Diabetes knowledge predicts hba1c levels of people with type 2 diabetes mellitus in rural china: a ten-month follow-up study
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

ABSTRACT Improving diabetes self-management (DSM) is facing real-world challenges among people with type 2 diabetes mellitus (T2DM) who have a low education level in resource-limited areas.
This study aimed to investigate whether diabetes knowledge could predict glycemic levels in people with T2DM in rural China. This analytical cross-sectional study recruited 321 people with
T2DM from eight villages by purposive sampling at baseline. After 10 months, 206 patients completed the follow-up survey and HbA1c tests, with a response rate of 64.17% (206/321). Multiple
regression analysis was employed to explore the correlation between diabetes knowledge and HbA1c levels. The patient's diabetes knowledge was significantly negatively correlated with
HbA1c levels before and after controlling for covariates in both hierarchical multiple regression and multiple logistic regression (_p_ < 0.01). In addition, other influencing factors,
including sex, age, marital status, employment status, income, and HbA1c levels at baseline, were also identified. Diabetes knowledge could predict HbA1c levels significantly among patients
with low education levels in rural China. Therefore, interventions on improving diabetes knowledge need to be strengthened for patients in rural China so that they can improve their health
outcomes and reduce the disease burden. SIMILAR CONTENT BEING VIEWED BY OTHERS POOR SELF-CARE PRACTICES AND CONTRIBUTING FACTORS AMONG ADULTS WITH TYPE 2 DIABETES IN ADAMA, ETHIOPIA Article
Open access 13 June 2024 MAGNITUDE AND PREDICTORS OF POOR GLYCEMIC CONTROL IN PATIENTS WITH DIABETES AT JIMMA MEDICAL CENTER, ETHIOPIA Article Open access 24 September 2023 LIFESTYLE
MODIFICATION AND MEDICATION USE AMONG DIABETES MELLITUS PATIENTS ATTENDING JIMMA UNIVERSITY MEDICAL CENTER, JIMMA ZONE, SOUTH WEST ETHIOPIA Article Open access 27 March 2023 INTRODUCTION The
prevalence of type 2 diabetes mellitus (T2DM) has sharply increased in the past four decades1. Diabetes and its complications not only seriously affect patients’ health but also bring huge
economic burdens to patients, their families, and society. In 2019, China’s medical expenditures related to diabetes reached $109 billion, ranking second in the world2. To prevent and
control diabetes, numerous studies were conducted and confirmed that lifestyle factors could influence patients’ health outcomes3,4,5. Furthermore, several studies, which were conducted in
China, Finland, and America, found that lifestyle interventions, including diet and exercise, can postpone the onset of T2DM, reduce the incidence of diabetes complications, and ultimately
increase the life expectancy of people with T2DM6,7,8,9,10,11. To apply existing and extensive evidence to manage diabetes in primary care, the International Diabetes Federation (IDF)
emphasized that the cornerstone of T2DM management is to improve diabetes self-management (DSM) ability, including diet, medication adherence, physical activity, and healthy body weight and
has produced a series of guidelines on diabetes management, prevention, and care12,13. China has the largest number of people with diabetes1 and thus may face the considerable challenge of
chronic complications in the future. The government has already paid much attention to managing diabetes and enacted the _policy of equalization of basic public health services_ in 200914.
In rural China, people with T2DM are targeted as the key population for chronic disease management and the specific measures include regular quarterly follow-ups, free fasting blood glucose
(FBG) tests, an annual comprehensive health examination, health education, and different medical prescriptions for people with T2DM15. Although the policy has been implemented for almost 12
years, the challenge related to diabetes prevention and control remains large and serious16,17. A recent study estimated that only 49.2% of treated patients achieved successful glycemic
control in China (HbA1c levels ≤ 7.0%)18. Another study showed that patients’ DSM behavior scores were at a lower-middle level in a suburban hospital in Beijing19. Similarly, a study
conducted in Shandong Province found that, compared with patients from urban areas, patients from rural areas had poorer DSM behaviors20. Patients in rural China are facing greater
difficulties and challenges than those in urban areas because of their lower education levels21 and an unbalanced distribution of high-quality medical resources22. Therefore, improving the
DSM of people with T2DM through educational interventions in rural China should be a top priority now and in the future23. HbA1c, which reflects average plasma glucose over 2 to 3 months
preceding the test, has been not only considered as a biomarker for the presence and severity of hyperglycemia, implying diabetes or pre-diabetes24, but also considered as a risk factor
marker for diabetes-related complications25 in the process of diabetes treatment and management. Serval studies indicated that high HbA1c variability is not only associated with
cardiovascular complications of T2DM26,27 but also associated with increased risk of all-cause and cardiovascular mortality25. Therefore, HbA1c was used as a biochemical marker of glucose
regulation in people with T2DM28, and it was also an outcome variable in the diabetes prevention intervention program29. Similarly, HbA1c will also be an important outcome variable in our
future intervention studies, aiming to reflect glycemic management in patients with diabetes. Before the intervention, the relationship between diabetes knowledge and HbA1c levels should be
cleared. Although there have been a few studies investigating the effects of the policy30,31, which indicated changes in diabetes knowledge, medication compliance, DSM, and HbA1c levels,
little attention has been given to further exploring the association between diabetes knowledge and HbA1c levels in patients in rural China. Besides, these studies have used cross-sectional
data32,33,34, which cannot do the causal inference. Therefore, this analytical cross-sectional study aimed to investigate whether diabetes knowledge could predict the HbA1c levels of people
with T2DM who have a low education level in rural China based on tracking data. MATERIALS AND METHODS PARTICIPANTS The baseline survey was conducted from January 4 to January 17, 2020, in
eight villages of three towns in DaFeng District, Jiangsu Province. Participants who were diagnosed with T2DM based on their electronic health records in each village clinic were involved in
this study. Inclusion criteria: (1) a diagnosis of T2DM from a hospital at a secondary level and above, based on _Guidelines for the Prevention and Treatment of Type 2 Diabetes in China_35;
(2) 18 years old and above; and (3) continuous residence for more than one year. Exclusion criteria included the inability to participate due to physical/mental disabilities or cognitive
impairment. Eventually, a sample of 321 participants was recruited into the study. SAMPLING In China, there is a five-tier administrative system, including provinces, cities,
counties/districts, towns, and villages/communities36. Purposive sampling was employed in this study: (1) Dafeng District was chosen as the site because it is highly representative from the
perspective of economic development level and is a National Demonstration Area for comprehensive prevention and control of chronic diseases37. (2) Three towns, including W town, X town, and
D town, were selected based on the results of the performance assessment conducted by the local health bureau. (3) Two villages from W town, four villages from X town, and one village from D
town were selected based on the population size of the town. (4) All people with T2DM who registered in the village clinic and met the inclusion criteria were interviewed face-to-face by
trained interviewers. Since there were no related studies on the effect size between diabetes knowledge and HbA1c, we chose a small effect size (0.15)38 to achieve a maximum sample size. A
priori G*power 3.139 calculations revealed a minimum sample size of 117 participants within a multiple regression analysis with 5 predictors to detect a small effect size, using α = 0.05,
power (1-β) = 0.90, and effect size = 0.15. Taking into account a 20% loss-to-follow-up rate, the final total sample size was 141 participants. PROCEDURE FOR FIELD SURVEY The patients who
volunteered to participate in the study were invited to village clinics, and four well-educated graduate students conducted the self-report questionnaire. The village doctors at village
clinics were responsible for the HbA1c test. Considering that most participants, with low levels of education, cannot speak Mandarin, four trained volunteers from a local voluntary
organization were invited to solve dialect barriers. Three hundred and twenty-one participants completed the baseline survey. Ten months later, 206 participants completed the follow-up
investigation and received HbA1c tests, and the attrition rate was 35.83% (115/321). There were no significant differences between the follow-up samples and loss to follow-up samples sample
in terms of age (t = −0.504, _p_ = 0.630), HbA1c level at baseline (t = 0.520, _p_ = 0.603), and diabetes knowledge (t = −0.512, _p_ = 0.609), except that the higher proportion of females
was found in respondents (χ2 = 10.137, _p_ = 0.001). Therefore, the loss to follow-up did not affect the stability of the relationship between diabetes knowledge and HbA1c levels.
MEASUREMENTS DEMOGRAPHIC INFORMATION AND CLINICAL CHARACTERISTICS The information, including age, sex, education level, marital status, employment status, and annual household income, was
collected during the baseline survey. Clinical characteristics, including a family history of diabetes, body mass index (BMI), duration of diabetes, hypoglycemia, and diabetes complications,
including hypertension, cardiac disease, diabetic nephropathy, diabetic retinopathy, diabetic peripheral angiopathy, and others, were obtained from the electronic health record system at
township health centers. DIABETES KNOWLEDGE Diabetes knowledge was assessed by the modified 20-item Diabetes Knowledge scale at baseline, which combined the original version of Diabetes
Knowledge scale (DKN)40 with the Chinese version of DKN scale41. Taking into account the literacy level and lifestyle of the participants, we fine-tuned the scale. The process can be found
in the Appendix. The final version of the DKN scale consisted of 17 single-choice items and 3 multiple-choice items. Each item is assigned a score of one for a correct answer and 0 for an
incorrect or unknown response. A higher score suggested a higher level of diabetes knowledge. Cronbach’s alpha of the modified 20-item DKN scale in this sample was 0.73. HBA1C TEST HbA1c
level reflects the average blood glucose concentrations for the preceding 2–3 months in patients42,43. In this study, HbA1c levels were tested, at baseline (T1) and 10-month (T2) follow-up
surveys, by using the portable HbA1c meter and the Diagnosis Kit for Human Glycosylated Hemoglobin (Botangping in Chinese). MEDICATION ADHERENCE Medication adherence was measured at T2 using
a self-designed questionnaire based on a thesis about medication adherence in Chinese people with heart failure44, which includes eight items concerning the situation of forgetting to take
medicine (four items), unauthorized withdrawal of taking medicine (two items), and perceived difficulty in taking prescribed medication (one item). Each item was designed with a five-point
scale ranging from 1 to 5, and the total score was 40. If a participant’s score was equal to 40, it was defined as “medication adherence”; otherwise, it was defined as “medication
nonadherence”. In this study, Cronbach’s alpha of the self-designed questionnaire was 0.93. DIABETES SELF-MANAGEMENT An adapted version of the Diabetes Self-care Activities (SDSCA) measure,
which consists of items covering diet, exercise, blood sugar testing, foot care, and smoking, was used to assess the level of DSM in this study45. After the pilot study, some changes were
made as follows: (1) The term “checking your foot” was removed because participants could not understand and communicate the true meaning. (2) Several specific food names were supplemented
behind the word “high-fat food” to ensure participants’ better understanding of the item. Finally, the adapted version of the SDSCA measure included 7 items from three dimensions, and all
items were measured on an eight-point scale ranging from 0 to 7. Of these, five items were about diet, one item was about exercise, and one item was about self-monitoring blood glucose
(SMBG). If a participant exercised three days or more a week, he or she was deemed to have a high level of DSM; otherwise, he or she had a low level of DSM. Similarly, examining FBG twice a
week or more was defined as a high level of SMBG; otherwise, it was a low level. STATISTICAL ANALYSIS To test the selection bias of the sample, Student's t-tests and Pearson’s
Chi-squared tests were performed to compare the differences in sociodemographic characteristics and clinical factors between the follow-up samples and the loss to follow-up samples. Multiple
regression analysis was conducted to explore the correlation between diabetes knowledge and HbA1c levels (T2) after adjusting for sociodemographic characteristics, clinical factors, and
DSM. Then multiple logistic regression analysis was employed to test the stability of the relationship between diabetes knowledge and HbA1c levels. Concurrently, regression diagnosis was
conducted to examine the robustness of models. First, the residual of the two models was predicted to draw a scatter plot. The relationship between diabetes knowledge and HbA1c levels was
linear. Second, eight kinds of indices were calculated to identify singular values. Seventeen singular values were found and were excluded. Third, the dependent variable satisfied a normal
distribution after removing singular values. Additionally, the variance inflation factors (VIFs) of all independent variables were less than 10, which indicated that collinearity did not
exist. Furthermore, the final model passed the White test, which confirmed that there was no heteroscedasticity. Finally, by calculating the cluster robust standard error, the final model
satisfied the assumption of no autocorrelation. Two individuals had missing values on BMI, which we calculated by their weight and height provided in electronic health records. Therefore,
206 participants with complete data were included in the final analyses. All analyses were conducted in Stata 14.0, and a p-value of < 0.05 was considered statistically significant.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE Ethical approval for this study was obtained from the China Ethics Committee of Registering Clinical Trials (ChiECRCT-20180073) on June 8, 2018.
All patients provided informed consent prior to the questionnaire and interview, all personal information was kept confidential, and reporting was made anonymously. All methods were carried
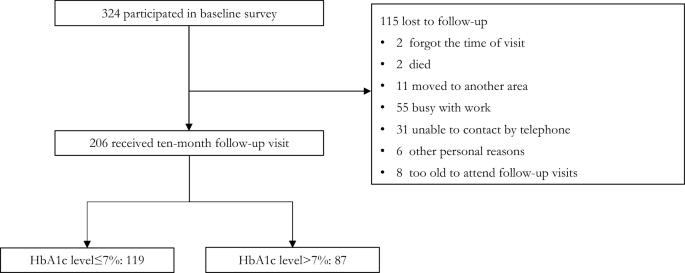
out in accordance with relevant guidelines and regulations. RESULTS PARTICIPANT CHARACTERISTICS As shown in Fig. 1, among the participants who completed the follow-up visits, the average
follow-up time was 319.25 days (SD = 10.90), which was around 10 months. The reasons why 115 participants were loss to follow-up can also be seen in Fig. 1. The sociodemographic
characteristics of the respondents are shown in Table 1. Of 206 respondents, 88.83% were married and 56.8% were farmers. Most of them had a low level of education, with 25.24% being
illiterate, and 36.97% only completing primary school. A majority (83.98%) had an annual household income of no more than 50,000 yuan. CLINICAL CHARACTERISTICS As shown in Table 2, the
average duration of diabetes was 8.11 years (SD = 5.53), with a range of 1–32 years among 206 respondents. Furthermore, 73.3% suffered from diabetes complications, and the top three
complications were cardiovascular disease (72.82%), cerebrovascular disease (0.09%), and diabetic peripheral neuropathy (0.08%). No significant differences were found between the follow-up
samples and loss follow-up samples sample in terms of family history of diabetes, hypoglycemia, the number of complications, duration, BMI, HbA1c levels at baseline, or diabetes knowledge.
RELATIONSHIPS BETWEEN HBA1C LEVELS AND CLINICAL OUTCOMES As shown in Table 3, in terms of diabetes knowledge at baseline, although the mean score of the respondents with HbA1c levels < 7%
(Mean = 10.25, SD = 3.36) was higher than that of the respondents with HbA1c levels ≥ 7% (Mean = 9.83, SD = 3.50), no significant difference was found. Additionally, the mean score for
medication adherence was 7.59 (SD = 1.34), ranging from 0 to 8. For the follow-up sample, 90.78% of them were classified as low-level SMBG, which means that they tested blood glucose less
than twice a week. There were no significant differences between the respondents with HbA1c levels < 7% and respondents with HbA1c levels ≥ 7% in terms of medication adherence, DSM in
diet, and SMBG. As reported in Table 4 and Supplementary Table S2, medication adherence and DSM factors did not influence HbA1c levels significantly in either the multiple linear regression
model or the logistic regression model. DIABETES KNOWLEDGE AS A PREDICTOR OF HBA1C LEVELS AT T2 As shown in Table 4, in Model 1, the inclusion of sex, age, education, marital status,
employment status, and annual household income account for 10.5% of the total variance of HbA1c levels (T2). The combined effect of clinical outcomes at baseline explained an additional
54.9% of the total variance in Model 2. Model 3 indicated that diabetes knowledge was a crucial predictor of HbA1c levels (β = −0.063, _p_ < 0.01), by itself, explaining an additional
1.7% of the total variance. In Model 4 and Model 5, medication adherence and DSM were entered into the multiple regression analyses, and diabetes knowledge was still a significant predictor
factor for HbA1c levels (β = −0.065, _p_ < 0.01; β = −0.062, _p_ < 0.01). Besides, sex (β = −0.669, _p_ < 0.001), age (β = −0.024, _p_ < 0.05), employment status (β = −0.296, _p_
< 0.05), annual household income (β = 0.473, _p_ < 0.05), and HbA1c levels (T1) (β = 0.828, _p_ < 0.001) significantly influenced the HbA1c levels at T2. To further investigate the
stability of the relationship between diabetes knowledge and HbA1c levels and to explore which factors influenced successful glycemic control, we divided the participants into two groups
according to their HbA1c levels (T2), with a cut-off point of HbA1c levels less than 7%46. If the HbA1c level(T2) was less than 7%, he or she had successful glycemic control, and not vice
versa. Similarly, the covariates were input into the logistic regression model in five steps. Supplementary Table S1 showed that sex, marital status, employment status, HbA1c levels(T1), and
diabetes knowledge significantly influenced HbA1c levels(T2). Female respondents were more likely to control glycemia successfully. The married respondents had higher risks of unsuccessful
glycemic control than single respondents. Compared with people engaged in other jobs, respondents who were farmers were more likely to control glycemia successfully. Apparently, in the
multiple logistic regression model, those respondents who had a higher score of diabetes knowledge would have a greater chance of controlling glycemia successfully. DISCUSSION In this study,
we investigated the correlation between diabetes knowledge and HbA1c levels in people with T2DM based on tracking data in rural China. We found that diabetes knowledge could predict HbA1c
levels before and after adjusting for sociodemographic, clinical, and behavioral variables. Furthermore, multiple logistic regression analysis confirmed the results. It was consistent with
the results of a study also conducted in Jiangsu Province, which found that improving diabetes knowledge helps lower FBG levels after a one-year educational intervention47. The results of
this study may suggest that improving diabetes knowledge leads to a decrease in HbA1c levels. The correlation can be explained by knowledge, attitude, and practices (KAP), which has been
applied to health education practice since the 1960s. For people with T2DM, receiving ongoing diabetes health education can improve their understanding of diabetes and help them establish an
active attitude toward treatments. Patients’ active attitudes may enable them to change their DSM behaviors and further influence the HbA1c levels. However, the coefficient of diabetes
knowledge may not be very high in the multiple linear regression model. Reviewing previous studies, a study estimated that every time the patients answered one more question, the HbA1c level
decreased by 0.23948. Another study found that 82% of participants had HbA1c > 7%, which was associated with poor diabetes knowledge. Additionally, a systematic review concluded that
continuous and regular education could result in a mean reduction of 2.02% for HbA1c among Chinese patients49. In contrast, a study conducted in an urban area in China found that there was
no significant difference in the knowledge scores between people with HbA1c < 7% and those with HbA1c ≥ 7%32. Another study revealed that after a two-year educational intervention, there
was no significant difference in FBG levels between treatment and control groups50. These findings were inconsistent, which suggested that the relationship between diabetes knowledge and
glycemic control is worthy of further study. There are two reasons why the coefficient of diabetes knowledge is not very high. On the one hand, as in previous studies51, there is still a
large gap between knowledge and behaviors related to glycemic control, and attitudes or undiscovered factors may play an essential role in the process. On the other hand, several
sociodemographic variables also influenced the HbA1c level significantly in Model 5. First, female patients’ HbA1c levels (T2) were lower than those of males, and female patients were more
likely to successfully control glycemia. It was not consistent with results obtained from other studies52,53,54,55. Some studies found that there was no sex difference in glycemic
control54,55, and other studies concluded that females were less likely to achieve the target HbA1c of < 7%52,53. Although females had better self-care and high levels of adherence53,
depression was more common in females than males, which made it more difficult for women to successfully control glycemia56. These studies were mostly conducted in urban areas; however, the
setting of this study was a rural area. There are many differences between urban and rural areas, such as economic and cultural factors, which may influence the sex differences in glycemic
control. In rural China, females need to do both farm work and housework, while males are mainly busy with farm work and rarely do housework. Thus, the total amount of exercise of females
may be higher than that of males, which increases the possibility of females achieving success in glycemic control. Second, older patients may have lower HbA1c levels since older patients
have more time to focus on their health, while younger patients are busy dealing with work and family. Third, patients who are farming had lower HbA1c levels than patients in other jobs
because farmers perform more physical activities than other jobs. In addition, compared with people whose monthly income is less than 5,000 yuan, people whose monthly income is 5,000–10,000
yuan had lower HbA1c levels, as patients were capable of paying medical bills. Similarly, sex, employment status, and diabetes knowledge significantly influenced HbA1c levels in the logistic
regression model. Furthermore, married respondents had higher risks of unsuccessful glycemic control than single respondents. It seems probable that when a couple has a conflict, the DSM
behavior of one of them will worsen57. Therefore, it seemed that single patients were more likely to achieve a target HbA1c of < 7%. Notably, as reported in Table 1, the people with T2DM
had poor diabetes knowledge in rural China. This was because they had a low education level, and some of them were even illiterate. In addition, the patients’ mean age was older than 60
years old, which was related to poor diabetes knowledge, as reported by a qualitative study58. As recent research reported, patients’ low level of diabetes knowledge is an objective
phenomenon in rural China59. Our finding is in line with a study in Thailand60, which found that people with T2DM also had poor diabetes knowledge. Based on the facts of poor diabetes
knowledge, improving diabetes knowledge levels may enable patients to realize the severity of T2DM and promote behavior change. In addition, we found that medication adherence and DSM
factors did not influence HbA1c levels significantly in either the multiple linear regression or logistic regression model. As reported in Table 3, most participants had poor medication
adherence and a low level of DSM due to a lack of diabetes knowledge. It is noted that SMBG was not associated with HbA1c levels (Supplementary Table S4) in this study, which was
inconsistent with the meta-analysis research61. Actually, the relationship between SMBG and HbA1c levels remains unclear. A recent randomized trial found there were no clinically or
statistically significant differences at 1 year in glycemic control between patients who performed SMBG compared with those who did not perform SMBG62. Theoretically, what is important is
the patient’s behavior change based on the results of SMBG that could influence glycemic control, rather than SMBG itself. Therefore, the relationship between these two variables and the
potential mechanism should be explored in the future. There are several limitations to the current study. First, only 64.17% of participants returned for the second measurement of HbA1c.
Although more men declined the second visit (Table 1), no significant difference was found between follow-up men and loss to follow-up men in terms of diabetes knowledge, and neither did
women (Supplementary Table S3). Therefore, the follow-up samples were unbiased and loss to follow-up did not affect the stability of the relationship between diabetes knowledge and HbA1c
levels. Second, the current study relies on a self-report measure of medication adherence and DSM, social desirability bias and recall bias may still exist. More objective measurements of
DSM should be used in the future. Third, only one district was selected in this study, future work will be extended to other sites so that the universality and differences in the
relationship between diabetes knowledge and HbA1c levels can be tested. Concurrently, this study has significant strengths. First, tracking data were used to explore the correlation between
the independent variable and dependent variable, which made causality more plausible. Second, HbA1c was used to assess patients’ average blood glucose concentrations during the preceding 2–3
months, which were more stable than others. Third, people with T2DM in rural areas were chosen as the study population, who were in urgent need of improving DSM behaviors but were rarely
concerned, which has practical significance. CONCLUSIONS This study provided longitudinal evidence for the effects of diabetes knowledge on HbA1c levels in patients with low education
levels, which indicated that interventions focusing on diabetes knowledge need to be strengthened in rural China. The acquisition of knowledge has been played down for several decades in
community chronic disease management. The findings presented important evidence, that knowledge acquisition may have an important role, which may have some implications for the policy of
chronic disease management for low- and middle-income countries. Improving diabetes knowledge need to be strengthened for patients with low education level in rural China, which help improve
outcomes and reduce the disease burden. DATA AVAILABILITY The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
ABBREVIATIONS * T2DM: Type 2 diabetes mellitus * HbA1c: Glycated haemoglobin * BMI: Body mass index * IDF: International Diabetes Federation * FBG: Fasting blood glucose * DKN: Original
version of the diabetes knowledge scales * SDSCA: Original version of the diabetes self-care activities measure * DSM: Diabetes self-management REFERENCES * International Diabetes
Federation. IDF Diabetes Atlas (2019). * International Diabetes Federation. Advocacy guide to the IDF Diabetes Atlas (2019). * Lambrinou, E., Hansen, T. B. & Beulens, J. W. Lifestyle
factors, self-management and patient empowerment in diabetes care. _Eur. J. Prev. Cardiol_ 26, 55–63. https://doi.org/10.1177/2047487319885455 (2019). Article PubMed Google Scholar *
Hamidi, S., Gholamnezhad, Z., Kasraie, N. & Sahebkar, A. The effects of self-efficacy and physical activity improving methods on the quality of life in patients with diabetes: A
systematic review. _J. Diabetes Res._ 2022, 2884933. https://doi.org/10.1155/2022/2884933 (2022). Article PubMed PubMed Central Google Scholar * Sharma, P., Busby, M., Chapple, L.,
Matthews, R. & Chapple, I. The relationship between general health and lifestyle factors and oral health outcomes. _Br. Dent. J._ 221, 65–69. https://doi.org/10.1038/sj.bdj.2016.525
(2016). Article CAS PubMed Google Scholar * Diabetes Prevention Program Research Group. The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: An
intent-to-treat analysis of the DPP/DPPOS. _Diabetes Care_ 35, 723–730. https://doi.org/10.2337/dc11-1468 (2012). Article CAS Google Scholar * Diabetes Prevention Program Research Group.
Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: The Diabetes Prevention Program Outcomes Study.
_Lancet Diabetes Endocrinol._ 3, 866–875. https://doi.org/10.1016/s2213-8587(15)00291-0 (2015). Article PubMed Central Google Scholar * Gong, Q. _et al._ Efficacy of lifestyle
intervention in adults with impaired glucose tolerance with and without impaired fasting plasma glucose: A post hoc analysis of Da Qing Diabetes Prevention Outcome Study. _Diabetes Obes.
Metab._ 23, 2385–2394. https://doi.org/10.1111/dom.14481 (2021). Article CAS PubMed PubMed Central Google Scholar * Gong, Q. _et al._ Morbidity and mortality after lifestyle
intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. _Lancet Diabetes Endocrinol._ 7, 452–461.
https://doi.org/10.1016/s2213-8587(19)30093-2 (2019). Article PubMed PubMed Central Google Scholar * Lehtisalo, J. _et al._ Diabetes, glycaemia, and cognition-a secondary analysis of the
Finnish Diabetes Prevention Study. _Diabetes Metab. Res. Rev._ 32, 102–110. https://doi.org/10.1002/dmrr.2679 (2016). Article CAS PubMed Google Scholar * Lindström, J. _et al._ Improved
lifestyle and decreased diabetes risk over 13 years: Long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS). _Diabetologia_ 56, 284–293.
https://doi.org/10.1007/s00125-012-2752-5 (2013). Article PubMed Google Scholar * International Diabetes Federation. Recommendations for Managing Type 2 Diabetes In Primary Care. (2017).
* International Diabetes Federation. Global Guideline for Managing Older People with Type 2 Diabetes. (2012). * National Health Commission of the People's Republic of China. _Opinions
on promoting the gradual equalization of basic public health services_, https://www.gov.cn/ztzl/ygzt/content_1661065.htm (2009). * National Health Commission of the People's Republic of
China. National Basic Public Health Service Standards (in Chinese). (2017). * Xu, Y. _et al._ Prevalence and control of diabetes in Chinese adults. _JAMA_ 310, 948–959.
https://doi.org/10.1001/jama.2013.168118 (2013). Article CAS PubMed Google Scholar * Wang, L. _et al._ Prevalence and treatment of diabetes in China, 2013–2018. _JAMA_ 326, 2498–2506.
https://doi.org/10.1001/jama.2021.22208 (2021). Article PubMed PubMed Central Google Scholar * Wang, L. _et al._ Prevalence and ethnic pattern of diabetes and prediabetes in China in
2013. _JAMA_ 317, 2515–2523. https://doi.org/10.1001/jama.2017.7596 (2017). Article PubMed PubMed Central Google Scholar * Wenhui, W. H. Z. Z. S. Y. L. W. Z. X Du, J Liao, Q Ye, H Wu
Self-management behaviors and its influencing factors among mid-aged adult patients with type 2 diabetes in A Suburb of Beijing (in Chinese). _Nurs. J. Chin. PLA_ 37 (2020). * Huang, X. _et
al._ Status quo of self-management behaviors and its influencing factors among type 2 diabetes patients in Shandong province (in Chinese). _Chin. J. Public Health_ 35, 1474–1476 (2019).
Google Scholar * Le, C., Rong, S., Dingyun, Y. & Wenlong, C. Socioeconomic disparities in type 2 diabetes mellitus prevalence and self-management behaviors in rural southwest China.
_Diabetes Res. Clin. Pract._ 121, 9–16. https://doi.org/10.1016/j.diabres.2016.07.032 (2016). Article PubMed Google Scholar * Wang, J. & Jia, W. Resources allocation and utilization
efficiency in China’s healthcare sector. _China Finance Econ. Rev._ 10, 88–109. https://doi.org/10.1515/cfer-2021-0012 (2021). Article CAS Google Scholar * Chinese Diabetes Society;
National Office for Primary Diabetes Care. National guidelines for the prevention and control of diabetes in primary care (in Chinese). _Zhonghua Nei Ke Za Zhi_ 57, 885–893.
https://doi.org/10.3760/cma.j.issn.0578-1426.2018.12.003 (2018). Article Google Scholar * World Health Organization. _Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes
Mellitus: Abbreviated Report of a WHO Consultation_ (World Health Organization, 2011). Google Scholar * Lee, S. _et al._ Predictions of diabetes complications and mortality using hba1c
variability: a 10-year observational cohort study. _Acta Diabetol_ 58, 171–180. https://doi.org/10.1007/s00592-020-01605-6 (2021). Article CAS PubMed Google Scholar * Ceriello, A. _et
al._ HbA1c variability predicts cardiovascular complications in type 2 diabetes regardless of being at glycemic target. _Cardiovasc. Diabetol._ 21, 13.
https://doi.org/10.1186/s12933-022-01445-4 (2022). Article CAS PubMed PubMed Central Google Scholar * Klein, K. R. & Buse, J. B. The trials and tribulations of determining HbA1c
targets for diabetes mellitus. _Nat. Rev. Endocrinol._ 16, 717–730. https://doi.org/10.1038/s41574-020-00425-6 (2020). Article CAS PubMed Google Scholar * Kojić Damjanov, S., Đerić, M.
& Eremić Kojić, N. Glycated hemoglobin A1c as a modern biochemical marker of glucose regulation. _Med. Pregl._ 67, 339–344 (2014). Article PubMed Google Scholar * Diabetes Prevention
Program Research Group. HbA1c as a predictor of diabetes and as an outcome in the diabetes prevention program: A randomized clinical trial. _Diabetes Care_ 38, 51–58.
https://doi.org/10.2337/dc14-0886 (2014). Article CAS PubMed Central Google Scholar * Yao, J. _et al._ Factors associated with the utilization of community-based diabetes management
care: A cross-sectional study in Shandong Province, China. _BMC Health Serv. Res._ 20, 407. https://doi.org/10.1186/s12913-020-05292-5 (2020). Article PubMed PubMed Central Google Scholar
* Zhang, R. _et al._ Progress of equalizing basic public health services in Southwest China–-Health education delivery in primary healthcare sectors. _BMC Health Serv. Res._ 20, 247.
https://doi.org/10.1186/s12913-020-05120-w (2020). Article CAS PubMed PubMed Central Google Scholar * He, X. & Wharrad, H. J. Diabetes knowledge and glycemic control among Chinese
people with type 2 diabetes. _Int. Nurs. Rev._ 54, 280–287. https://doi.org/10.1111/j.1466-7657.2007.00570.x (2007). Article CAS PubMed Google Scholar * Yang, H. _et al._ Association
between knowledge-attitude-practices and control of blood glucose, blood pressure, and blood lipids in patients with type 2 diabetes in Shanghai, China: A cross-sectional study. _J. Diabetes
Res._ 2017, 3901392. https://doi.org/10.1155/2017/3901392 (2017). Article PubMed PubMed Central Google Scholar * Guo, X. H. _et al._ A nationwide survey of diabetes education,
self-management and glycemic control in patients with type 2 diabetes in China. _Chin. Med. J._ 125, 4175–4180 (2012). CAS PubMed Google Scholar * Chinese Diabetes Society. Guidelines for
the prevention and control of type 2 diabetes in China (in Chinese). _Chin. J. Pract. Intern. Med._ 38, 292–344 (2018). Google Scholar * The State Council of the People's Republic of
China. _Administrative divisions of the People's Republic of China_, https://www.gov.cn/guoqing/2005-09/13/content_5043917.htm (2005). * National Health Commission of Jiangsu Province.
_Notice on the Announcement of the Results of the Evaluation and Review of the Construction of National Demonstration Areas for comprehensive prevention and control of chronic diseases in
Jiangsu Province_, http://wjw.jiangsu.gov.cn/art/2018/12/29/art_7251_8337518.html (2018). * Cohen, J. _Statistical Power Analysis for the Behavioral Sciences_ 8–13 (Psychology Press, 1988).
MATH Google Scholar * Faul, F., Erdfelder, E., Lang, A. G. & Buchner, A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences.
_Behav. Res. Methods_ 39, 175–191. https://doi.org/10.3758/bf03193146 (2007). Article PubMed Google Scholar * Beeney, L., Dunn, S. & Welch, G. in _Handbook of Psychology and Diabetes_
p. 159–189 (1994). * Yin, X., Savage, C., Toobert, D., Wei, P. & Whitmer, K. Adaptation and testing of instruments to measure diabetes self-management in people with type 2 diabetes in
mainland China. _J. Transcult. Nurs._ 19, 234–242. https://doi.org/10.1177/1043659608319239 (2008). Article Google Scholar * Nathan, D. M., Turgeon, H. & Regan, S. Relationship between
glycated haemoglobin levels and mean glucose levels over time. _Diabetologia_ 50, 2239–2244. https://doi.org/10.1007/s00125-007-0803-0 (2007). Article CAS PubMed PubMed Central Google
Scholar * Goldstein, D. E. _et al._ Tests of glycemia in diabetes. _Diabetes Care_ 27, 1761–1773. https://doi.org/10.2337/diacare.27.7.1761 (2004). Article PubMed Google Scholar * Meng,
J., Kang, X., Li, Z. & Lyu, R. Study on medication adherence in patients with chronic heart failure (in Chinese). _J. Nurs. Admin._ 11, 229–232 (2011). Google Scholar * Toobert, D. J.,
Hampson, S. E. & Glasgow, R. E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. _Diabetes Care_ 23, 943–950.
https://doi.org/10.2337/diacare.23.7.943 (2000). Article CAS PubMed Google Scholar * Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in
China (2020 edition). _Chin. J. Endocrinol. Metab._ 37, 311–398. https://doi.org/10.3760/cma.j.cn311282-20210304-00142 (2021). * Chen, S., Qian, D., Burström, K. & Burström, B. Impact of
an educational intervention in primary care on fasting blood glucose levels and diabetes knowledge among patients with type 2 diabetes mellitus in rural China. _Patient Educ. Counsel._ 103,
1767–1773. https://doi.org/10.1016/j.pec.2020.03.010 (2020). Article Google Scholar * Colleran, K. M., Starr, B. & Burge, M. R. Putting diabetes to the test: Analyzing glycemic
control based on patients’ diabetes knowledge. _Diabetes Care_ 26, 2220–2221. https://doi.org/10.2337/diacare.26.7.2220 (2003). Article PubMed Google Scholar * Choi, T. S. T., Davidson,
Z. E., Walker, K. Z., Lee, J. H. & Palermo, C. Diabetes education for Chinese adults with type 2 diabetes: A systematic review and meta-analysis of the effect on glycemic control.
_Diabetes Res. Clin. Pract._ 116, 218–229. https://doi.org/10.1016/j.diabres.2016.04.001 (2016). Article PubMed Google Scholar * Chen, S., Qian, D. & Burström, B. Two-year impact of
an educational intervention in primary care on blood glucose control and diabetes knowledge among patients with type 2 diabetes mellitus: a study in rural China. _Global Health Action_ 14,
1893502. https://doi.org/10.1080/16549716.2021.1893502 (2021). Article PubMed PubMed Central Google Scholar * Coates, V. E. & Boore, J. R. Knowledge and diabetes self-management.
_Patient Educ. Counsel._ 29, 99–108. https://doi.org/10.1016/0738-3991(96)00938-x (1996). Article CAS Google Scholar * Kautzky-Willer, A., Kosi, L., Lin, J. & Mihaljevic, R.
Gender-based differences in glycaemic control and hypoglycaemia prevalence in patients with type 2 diabetes: results from patient-level pooled data of six randomized controlled trials.
_Diabetes Obes. Metab._ 17, 533–540. https://doi.org/10.1111/dom.12449 (2015). Article CAS PubMed PubMed Central Google Scholar * Yin, J. _et al._ Gender, diabetes education, and
psychosocial factors are associated with persistent poor glycemic control in patients with type 2 diabetes in the Joint Asia Diabetes Evaluation (JADE) program. _J. Diabetes_ 8, 109–119.
https://doi.org/10.1111/1753-0407.12262 (2016). Article CAS PubMed Google Scholar * Hartz, A. _et al._ Factors that influence improvement for patients with poorly controlled type 2
diabetes. _Diabetes Res. Clin. Pract._ 74, 227–232. https://doi.org/10.1016/j.diabres.2006.03.023 (2006). Article PubMed Google Scholar * Juarez, D. T. _et al._ Factors associated with
poor glycemic control or wide glycemic variability among diabetes patients in Hawaii, 2006–2009. _Prevent. Chronic Dis._ 9, 120065. https://doi.org/10.5888/pcd9.120065 (2012). Article
Google Scholar * Zhang, Y. _et al._ Measuring depressive symptoms using the Patient Health Questionnaire-9 in Hong Kong Chinese subjects with type 2 diabetes. _J. Affect. Disord._ 151,
660–666. https://doi.org/10.1016/j.jad.2013.07.014 (2013). Article PubMed ADS Google Scholar * Katz, A. M. Wives of diabetic men. _Bull. Menn. Clin._ 33, 79–94 (1969). Google Scholar *
Ong, W. M., Chua, S. S. & Ng, C. J. Barriers and facilitators to self-monitoring of blood glucose in people with type 2 diabetes using insulin: a qualitative study. _Patient Prefer.
Adher._ 8, 237–246. https://doi.org/10.2147/ppa.S57567 (2014). Article Google Scholar * Wang, Q. _et al._ Prevalence, awareness, treatment and control of diabetes mellitus among
middle-aged and elderly people in a rural Chinese population: A cross-sectional study. _PLoS ONE_ 13, e0198343. https://doi.org/10.1371/journal.pone.0198343 (2018). Article CAS PubMed
PubMed Central Google Scholar * Jaeger, S. R. & Cardello, A. V. Factors affecting data quality of online questionnaires: Issues and metrics for sensory and consumer research. _Food
Qual. Prefer._ 102, 104676. https://doi.org/10.1016/j.foodqual.2022.104676 (2022). Article Google Scholar * Malanda, U. L. _et al._ Self-monitoring of blood glucose in patients with type 2
diabetes mellitus who are not using insulin. _Cochrane Database Syst. Rev._ 1, CD005060. https://doi.org/10.1002/14651858.CD005060.pub3 (2012). Article PubMed Google Scholar * Young, L.
A. _et al._ Glucose self-monitoring in non-insulin-treated patients with type 2 diabetes in primary care settings: A randomized trial. _JAMA Internal Med._ 177, 920–929.
https://doi.org/10.1001/jamainternmed.2017.1233 (2017). Article Google Scholar Download references ACKNOWLEDGEMENTS Thank you for the cooperation of the officials of Health Commission of
Dafeng District in the process of this study, as well as for the cooperation of those who participated in data collection. FUNDING This study was supported by Discipline Construction Funds
from the School of Social Development and Public Policy of Beijing Normal University [Grant No. 312230014] and National Key Research and Development Program of China [Grant No.
2018YFB2101100]. AUTHOR INFORMATION Author notes * These authors contributed equally: Xiaoying Wang and Bo Tian. AUTHORS AND AFFILIATIONS * School of Social Development and Public Policy,
Center for Behavioral Health, Beijing Normal University, Beijing, China Xiaoying Wang, Bo Tian, Jina Li & Weijun Zhang * National Population Heath Data Center, Chinese Academy of Medical
Sciences and Peking Union Medical College, Beijing, China Shengfa Zhang * School of Public Health, Fudan University, Shanghai, China Jinsui Zhang * Yancheng Dafeng People’s Hospital,
Yancheng, Jiangsu Province, China Weiping Yang * School of Sociology and Population Studies, Renmin University of China, Beijing, China Weiwei Wang * North China Electric Power University,
Beijing, China Yuchen Wang Authors * Xiaoying Wang View author publications You can also search for this author inPubMed Google Scholar * Bo Tian View author publications You can also search
for this author inPubMed Google Scholar * Shengfa Zhang View author publications You can also search for this author inPubMed Google Scholar * Jinsui Zhang View author publications You can
also search for this author inPubMed Google Scholar * Weiping Yang View author publications You can also search for this author inPubMed Google Scholar * Jina Li View author publications You
can also search for this author inPubMed Google Scholar * Weiwei Wang View author publications You can also search for this author inPubMed Google Scholar * Yuchen Wang View author
publications You can also search for this author inPubMed Google Scholar * Weijun Zhang View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS
W.Z. was involved in the design of this study and revised the manuscript. X.W., B.T., and S.Z. were involved in the design of this study and data collection. X.W. and W.Z. performed the
statistical analysis and wrote the original draft. J.Z., W.W., J.L., W.Y., and Y.W. contributed to the discussion and reviewed the manuscript. In addition, W.Y. provided full support for
data collection. All authors read and approved the final manuscript. CORRESPONDING AUTHOR Correspondence to Weijun Zhang. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no
competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits
use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the
Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless
indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory
regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Wang, X., Tian, B., Zhang, S. _et al._ Diabetes knowledge predicts HbA1c levels of
people with type 2 diabetes mellitus in rural China: a ten-month follow-up study. _Sci Rep_ 13, 18248 (2023). https://doi.org/10.1038/s41598-023-45312-y Download citation * Received: 18
January 2023 * Accepted: 18 October 2023 * Published: 25 October 2023 * DOI: https://doi.org/10.1038/s41598-023-45312-y SHARE THIS ARTICLE Anyone you share the following link with will be
able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative
