google Scholar * Peterson, P. K. et al. Suppression of human peripheral-blood mononuclear cell-function by methadone
and morphine. _J. Infect. Dis._ 159, 480–487 (1989). CAS PubMed Google Scholar * Chao, C. C., Molitor, T. W., Close, K., Hu, S. X. & Peterson, P. K. Morphine inhibits the release of
tumor-necrosis-factor in human peripheral-blood mononuclear cell-cultures. _Int. J. Immunopharmacol._ 15, 447–453 (1993). CAS PubMed Google Scholar * Afsharimani, B., Cabot, P. &
Parat, M. O. Morphine and tumor growth and metastasis. _Cancer Metastasis Rev._ 30, 225–238 (2011). CAS PubMed Google Scholar * Carr, D. J. J., Gebhardt, B. M. & Paul, D. α-Adrenergic
and Mu-2 opioid receptors are involved in morphine-induced suppression of splenocyte natural-killer activity. _J. Pharmacol. Exp. Ther._ 264, 1179–1186 (1993). CAS PubMed Google Scholar
* Carr, D. J., Mayo, S., Gebhardt, B. M. & Porter, J. Central α-adrenergic involvement in morphine-mediated suppression of splenic natural killer activity. _J. Neuroimmunol._ 53, 53–63
(1994). CAS PubMed Google Scholar * Freier, D. O. & Fuchs, B. A. A mechanism of action for morphine-induced immunosuppression: corticosterone mediates morphine-induced suppression of
natural killer cell activity. _J. Pharmacol. Exp. Ther._ 270, 1127–1133 (1994). CAS PubMed Google Scholar * Sacerdote, P., Manfredi, B., Mantegazza, P. & Panerai, A. E.
Antinociceptive and immunosuppressive effects of opiate drugs: a structure-related activity study. _Br. J. Pharmacol._ 121, 834–840 (1997). CAS PubMed PubMed Central Google Scholar *
Rojavin, M. et al. Morphine treatment in-vitro or in-vivo decreases phagocytic functions of murine macrophages. _Life Sci._ 53, 997–1006 (1993). CAS PubMed Google Scholar * Khabbazi, S.,
Nassar, Z. D., Goumon, Y. & Parat, M. O. Morphine decreases the pro-angiogenic interaction between breast cancer cells and macrophages in vitro. _Sci. Rep._ 6, 31572 (2016). CAS PubMed
PubMed Central Google Scholar * Alicea, C., Belkowski, S., Eisenstein, T. K., Adler, M. W. & Rogers, T. J. Inhibition of primary murine macrophage cytokine production in vitro
following treatment with the κ-opioid agonist U50,488H. _J. Neuroimmunol._ 64, 83–90 (1996). CAS PubMed Google Scholar * Wheatley, D. N. Controlling cancer by restricting arginine
availability—arginine-catabolizing enzymes as anticancer. _Anticancer Drugs_ 15, 825–833 (2004). CAS PubMed Google Scholar * Feun, L. & Savaraj, N. Pegylated arginine deiminase: a
novel anticancer enzyme agent. _Expert Opin. Investig. Drugs_ 15, 815–822 (2006). CAS PubMed PubMed Central Google Scholar * Izzo, F. et al. Pegylated arginine deiminase treatment of
patients with unresectable hepatocellular carcinoma: results from phase I/II studies. _J. Clin. Oncol._ 22, 1815–1822 (2004). CAS PubMed Google Scholar * Nanthakumaran, S., Brown, I.,
Heys, S. D. & Schofield, A. C. Inhibition of gastric cancer cell growth by arginine: molecular mechanisms of action. _Clin. Nutr._ 28, 65–70 (2009). CAS PubMed Google Scholar *
Albina, J. E., Caldwell, M. D., Henry, W. L. Jr. & Mills, C. D. Regulation of macrophage functions by L-arginine. _J. Exp. Med._ 169, 1021–1029 (1989). CAS PubMed Google Scholar *
Park, K. G., Hayes, P. D., Garlick, P. J., Sewell, H. & Eremin, O. Stimulation of lymphocyte natural cytotoxicity by L-arginine. _Lancet_ 337, 645–646 (1991). CAS PubMed Google Scholar
* Cho-Chung, Y. S., Clair, T., Bodwin, J. S. & Berghoffer, B. Growth arrest and morphological change of human breast cancer cells by dibutyryl cyclic AMP and L-arginine. _Science_ 214,
77–79 (1981). CAS PubMed Google Scholar * Synakiewicz, A., Stachowicz-Stencel, T. & Adamkiewicz-Drozynska, E. The role of arginine and the modified arginine deiminase enzyme ADI-PEG
20 in cancer therapy with special emphasis on phase I/II clinical trials. _Expert Opin. Investig. Drugs_ 23, 1517–1529 (2014). CAS PubMed Google Scholar * Samid, D., Yeh, A. &
Prasanna, P. Induction of erythroid differentiation and fetal hemoglobin production in human leukemic cells treated with phenylacetate. _Blood_ 80, 1576–1581 (1992). CAS PubMed Google
Scholar * Samid, D. et al. Selective activity of phenylacetate against malignant gliomas: resemblance to fetal brain damage in phenylketonuria. _Cancer Res._ 54, 891–895 (1994). CAS PubMed
Google Scholar * Samid, D., Shack, S. & Myers, C. E. Selective growth arrest and phenotypic reversion of prostate cancer cells in vitro by nontoxic pharmacological concentrations of
phenylacetate. _J. Clin. Invest._ 91, 2288–2295 (1993). CAS PubMed PubMed Central Google Scholar * DeBerardinis, R. J. & Cheng, T. Q’s next: the diverse functions of glutamine in
metabolism, cell biology and cancer. _Oncogene_ 29, 313–324 (2010). CAS PubMed Google Scholar * Salaun, B., Coste, I., Rissoan, M. C., Lebecque, S. J. & Renno, T. TLR3 can directly
trigger apoptosis in human cancer cells. _J. Immunol._ 176, 4894–4901 (2006). CAS PubMed Google Scholar * Adams, S. Toll-like receptor agonists in cancer therapy. _Immunotherapy_ 1,
949–964 (2009). CAS PubMed Google Scholar * Ho, V. et al. TLR3 agonist and sorafenib combinatorial therapy promotes immune activation and controls hepatocellular carcinoma progression.
_Oncotarget_ 6, 27252–27266 (2015). PubMed PubMed Central Google Scholar * Robinson, R. A. et al. Phase 1–2 trial of multiple-dose polyriboinosinic-polyribocytidylic acid in patients with
leukemia or solid tumors. _J. Natl Cancer Inst._ 57, 599–602 (1976). CAS PubMed Google Scholar * Alderson, M. R., McGowan, P., Baldridge, J. R. & Probst, P. TLR4 agonists as
immunomodulatory agents. _J. Endotoxin Res._ 12, 313–319 (2006). CAS PubMed Google Scholar * Coler, R. N. et al. Development and characterization of synthetic glucopyranosyl lipid
adjuvant system as a vaccine adjuvant. _PLoS One_ 6, e16333 (2011). CAS PubMed PubMed Central Google Scholar * Yusuf, N. et al. Protective role of toll-like receptor 4 during the
initiation stage of cutaneous chemical carcinogenesis. _Cancer Res._ 68, 615–622 (2008). CAS PubMed PubMed Central Google Scholar * Spaner, D. E. et al. Immunomodulatory effects of
toll-like receptor-7 activation on chronic lymphocytic leukemia cells. _Leukemia_ 20, 286–295 (2006). CAS PubMed Google Scholar * Dummer, R. et al. An exploratory study of systemic
administration of the Toll-like receptor-7 agonist 852A in patients with refractory metastatic melanoma. _Clin. Cancer Res._ 14, 856–864 (2008). CAS PubMed Google Scholar * Krieg, A. M.
CpG motifs in bacterial DNA and their immune effects. _Annu. Rev. Immunol._ 20, 709–760 (2002). CAS PubMed Google Scholar * Krieg, A. M. Therapeutic potential of Toll-like receptor 9
activation. _Nat. Rev. Drug Discov._ 5, 471–484 (2006). CAS PubMed Google Scholar * Gruenbacher, G. et al. IL-2 costimulation enables statin-mediated activation of human NK cells,
preferentially through a mechanism involving CD56+ dendritic cells. _Cancer Res._ 70, 9611–9620 (2010). CAS PubMed Google Scholar * Van Gool, F. et al. Interleukin-5-producing group 2
innate lymphoid cells control eosinophilia induced by interleukin-2 therapy. _Blood_ 124, 3572–3576 (2014). PubMed PubMed Central Google Scholar * Williams, M. A., Tyznik, A. J. &
Bevan, M. J. Interleukin-2 signals during priming are required for secondary expansion of CD8+ memory T cells. _Nature_ 441, 890–893 (2006). CAS PubMed PubMed Central Google Scholar * Le
Bon, A. et al. Cross-priming of CD8+ T cells stimulated by virus-induced type I interferon. _Nat. Immunol._ 4, 1009–1015 (2003). PubMed Google Scholar * Trinchieri, G. & Santoli, D.
Anti-viral activity induced by culturing lymphocytes with tumor-derived or virus-transformed cells—enhancement of human natural killer cell activity by interferon and antagonistic inhibition
of susceptibility of target-cells to lysis. _J. Exp. Med._ 147, 1314–1333 (1978). CAS PubMed Google Scholar * Bogdan, C., Mattner, J. & Schleicher, U. The role of type I interferons
in non-viral infections. _Immunol. Rev._ 202, 33–48 (2004). CAS PubMed Google Scholar * Okanoue, T. et al. Side effects of high-dose interferon therapy for chronic hepatitis C. _J.
Hepatol._ 25, 283–291 (1996). CAS PubMed Google Scholar * Naik, S. et al. Curative one-shot systemic virotherapy in murine myeloma. _Leukemia_ 26, 1870–1878 (2012). CAS PubMed PubMed
Central Google Scholar * Kottke, T. et al. Broad antigenic coverage induced by vaccination with virus-based cDNA libraries cures established tumors. _Nat. Med._ 17, 854–859 (2011). CAS
PubMed PubMed Central Google Scholar * Russell, S. J., Peng, K. W. & Bell, J. C. Oncolytic virotherapy. _Nat. Biotechnol._ 30, 658–670 (2012). CAS PubMed PubMed Central Google
Scholar * Andtbacka, R. H. I. et al. Final analyses of OPTiM: a randomized phase III trial of talimogene laherparepvec versus granulocyte–macrophage colony-stimulating factor in
unresectable stage III–IV melanoma. _J. Immunother. Cancer_ 7, 145 (2019). PubMed PubMed Central Google Scholar * Carthon, B. C. et al. Preoperative CTLA-4 blockade: tolerability and
immune monitoring in the setting of a presurgical clinical trial. _Clin. Cancer Res._ 16, 2861–2871 (2010). CAS PubMed PubMed Central Google Scholar * Shrikant, P., Khoruts, A. &
Mescher, M. F. CTLA-4 blockade reverses CD8+ T cell tolerance to tumor by a CD4+ T cell-and IL-2-dependent mechanism. _Immunity_ 11, 483–493 (1999). CAS PubMed Google Scholar * Phan, G.
Q. et al. Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. _Proc. Natl Acad. Sci. USA_ 100, 8372–8377
(2003). CAS PubMed PubMed Central Google Scholar * Lee, C. K. et al. Checkpoint inhibitors in metastatic EGFR-mutated non-small cell lung cancer—a meta-analysis. _J. Thorac. Oncol._ 12,
403–407 (2017). PubMed Google Scholar * Dong, H. et al. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. _Nat. Med._ 8, 793–800 (2002). CAS
PubMed Google Scholar * Moslehi, J. J., Salem, J. E., Sosman, J. A., Lebrun-Vignes, B. & Johnson, D. B. Increased reporting of fatal immune checkpoint inhibitor-associated myocarditis.
_Lancet_ 391, 933 (2018). PubMed PubMed Central Google Scholar * Ramalingam, S. et al. Long-term OS for patients with advanced NSCLC enrolled in the KEYNOTE-001 study of pembrolizumab.
_J. Thorac. Oncol._ 11, S241–S242 (2016). Google Scholar * Valzasina, B. et al. Triggering of OX40 (CD134) on CD4+CD25+ T cells blocks their inhibitory activity: a novel regulatory role for
OX40 and its comparison with GITR. _Blood_ 105, 2845–2851 (2005). CAS PubMed Google Scholar * Vu, M. D. et al. OX40 costimulation turns off Foxp3+ tregs. _Blood_ 110, 2501–2510 (2007).
CAS PubMed PubMed Central Google Scholar * Lei, F. Y. et al. Regulation of A1 by OX40 contributes to CD8+ T cell survival and anti-tumor activity. _PLoS One_ 8, e70635 (2013). CAS
PubMed PubMed Central Google Scholar * Song, J. X., So, T. & Croft, M. Activation of NF-κB1 by OX40 contributes to antigen-driven T cell expansion and survival. _J. Immunol._ 180,
7240–7248 (2008). CAS PubMed Google Scholar * Curti, B. D. et al. OX40 is a potent immune-stimulating target in late-stage cancer patients. _Cancer Res._ 73, 7189–7198 (2013). CAS PubMed
PubMed Central Google Scholar * Weinberg, A. D. et al. Anti-OX40 (CD134) administration to nonhuman primates: immunostimulatory effects and toxicokinetic study. _J. Immunother._ 29,
575–585 (2006). CAS PubMed Google Scholar * Montler, R. et al. OX40, PD-1 and CTLA-4 are selectively expressed on tumor-infiltrating T cells in head and neck cancer. _Clin. Transl
Immunol._ 5, e70 (2016). Google Scholar Download references ACKNOWLEDGEMENTS The authors thank the US National Cancer Institute (NCI), the Israel Ministry of Science and the Israeli Science
Foundation for research funding. REVIEWER INFORMATION _Nature Reviews Clinical Oncology_ thanks Bernhard Riedel, Daniel Sessler, Marie-Odile Parat and Rebecca Auer for their contribution to
the peer review of this work. AUTHOR INFORMATION Author notes * These authors contributed equally: Pini Matzner, Elad Sandbank. AUTHORS AND AFFILIATIONS * Neuro-Immunology Research Unit,
School of Psychological Sciences, Tel-Aviv University, Tel Aviv-Yafo, Israel Pini Matzner, Elad Sandbank & Shamgar Ben-Eliyahu * Department of Hematology and Oncology, Kaiser Permanente
Northern California, San Francisco, CA, USA Elad Neeman * Surgical Department, Yitzhak Shamir Medical Center, Be’er Ya’akov, Israel Oded Zmora * Department of Anesthesiology and
Perioperative Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX, USA Vijaya Gottumukkala * Sagol School of Neuroscience, Tel Aviv University, Tel Aviv-Yafo, Israel
Shamgar Ben-Eliyahu Authors * Pini Matzner View author publications You can also search for this author inPubMed Google Scholar * Elad Sandbank View author publications You can also search
for this author inPubMed Google Scholar * Elad Neeman View author publications You can also search for this author inPubMed Google Scholar * Oded Zmora View author publications You can also
search for this author inPubMed Google Scholar * Vijaya Gottumukkala View author publications You can also search for this author inPubMed Google Scholar * Shamgar Ben-Eliyahu View author
publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS All authors contributed equally to all aspects of the article. CORRESPONDING AUTHOR Correspondence to
Shamgar Ben-Eliyahu. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard
to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Matzner, P., Sandbank, E.,
Neeman, E. _et al._ Harnessing cancer immunotherapy during the unexploited immediate perioperative period. _Nat Rev Clin Oncol_ 17, 313–326 (2020). https://doi.org/10.1038/s41571-019-0319-9
Download citation * Accepted: 05 December 2019 * Published: 17 February 2020 * Issue Date: May 2020 * DOI: https://doi.org/10.1038/s41571-019-0319-9 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative
