The delta neutrophil index (dni) as a prognostic marker for mortality in adults with sepsis: a systematic review and meta-analysis
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT We performed a meta-analysis to seek evidence for the usefulness of the delta neutrophil index (DNI) as a prognostic blood biomarker for mortality in the early stage of sepsis in
adults. A literature search was performed using criteria set forth in a predefined protocol. Studies of adults with sepsis that provided a DNI measurement and that had mortality as the
outcome, were included. Review articles, editorials, and non-human studies were excluded. The methodological quality of identified studies was assessed independently by two authors using the
Quality in Prognosis Studies (QUIPS) tool. A total of 1,822 patients from eleven studies were ultimately included. Standardized mean differences between non-survivors and survivors were
compared. An elevated DNI was associated with mortality in patients with sepsis (standardized mean difference [SMD] 1.22; 95% confidence interval 0.73–1.71; I2 = 91%). After excluding two
studies—one that included paediatric patients and one with a disproportionately low mortality rate—heterogeneity was minimized (SMD 0.74, 95% confidence interval 0.53–0.94; I2 = 43%).
Overall, the findings suggest that high DNI values are associated with mortality in septic patients. SIMILAR CONTENT BEING VIEWED BY OTHERS CELL-FREE DNA AS DIAGNOSTIC AND PROGNOSTIC
BIOMARKERS FOR ADULT SEPSIS: A SYSTEMATIC REVIEW AND META-ANALYSIS Article Open access 10 November 2023 THE PROGNOSTIC VALUE OF THE COMBINED NEUTROPHIL-TO-LYMPHOCYTE RATIO (NLR) AND
NEUTROPHIL-TO-PLATELET RATIO (NPR) IN SEPSIS Article Open access 02 July 2024 MACROPHAGE MIGRATION INHIBITORY FACTOR AS A DIAGNOSTIC AND PREDICTIVE BIOMARKER IN SEPSIS: META-ANALYSIS OF
CLINICAL TRIALS Article Open access 13 April 2021 INTRODUCTION Sepsis is a rapidly progressive, life-threatening disease. Accurate and expeditious assessment of sepsis is important for early
administration of antibiotics and removal of the source of infection1,2. In the 2016 version of the sepsis guidelines (Sepsis-3)3, the concept of the systemic inflammatory response syndrome
has been deleted. However, it is important for clinicians to distinguish sepsis from a non-infectious inflammatory response in order to institute appropriate treatment; this requires
reliable diagnostic tools that reflect early changes4,5. Hence, many clinicians have studied the usefulness of blood biomarkers such as C-reactive protein, procalcitonin, and lactate for
early assessment of sepsis and for prognostication, in order to initiate timeous treatment and to prevent rapid progression to multi-organ failure6,7,8,9,10. In infectious conditions, mature
segmented neutrophils normally proliferate to kill bacteria in the host. Simultaneously, the number of circulating immature neutrophils increases; however, these can cause organ failure in
the host11. The increase in the number of circulating immature granulocyte is referred to as ‘a left shift’, defined as an elevated immature/total granulocyte ratio or an elevated neutrophil
band count12,13. In sepsis, this reflects severity and aggravation of the disease course14,15. Although accurate measurement of immature neutrophil numbers is needed as a blood biomarker,
practically, such quantification is not readily accessible16,17. The delta neutrophil index (DNI) is the immature granulocyte fraction provided by a blood cell analyser; it is determined by
subtracting the fraction of mature polymorphonuclear leukocytes from the sum of myeloperoxidase-reactive cells and reflects the number of immature neutrophils as a blood biomarker. This
index is calculated by differentiating two granulocyte measurements; one measured using the cytochemical myeloperoxidase reaction and the other by the nuclear lobularity channel18. Since
measurement of the DNI is reproducible, rapid, and accurate, the DNI has been used as a blood biomarker in patients with sepsis. This systematic review aimed to seek evidence for the
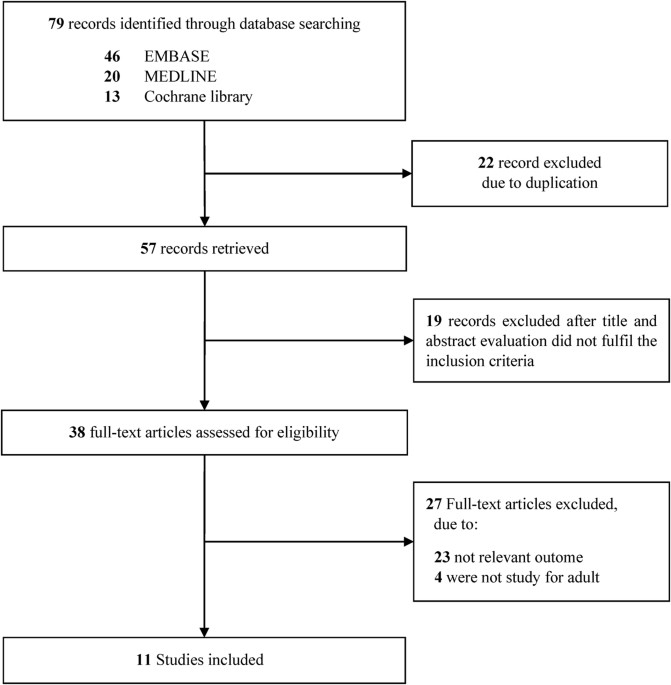
usefulness of the DNI as a prognostic blood biomarker of mortality in patients in the early stage of sepsis. RESULTS STUDY SELECTION AND CHARACTERISTICS The process for identifying eligible
studies is shown in Fig. 1. Searches of the databases identified 79 articles. A total of 57 studies remained after excluding duplicate articles. Of these, 19 articles were excluded because
their titles and abstracts did not fulfil the inclusion criteria at initial screening. The full texts of 38 potentially relevant studies were comprehensively reviewed. Of these, 29 articles
were excluded for the following reasons: non-relevant outcome or non-adult study population. Finally, eleven studies met the criteria and were included in the review; nine were full
publications17,18,19,20,21,22,23,24,25 and two were abstract-only publications26,27. The main characteristics of the eleven eligible publications are shown in Table 1. In addition, details
of the population included in each study are provided in Supplementary Table S1. All included studies were observational, were about sepsis, and had mortality as the main outcome. Ten
studies were conducted in Korea, one was conducted in Egypt. Three studies had as their inclusion criteria, cases of bacteraemia. Eight studies included patients with sepsis or septic shock
while the three remaining studies had subjects with acute kidney injury, acute cholecystitis, and spontaneous bacterial peritonitis, respectively. In seven studies, the time that blood was
sampled to measure the DNI was exactly stated; this detail was unclear or not reported in the other studies. In seven studies, 28-day or 30-day mortality was assessed, whereas two studies
assessed 10-day or in-hospital mortality. In these studies, the mean ± standard deviation (SD) of the DNI value (%) was measured by univariate analysis comparing survivors and non-survivors.
The standardized mean difference (SMD) of the DNI values was calculated, with the 95% confidence interval (CIs). QUALITY OF THE INCLUDED STUDIES In five of the nine studies (among which
methodological quality were conducted), the quality criteria were fulfilled and they were deemed to be of high quality; the other four did not meet at least one criterion. Three studies were
considered of low-quality. Details of our assessment of the quality are presented as Supplementary Figs S1 and S2. Additionally, all four studies which were included to measure the
predictive accuracy of DNI for mortality were considered to be of high-quality (Supplementary Figs S3 and S4). MAIN ANALYSIS Eleven relevant studies including 1,822 patients were analysed.
All of these studies reported differences in DNI values between survivors and non-survivors. In our meta-analysis, the DNI level was found to be significantly higher in non-survivors than in
survivors, demonstrating a positive association with an overall SMD [(mean level in the non-survivor group – mean level in the survivor group)/pooled SD] of 1.22 (95% CI 0.73–1.71; I2 =
91%; _p_ < 0.00001, Fig. 2). After excluding the two abstract-only publications, the SMD of the remaining seven studies was 1.46 (95% CI 0.86–2.06; I2 = 93%; _p_ < 0.00001). SUBGROUP
ANALYSIS AND SENSITIVITY ANALYSIS We performed subgroup analyses according to the inclusion criteria, country of study, sample size, time of outcome assessment, and quality of included
studies (Table 2). In the analysis for inclusion criteria, the SMD of the DNI was 1.28 (95% CI 0.73–16.08) and I2 was 92%. In the analysis for time of outcome assessment, the SMD was 1.61
(95% CI 0.83–2.39) and I2 was 80%. In the subgroup analyses, no item had low heterogeneity. A sensitivity analysis was performed by sequential removal of individual studies to minimize
heterogeneity among the remaining studies. By removing the studies by Zanaty _et al_.20 and Kim _et al_.23, the heterogeneity was minimized to 43% (SMD 0.74, 95% CI 0.53–0.94; I2 = 43%, Fig.
3). PREDICTIVE ACCURACY OF THE DNI FOR MORTALITY Meta-analysis was performed to compare the predictive accuracy of the DNI for mortality. The pooled area under the curve (AUC) based on thr
summary receiver operating characteristic (SROC) curve was 0.82, which demonstrated a good grade of DNI in predicting mortality (Fig. 4). Additionally, the pooled diagnostic odds ratio of
DNI was 9.37 (95% CI 3.74–23.48) (Supplementary Table S2 and Fig. S5). Pooled sensitivity and specificity of DNI value were 0.70 (95% CI 0.60–0.80) and 0.72 (95% CI 0.68–0.75), respectively
(Supplementary Table S2 and Fig. S6). Pooled positive and negative likelihood ratio were also 3.33 (95% CI 1.95–5.69) and 0.41 (95% CI 3.74–23.48), respectively (Supplementary Table S2). The
best thresholds of DNI in predicting mortality were 1.3%, 5.2%, 5.7%, and 7.6% in each included study (Supplementary Table S2). DISCUSSION This systematic review and meta-analysis is the
first to demonstrate that the DNI has prognostic value in adults with sepsis: High DNI values tended to be associated with mortality in septic patients. Since sepsis is a rapidly progressive
and unpredictable disease regardless of the provision of appropriate treatment, the DNI could be a novel prognostic biomarker. Although the level of the DNI was significantly higher in
non-survivors than in survivors, this meta-analysis showed high heterogeneity (SMD 1.22, 95% CI 0.73–1.71; I2 = 91%). To resolve this issue, subgroup analyses were performed for the clinical
parameters thought to be inducing heterogeneity, such as the inclusion criteria used, country in which the studies were performed (Korea vs. Egypt), sample size (≥100 vs. <100), time of
outcome assessment (28-day mortality vs. other), and quality of included studies (high vs. low). Despite these subgroup analyses, high levels of heterogeneity remained (Table 2). After
performing an additional sensitivity analysis by removing studies by Zanaty _et al_.20 and Kim _et al_.23, heterogeneity was minimized (SMD 0.74, 95% CI 0.53–0.94; I2 = 43%, Fig. 3). The
study by Zanaty _et al_.20 did not clearly explain the patient selection in the assessment of quality and had a relatively smaller sample size than the other included studies. In the study
by Kim _et al_.23, the overall mortality in septic patients was exceptionally low at 3.7%; and much lower than that of the other included studies, whose mean estimate of overall mortality
was 32.9%. We assumed that selection bias in the study by Zanaty _et al_.20 and the lower mortality rate in the study by Kim _et al_.23 contributed to the high heterogeneity in this
meta-analysis. Several confounding factors could have affected short-term mortality in this study. First, the use of appropriate antibiotics to treat the focus of infection in patients with
sepsis influences mortality. Empiric broad-spectrum antibiotics should be administered to septic patients as soon as possible. In addition, the time to initiation of antibiotic
administration is usually limited to 3–6 h28,29,30,31. After identification of a pathogen by blood culture, targeted antibiotic therapy should be initiated. However, in the included studies,
data associated with antibiotic therapy were incomplete. Second, the severity of sepsis can affect mortality32,33,34. Previous studies have reported clinical severity scores, such as the
acute physiology and chronic health evaluation (APACHE) and sequential organ failure assessment (SOFA) scores35. These scores can be used in subgroup analysis to resolve the high
heterogeneity issue. However, information on severity scores could not be obtained from the included studies. To diagnose sepsis early and predict mortality, procalcitonin is a promising
biomarker that is widely used in adult patients. Although it is an excellent indicator of sepsis and has high sensitivity, there is controversy around its power to predict mortality36,37.
Pettila _et al_. showed that procalcitonin values differ significantly between survivors and non-survivors38. In the present study, the DNI was not compared with the clinical prediction
indices such as procalcitonin. Hence, the predictive power of DNI for mortality relative to these other indices remains unknown. Nevertheless, we found that the DNI has the potential to
predict mortality in adults with sepsis. Thus, the DNI could be useful in rapidly identifying sepsis and determining whether early intervention to remove the septic focus should be
performed. Further research to evaluate the use of the DNI in combination with other indices (such as procalcitonin) to increase predictive power in the overall assessment of sepsis, are
warranted. In a recent meta-analysis of the DNI by Park _et al_., the DNI was reported to have prognostic impact for mortality in septic patients39. The pooled sensitivity and specificity of
the DNI for death were 0.70 (95% CI 0.56–0.81) and 0.78 (95% CI 0.73–0.83), respectively. The pooled AUC by SROC curve was also 0.84. However, in that meta-analysis, the same population
with two different measures of mortality (10-day and 28-day mortality in the study by Kim, 2014) was included twice39,40. Additionally, inclusion of a paediatric study (Lee, 2013)
contributed to heterogeneity in the population domain as all other included studies were performed with adult subjects41. Therefore, we thought that the prognostic value of the DNI in the
meta-analysis by Park _et al_. was not appropriately evaluated. In our meta-analysis, we made an effort to perform a consistent analysis for a defined population (adult septic patients only)
and a specific outcome (28-day mortality in the subgroup analysis). Our meta-analysis revealed the predictive accuracy of DNI for mortality in adult septic patients. The pooled specificity
(0.72, 95% CI 0.68–0.75) and AUC (0.82) of the DNI for death were a little lower than that reported in the study by Park _et al_.39. We also found that the best threshold value of DNI in
predicting mortality ranged from 1.3% to 7.6%. The DNI is an unfamiliar blood marker; it evaluates infection by calculating the proportion of immature granulocytes. Although the leucocyte
count is commonly and widely used to evaluate inflammation in infectious diseases, it can be affected by inflammation in non-infectious disorders such as rheumatoid arthritis, lupus, and
malignancy42,43,44. In evaluating septic conditions, the DNI is therefore more valuable than the leucocyte count as it reflects the circulating immature granulocyte count irrespective of the
leucocyte count45. Additionally, several studies have found that the DNI has the advantages of accuracy and rapidity in evaluating infection22,23,39. Hence, although the DNI is not widely
used, these characteristics and advantages motivated us to evaluate further its value as a clinical prognostic biomarker. There were several limitations in this study. First, wide
representation was not secured because most included studies were geographically confined to South Korea. The findings of this study might have been different had patients from other
countries with different health care systems or ethnicities been included. Additionally, all studies were single-centre investigations, reducing the generalisability of this study’s
findings, which may therefore not be applied to most patients with sepsis. Additional studies with wider representation are required to yield more robust conclusions. Second, the pooled
outcomes of this study were limited to short-term mortality. None of the included studies presented long-term (6-month or 1-year) mortality rates. Therefore, further studies are required to
evaluate the effect of the DNI as a prognostic factor for long-term mortality in adults with sepsis. In conclusion, our systematic review and meta-analysis found that high DNI values tend to
be associated with mortality in septic patients. METHODS SEARCH STRATEGY AND DATA SOURCES Using the Cochrane review methods46, we performed an extensive database search for studies
evaluating the prognostic significance of the delta neutrophil index (DNI) in adult patients with sepsis. The literature search was performed by two experienced reviewers (Ahn C and Kim W)
on November 21, 2017. We searched MEDLINE, EMBASE, and the Cochrane Library without language restrictions. Additionally, we checked the references of eligible studies to find related
studies. Search keywords were selected following a discussion among all authors; the words decided on were: delta neutrophil, sepsis, systemic inflammatory response syndrome (see
Supplementary Table S3). STUDY SELECTION All identified studies were inputted into Endnote 7.5 reference management software (Thomson Reuters, New York, NY, USA). Two reviewers (Ahn C and
Kim W) independently selected all studies on the basis of predefined selection criteria. The title, abstract, and type of each identified article were checked in the screening stage.
Duplicate articles were excluded after comparing the title, authors, and journal and year of publication of all identified studies. We obtained and assessed the full text of all potentially
relevant studies in Portable Document Format electronic file format. Ultimately, included studies had the following features: (1) they involved adult patients with sepsis, (2) they included
a measurement of the DNI; and (3) survival outcomes (28-day or in-hospital mortality) were assessed. DATA EXTRACTION Three reviewers (Ahn C, Kim W, and Lim TH) independently extracted the
characteristics and outcomes of patients in the included studies. Discrepancies between reviewers were discussed and resolved by consensus. The following variables were extracted: the first
author’s name, year of publication, country in which the study was conducted, inclusion period, equipment used for DNI measurement, study population, inclusion criteria, mortality, and mean
(±SD) DNI level. If the latter was not available, estimated mean (±SD) levels were calculated from median values with interquartile ranges using the method of Wan _et al_.47. If any of these
variables were not described in the studies, we sent relevant questions to the corresponding authors via email. ASSESSMENT OF METHODOLOGICAL QUALITY The methodological quality of nine
identified studies were independently assessed by Ahn C and Kim W with blinding to authorship and journal using the Quality in Prognosis Studies (QUIPS) tool, with values of 2, 1, and 0
considered to be low, unclear, and high risk, respectively48. Studies achieving more than nine points from the sum of each six-item score were considered to be of high quality. Any
unresolved disagreements between reviewers were resolved by discussion or review by the third author. Publication bias was not assessable in these studies. As tests for funnel plot asymmetry
are generally only performed when at least 10 studies are included in a meta-analysis, this was not done in the present study. Additionally, the methodological quality of four identified
studies which include a predictive accuracy for mortality were assessed using the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool49. STATISTICAL ANALYSIS In the main
analysis, we investigated the association between the initial DNI level and mortality among patients with sepsis. The strength of association between DNI and death was measured using the
mean with SD between survivors and non-survivors, using a random effects model. DNI levels across comparison groups were extracted as mean differences with 95% CIs. To estimate
heterogeneity, we estimated the proportion of between-study inconsistency due to the true differences between studies (rather than differences due to random error or chance) using the I2
statistic, with values of 25%, 50%, and 75% considered to be low, moderate, and high, respectively50. We conducted planned subgroup analyses based on inclusion criteria (sepsis/septic shock
or bacteraemia); country (Korea or other); sample size (≥100 or <100 subjects); the time window of mortality assessment (within 28 days or other); the time window of DNI level measurement
(within 24 h or other); and methodological quality of the study (high or low). SROC curve was used to predict mortality in adult septic patients, which also represented the calculated value
of Q* index and AUC. The value of AUC was assessed using the following four AUC categories: more than 0.97 (excellent), from 0.93 to 0.96 (very good), from 0.75 to 0.92 (good), and less
than 0.75 (reasonable but obviously deficient in prognostic accuracy)51. We used Review Manager version 5.3 (Cochrane Collaboration, Oxford, UK) to perform the statistical analysis, and a
_P_-value < 0.05 was considered statistically significant. DATA AVAILABILITY The datasets generated and analysed during the current study are available from the corresponding author on
reasonable request. REFERENCES * Dellinger, R. P. _et al_. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. _Intensive Care Med._
39, 165–228 (2013). Article CAS PubMed Google Scholar * Garnacho-Montero, J. _et al_. Impact of adequate empirical antibiotic therapy on the outcome of patients admitted to the intensive
care unit with sepsis. _Crit. Care Med._ 31, 2742–2751 (2003). Article PubMed Google Scholar * Singer, M. _et al_. The third international consensus definitions for sepsis and septic
shock (sepsis-3). _JAMA._ 315, 801–810 (2016). Article CAS PubMed PubMed Central Google Scholar * Liu, D., Su, L., Han, G., Yan, P. & Xie, L. Prognostic value of procalcitonin in
adult patients with sepsis: a systematic review and meta-analysis. _PLoS One_ 10, e0129450, https://doi.org/10.1371/journal.pone.0129450 (2015). Article PubMed PubMed Central Google
Scholar * Wacker, C., Prkno, A., Brunkhorst, F. M. & Schlattmann, P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. _Lancet Infect. Dis._ 13,
426–435 (2013). Article CAS PubMed Google Scholar * Kim, H., Kim, Y., Lee, H. K., Kim, K. H. & Yeo, C. D. Comparison of the delta neutrophil index with procalcitonin and C-reactive
protein in sepsis. _Clin. Lab._ 60, 2015–2021 (2014). Article CAS PubMed Google Scholar * Behnes, M. _et al_. Diagnostic and prognostic utility of soluble CD 14 subtype (presepsin) for
severe sepsis and septic shock during the first week of intensive care treatment. _Crit. Care_ 18, 507, https://doi.org/10.1186/s13054-014-0507-z (2014). Article PubMed PubMed Central
Google Scholar * Castelli, G. P. _et al_. Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. _Crit. Care_ 8, R234–242 (2004).
Article PubMed PubMed Central Google Scholar * Akpinar, S., Rollas, K., Alagöz, A., Seğmen, F. & Sipit, T. Performance evaluation of MR-proadrenomedullin and other scoring systems
in severe sepsis with pneumonia. _J. Thorac. Dis._ 6, 921–929 (2014). PubMed PubMed Central Google Scholar * Vassiliou, A. G. _et al_. Elevated biomarkers of endothelial
dysfunction/activation at ICU admission are associated with sepsis development. _Cytokine_ 69, 240–247 (2014). Article CAS PubMed Google Scholar * Cornbleet, P. J. Clinical utility of
the band count. _Clin. Lab. Med._ 22, 101–136 (2002). Article PubMed Google Scholar * Seebach, J. D., Morant, R., Rüegg, R., Seifert, B. & Fehr, J. The diagnostic value of the
neutrophil left shift in predicting inflammatory and infectious disease. _Am. J. Clin. Pathol._ 107, 582–591 (1997). Article CAS PubMed Google Scholar * Cavallazzi, R., Bennin, C.-L.,
Hirani, A., Gilbert, C. & Marik, P. E. Review of A Large Clinical Series: Is the Band Count Useful in the Diagnosis of Infection? An Accuracy Study in Critically Ill Patients. _J.
Intensive Care Med._ 25, 353–357 (2010). Article PubMed Google Scholar * Ha, S. O. _et al_. Fraction of immature granulocytes reflects severity but not mortality in sepsis. _Scand. J.
Clin. Lab. Invest._ 75, 36–43 (2015). Article CAS PubMed Google Scholar * Mare, T. A. _et al_. The diagnostic and prognostic significance of monitoring blood levels of immature
neutrophils in patients with systemic inflammation. _Crit. Care_ 19, 57, https://doi.org/10.1186/s13054-015-0778-z (2015). Article PubMed PubMed Central Google Scholar * Ansari-Lari, M.
A., Kickler, T. S. & Borowitz, M. J. Immature granulocyte measurement using the Sysmex XE-2100: relationship to infection and sepsis. _Am. J. Clin. Pathol._ 120, 795–799 (2003). Article
PubMed Google Scholar * Seok, Y. _et al_. Delta neutrophil index: a promising diagnostic and prognostic marker for sepsis. _Shock_ 37, 242–246 (2012). Article CAS PubMed Google
Scholar * Nahm, C. H., Choi, J. W. & Lee, J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. _Ann. Clin. Lab.
Sci._ 38, 241–246 (2008). CAS PubMed Google Scholar * Kim, H. W. _et al_. Delta neutrophil index: could it predict mortality in patients with bacteraemia? _Scand. J. Infect. Dis._ 44,
475–480 (2012). Article PubMed Google Scholar * Zanaty, O. M., Megahed, M., Demerdash, H. & Swelem, R. Delta neutrophil index versus lactate clearance: Early markers for outcome
prediction in septic shock patients. _Alex. J. Med._ 48, 327–333 (2012). Article Google Scholar * Hwang, Y. J. _et al_. Newly designed delta neutrophil index–to–serum albumin ratio
prognosis of early mortality in severe sepsis. _Am. J. Emerg. Med._ 33, 1577–1582 (2015). Article PubMed Google Scholar * Han, I. M. _et al_. Delta neutrophil index is an independent
predictor of mortality in septic acute kidney injury patients treated with continuous renal replacement therapy. _BMC Nephrol._ 18, 94, https://doi.org/10.1186/s12882-017-0507-8 (2017).
Article PubMed PubMed Central Google Scholar * Kim, H. _et al_. Usefulness of the delta neutrophil index as a promising prognostic marker of acute cholangitis in emergency departments.
_Shock_ 47, 303–311 (2017). Article PubMed Google Scholar * Kim, H. W. _et al_. Delta neutrophil index as a prognostic marker of early mortality in gram negative bacteremia. _Infect.
Chemother._ 46, 94–102 (2014). Article CAS PubMed PubMed Central Google Scholar * Lim, T. S. _et al_. Use of the delta neutrophil index as a prognostic factor of mortality in patients
with spontaneous bacterial peritonitis: Implications of a simple and useful marker. _PLoS One_ 9, e86884 (2014). Article ADS PubMed PubMed Central Google Scholar * Kim, H. Y. _et al_.
Clinical significance of delta neutrophil index in patients with sepsis. _Clin. Microbiol. Infect._ 17, S818, https://doi.org/10.1111/j.1469-0691.2011.03559.x (2011). Article Google Scholar
* Shin, H. J. Usefulness of delta neutrophil index (DNI) for SIRS patient in emergency department. _Crit. Care Med._ 39, 103, https://doi.org/10.1097/01.ccm.0000408627.24229.88 (2011).
Article Google Scholar * Ferrer, R. _et al_. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based
performance improvement program. _Crit. Care Med._ 42, 1749–1755 (2014). Article CAS PubMed Google Scholar * Ferrer, R. _et al_. Effectiveness of treatments for severe sepsis: a
prospective, multicenter, observational study. _Am. J. Respir. Crit. Care Med._ 180, 861–866 (2009). Article CAS PubMed Google Scholar * Rivers, E. _et al_. Early interventions in severe
sepsis and septic shock: a review of the evidence one decade later. _Minerva Anestesiol._ 78, 712–724 (2012). CAS PubMed Google Scholar * Gaieski, D. F. _et al_. Impact of time to
antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. _Crit. Care Med._ 38, 1045–1053 (2010).
Article PubMed Google Scholar * Mikkelsen, M. E. _et al_. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. _Crit. Care Med._ 37,
1670–1677 (2009). Article CAS PubMed Google Scholar * Angus, D. C. _et al_. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of
care. _Crit. Care Med._ 29, 1303–1310 (2001). Article CAS PubMed Google Scholar * Wichmann, M., Inthorn, D., Andress, H.-J. & Schildberg, F. Incidence and mortality of severe sepsis
in surgical intensive care patients: the influence of patient gender on disease process and outcome. _Intensive Care Med._ 26, 167–172 (2000). Article CAS PubMed Google Scholar * Rhodes,
A. _et al_. The surviving sepsis campaign bundles and outcome: results from the international multicentre prevalence study on sepsis (the IMPreSS study). _Intensive Care Med._ 41, 1620–1628
(2015). Article PubMed Google Scholar * Kibe, S., Adams, K. & Barlow, G. Diagnostic and prognostic biomarkers of sepsis in critical care. _J. Antimicrob. Chemother._ 66(Suppl 2),
ii33–ii40, https://doi.org/10.1093/jac/dkq523 (2011). CAS PubMed Google Scholar * Ruiz-Alvarez, M. J. _et al_. Diagnostic efficacy and prognostic value of serum procalcitonin
concentration in patients with suspected sepsis. _J. Intensive Care Med._ 24, 63–71 (2009). Article CAS PubMed Google Scholar * Pettilä, V., Hynninen, M., Takkunen, O., Kuusela, P. &
Valtonen, M. Predictive value of procalcitonin and interleukin 6 in critically ill patients with suspected sepsis. _Intensive Care Med._ 28, 1220–1225 (2002). Article PubMed Google
Scholar * Park, J. H. _et al_. Delta neutrophil index (DNI) as a novel diagnostic and prognostic marker of infection: a systematic review and meta-analysis. _Inflamm. Res._ 66, 863–870
(2017). Article CAS PubMed Google Scholar * Kim, H. W. _et al_. Delta neutrophil index as a prognostic marker of early mortality in gram negative bacteremia. _Infect. Chemother._ 46,
94–102 (2014). Article CAS PubMed PubMed Central Google Scholar * Lee, S. M. _et al_. Usefulness of the delta neutrophil index for assessing neonatal sepsis. _Acta Paediatr._ 102,
e13–16, https://doi.org/10.1111/apa.12052 (2013). Article PubMed Google Scholar * Abramson, N. & Melton, B. Leukocytosis: basics of clinical assessment. _Am. Fam. Physician_ 62,
2053–2060 (2000). CAS PubMed Google Scholar * Pyo, J. Y. _et al_. Delta neutrophil index as a marker for differential diagnosis between flare and infection in febrile systemic lupus
erythematosus patients. _Lupus_ 22, 1102–1109 (2013). Article CAS PubMed Google Scholar * Pyo, J. Y. _et al_. Delta neutrophil index contributes to the differential diagnosis between
acute gout attack and cellulitis within 24 hours after hospitalization. _Rheumatology (Oxford)_ 56, 795–801 (2017). Google Scholar * Shin, D. H., Kim, E. J., Kim, S. J., Park, J.-Y. &
Oh, J. Delta neutrophil index as a marker for differential diagnosis between acute graft pyelonephritis and acute graft rejection. _PLoS One_ 10, e0135819,
https://doi.org/10.1371/journal.pone.0135819 (2015). Article PubMed PubMed Central Google Scholar * Higgins, J. P. & Green, S. _Cochrane handbook for systematic reviews of
interventions. Version 5.1.0_. (The Nordic Cochrane Centre, Copenhagen, 2011). * Wan, X., Wang, W., Liu, J. & Tong, T. Estimating the sample mean and standard deviation from the sample
size, median, range and/or interquartile range. _BMC Med. Res. Methodol._ 14, 135, https://doi.org/10.1186/1471-2288-14-135 (2014). Article PubMed PubMed Central Google Scholar * Hayden,
J. A., van der Windt, D. A., Cartwright, J. L., Côté, P. & Bombardier, C. Assessing bias in studies of prognostic factors. _Ann. Intern. Med._ 158, 280–286 (2013). Article PubMed
Google Scholar * Whiting, P. F. _et al_. Quadas-2: A revised tool for the quality assessment of diagnostic accuracy studies. _Ann. Intern. Med._ 155, 529–536 (2011). Article PubMed Google
Scholar * Higgins, J. & Thompson, S. G. Quantifying heterogeneity in a meta‐analysis. _Stat. Med._ 21, 1539–1558 (2002). Article PubMed Google Scholar * Jones, C. M. &
Athanasiou, T. Summary Receiver Operating Characteristic Curve Analysis Techniques in the Evaluation of Diagnostic Tests. _Ann. Thorac. Surg._ 79, 16–20 (2005). Article PubMed Google
Scholar Download references ACKNOWLEDGEMENTS This research was supported by the Research Program to Solve Social Issues of the National Research Foundation of Korea (NRF) funded by the
Ministry of Science and ICT. (NRF-2015M3C8A8073386). Additionally, we would like to thank Editage (www.editage.com) for English language editing. AUTHOR INFORMATION Author notes * Chiwon Ahn
and Wonhee Kim contributed equally to this work. AUTHORS AND AFFILIATIONS * Department of Emergency Medicine, Armed Forces Yangju Hospital, Yangju, Korea Chiwon Ahn * Department of
Biomedical Engineering, Graduate School of Medicine, Hanyang University, Seoul, Korea Chiwon Ahn, Wonhee Kim & Youngsuk Cho * Department of Emergency Medicine, College of Medicine,
Hallym University, Chuncheon, Korea Wonhee Kim & Youngsuk Cho * Department of Emergency Medicine, College of Medicine, Hanyang University, Seoul, Korea Tae Ho Lim * Department of
Neurosurgery, College of Medicine, Hanyang University, Seoul, Korea Kyu-Sun Choi * Department of Preventive Medicine, College of Korean Medicine, Kyung Hee University, Seoul, Korea Bo-Hyoung
Jang Authors * Chiwon Ahn View author publications You can also search for this author inPubMed Google Scholar * Wonhee Kim View author publications You can also search for this author
inPubMed Google Scholar * Tae Ho Lim View author publications You can also search for this author inPubMed Google Scholar * Youngsuk Cho View author publications You can also search for this
author inPubMed Google Scholar * Kyu-Sun Choi View author publications You can also search for this author inPubMed Google Scholar * Bo-Hyoung Jang View author publications You can also
search for this author inPubMed Google Scholar CONTRIBUTIONS C. Ahn, W. Kim and T.H. Lim conceived the study and designed the review. C. Ahn and T.H. Lim obtained research funding. B.H. Jang
and C. Ahn performed the searches and screened studies for eligibility. W. Kim, Y. Cho, and K.-S. Choi assessed the quality of the papers and performed the statistical analysis. C. Ahn and
W. Kim drafted the manuscript, and all authors contributed substantially to its revision. T.H. Lim takes responsibility for the paper as a whole. CORRESPONDING AUTHOR Correspondence to Tae
Ho Lim. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE: Springer Nature remains neutral with regard to
jurisdictional claims in published maps and institutional affiliations. ELECTRONIC SUPPLEMENTARY MATERIAL SUPPLEMENTARY FIGURES AND TABLES RIGHTS AND PERMISSIONS OPEN ACCESS This article is
licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give
appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in
this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative
Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a
copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Ahn, C., Kim, W., Lim, T.H. _et al._ The delta
neutrophil index (DNI) as a prognostic marker for mortality in adults with sepsis: a systematic review and meta-analysis. _Sci Rep_ 8, 6621 (2018). https://doi.org/10.1038/s41598-018-24211-7
Download citation * Received: 30 November 2017 * Accepted: 23 March 2018 * Published: 26 April 2018 * DOI: https://doi.org/10.1038/s41598-018-24211-7 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative
