Superior pellucid marginal corneal degeneration
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

Purpose To report the clinical features and topographic findings of superior pellucid marginal corneal degeneration (PMCD).
Methods Retrospective chart review of 15 eyes of eight patients of superior PMCD. Detailed history, visual acuity at presentation, degree of astigmatism, slit-lamp examination findings,
topographic features, and Orbscan findings were noted where available. Improvement in visual acuity with spectacles or contact lens correction, surgical procedure if any, and final visual
acuity were analysed.
Results In all, six patients were males and two were females. All cases except one were bilateral. The patients ranged in age from 18 to 48 years. All cases had isolated superior PMCD. One
patient was a diagnosed case of vernal keratoconjunctivitis. The visual acuity at presentation ranged from hand motions to 20/25. The degree of thinning varied from 30 to 90%. The extent of
thinning was commonly seen between the 10 and 2 o'clock positions. Ectasia was seen below the site of thinning in all the cases of superior PMCD. Topographic features including vertical
corridor of reduced power, against-the-rule astigmatism and superior loop cylinder were seen in 10 eyes. Orbscan was carried out in two eyes of one patient and revealed an area of increased
elevation in relation to the best-fit sphere superiorly corresponding to the area of ectasia in both the eyes. The visual acuity improved with rigid gas-permeable contact lens in six eyes
and the final visual acuity ranged from 20/400 to 20/30. Two eyes were subjected to surgical intervention (peripheral annular graft=1 and lamellar graft=1).
Conclusions PMCD can occur superiorly. It should be considered in the differential diagnosis of superior ectatic disorders. The topographic findings, of reduced power in the vertical
meridian and superior loop cylinder, are typical of superior pellucid marginal degeneration. Visual rehabilitation is usually possible with contact lenses, with surgical management required
in selected cases.
Pellucid marginal corneal degeneration (PMCD) is a bilateral noninflammatory ectatic peripheral corneal disorder usually involving the inferior portion of the cornea.1 It occurs in the
fourth to fifth decades of life and presents as decreased visual acuity due to high irregular against-the-rule astigmatism.2 The cornea typically shows a crescentric area of thinning, from
the 4 to 8 o‘clock position, 1–2 mm from the limbus. The area separating the thinning from the limbus is normal, while the cornea superior to it is ectatic.3 The high against-the-rule
astigmatism and inferior steepening results in the classical topographic features of reduced corneal power in the vertical meridian and increased power in the peripheral cornea inferior to
the lesion site.4 This area of increased power (loop cylinder) usually extends upwards along the cornea in the horizontal oblique hemimeridians. We report eight patients (15 eyes) of
superior pellucid marginal degeneration with topographic features.
We retrospectively reviewed the records of all cases of superior PMCD seen in the cornea service at LV Prasad Eye Institute, a tertiary eye-care centre in Hyderabad, India. A detailed
clinical history including the age of onset of symptoms, family history, any associated systemic diseases or atopy was obtained from all the patients. Slit-lamp biomicroscopic examination in
all the cases detected the extent and degree of thinning as well as the presence of other ectatic conditions. Topographic evaluation was carried out with TMS-1 videokeratoscope (version
1.61). In addition, case no. 2 was evaluated using the orbscan topography system (version 3.0). The case details of patient no. 2 are described below.
A 45-year-old woman presented to us on 6 July 2001 for the management of high astigmatic error in both the eyes. Her medical history was positive for hyperthyroidism. No history of atopy
could be elicited. The best-corrected visual acuity in the right eye was 20/30 with +7Dsph/−16Dcyl × 75 and in the left eye was 20/40 with +6Dsph/−13Dcyl × 110. Biomicroscopic examination
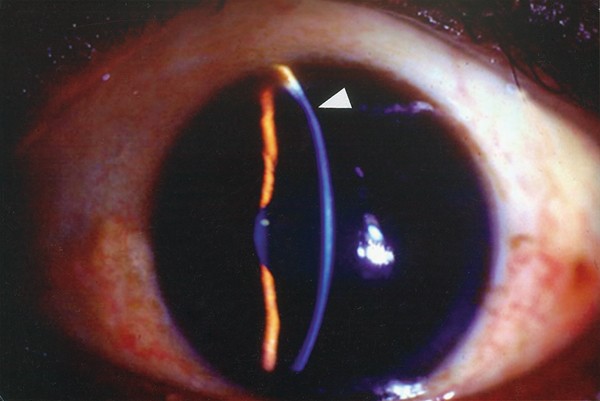
showed clear corneas in both the eyes with no evidence of any inflammation or vascularization. There was a crescent shaped thinning about 2 mm from the limbus extending from 10 to 12 o'
clock positions in both the eyes (Figure 1). The area inferior to thinning was ectatic (Figure 2). The right eye had about 30% thinning and the left eye had 50% thinning. The inferior cornea
was normal in both the eyes. The rest of the anterior segment was unremarkable except for a few anterior cortical lenticular opacities in the right eye. Topographic evaluation revealed
against-the-rule astigmatism with the corridor of lowest power at about 70° in the right eye and 115° in the left eye (Figures 3 and 4).
Slit-lamp view of the right eye of case no. 2 showing thinning superiorly away from the limbus.
Slit-lamp view of the same patient (left eye) showing the ectasia inferior to site of thinning.
Topography of the right eye of the same patient showing the axis of reduced power at 70° with a bow-tie pattern. Note that the superior loop cylinder is not seen in this picture.
Topography of the left eye of the same patient showing changes similar to Figure 3 with the shifting of the meridian of least power to 115°.
Orbscan findings showed an area of increased elevation in relation to the best-fit sphere superiorly corresponding to the area of ectasia in both the eyes (Figures 5 and 6). Further in the
horizontal meridian, the corneal surface showed progressive depression from the centre to the periphery, suggesting steepening. The patient underwent a rigid gas-permeable contact lens trial
and the best-corrected visual acuity was 20/25 in the right eye and 20/30 in the left eye.
Orbscan elevation BFS map of the right eye of the same patient showing the area of increased elevation seen in both the anterior and posterior float. Moreover, note the keratometric map
showing the superior loop cylinder with extension onto horizontal hemimeridians.
Orbscan elevation map of the left eye of the same patient showing a similar area of increased power superiorly. Also seen is an increasing depression in the horizontal meridian towards the
periphery from the centre.
The salient clinical features of the 15 eyes of eight patients are summarized in Table 1. Of these patients, six were males and two were females. All the patients in this series were
bilateral except one. Patient no. 3 had topographic evidence of early PMCD in the right eye. The age of the patients ranged from 18 to 48 years. Patient no. 8 was a diagnosed case of vernal
keratoconjunctivitis and she was not on topical steroids. All the cases had isolated superior PMCD. One case had associated secondary keratoglobus. The visual acuity at presentation ranged
from hand motions to 20/25. The degree of thinning varied from 30 to 90%. In eight eyes, the extent of thinning was from 10 o'clock to 2 o'clock positions. The topographic features in 10 out
of 16 eyes were consistent with the findings of superior PMCD (Table 2). The corneal power was markedly lower in the vertical meridian with a superior loop cylinder peripheral to the area
of thinning. The right eye of patient nos. 1, 4, 6 and the left eye of patient no. 8 had a distorted pattern due to scarring. The scarring is probably because of resolved hydrops in 10
cases. The left eye of patient no. 3 had a keratoglobus-like pattern and the left eye of patient no. 6 had an asymmetric bow-tie pattern. Six eyes were subjected to rigid gas-permeable
contact lens fitting for visual rehabilitation. In two more eyes, RGP contact lens trial was advised. The final visual acuity in those treated with contact lenses ranged from 20/400 to
20/30. Two eyes were subjected to surgery. Patient no. 1 underwent lamellar keratoplasty in the right eye. He had a final visual acuity of 20/50 at 14 months follow-up with a residual
astigmatism of 6D. Patient no. 5 had a peripheral annular graft in the right eye. He had a visual acuity of 20/100 with 7D of astigmatism at his last visit, 2 months following surgery.
Patient no. 7 had almost total cataract in both the eyes, the cause of which was not clear. She underwent cataract surgery. RGP contact lens trial was advised after surgery.
PMCD is a rare clinical entity.1 Although PMCD is a bilateral disorder, atypical unilateral cases have been reported.5,6 The reported age of onset in the literature is the fourth to fifth
decade.1 Cameron and Mahmood3 have reported the association of atopy and vernal keratoconjunctivitis in their series of patients with superior corneal thinning with PMCD. PMCD differs from
other ectatic disorders in its characteristic inferior location and lack of inflammatory signs.7 The site of ectasia is the normal cornea, above the zone of maximum thinning. This differs
from keratoconus where protrusion occurs at the site of maximum thinning.8 Although usually described as involving the inferior four clock hours, superior corneal involvement associated with
inferior PMCD has been reported in the literature.3,7,8,9 Bower et al7 reported a case with superior PMCD with less prominent inferior corneal thinning along with high against-the-rule
astigmatism.8 Tagalia and Sugar9 reported two cases with characteristic features of PMCD with involvement of superior cornea only. Rao et al8 reported corneal topographic changes in five
patients with atypical pellucid marginal degeneration. Isolated superior PMCD was seen in three eyes. The site of thinning can occur in any quadrant. Rao et al8 had a case with nasal PMCD in
their series.
In our series, the age of the patients ranged from 18 to 48 years. Most of the patients were males. Only one patient had associated vernal keratoconjunctivitis. In this series, patient no. 3
had superior PMCD in the left eye with only videokeratographic signs of superior ectasia in the other eye. Topographic features of PMCD with no clinical signs have been reported with
typical, inferior PMCD.2
The classical topographic picture described includes reduced corneal power in the vertical axis and increased power in the peripheral cornea inferior to the site of lesion. This area of
increased power (loop cylinder) usually extends upward along the corneal horizontal oblique hemimeridians.7 A similar picture has also been described in other ectatic disorders such as
Terriens marginal corneal degeneration.10 However, the steepening of inferior periphery with extension to the horizontal oblique meridians is believed to be characteristic of PMCD.2 In the
case of superior PMCD, thinning occurs in a crescent-shaped area superiorly and the area inferior to the site of thinning is ectatic. Consequently, the topographic picture also varies with a
shift of loop cylinder to the superior quadrant. Hence instead of the classical inferior loop, there is a superior loop cylinder peripheral to the area of thinning.2
In this case series, there was superior thinning of the cornea with ectasia. Corneal topography showed typical features of superior PMCD in 10 of the 16 eyes. The flattening in the vertical
meridian is due to the stromal thinning and tissue loss in a semilunar pattern.2 The steepening and protrusion occur at the border of the unaffected tissue, causing the characteristic high
cylindrical loop. The high against-the-rule astigmatism is due to a paradoxical steepening at 90° due to a coupling phenomenon. In all the eyes, the axis of least corridor of power shifted
according to the site and extent of thinning. This axis of least power, as well as the location of loop cylinder depended on the site, extent and spread of circumferential thinning. Orbscan
slit-scan topography evaluation delineated the extent of ectasia in corneal surfaces and correlated with the TMS findings. There have been reports suggesting the possibility of PMCD
preceding keratoglobus.2 One of our cases had associated secondary keratoglobus. This suggests that PMCD may form a part of the spectrum of ectatic disorders where a combination of these
conditions might be seen.
We report this series to highlight that PMCD can occur superiorly. Apart from this series, the literature is sparse on superior PMCD.8,9 We reviewed all cases of PMCD seen during a 1-year
period between 1 July 2001 and 30 June 2002. We studied cases during this 1 year period because we are now aware of superior PMCD and we are actively looking for it. In all, 19 cases of PMCD
presented at our clinic during this period and four (21.05%) of these were isolated superior PMCD. Three out of 19 patients (15.8%) had keratoconus associated with inferior PMCD. We
speculate that we are diagnosing more patients of superior PMCD because difficult cornea cases from all parts of the country are referred to our tertiary-care centre. The other probable
reason is that we are taking more care in evaluating patients with peripheral corneal ectatic disorders.
To conclude, PMCD can occur superiorly. PMCD should be considered in the differential diagnosis of superior corneal ectatic disorders. The topographic picture is characteristic with a
vertical meridian of least power and the superior loop cylinder. Visual rehabilitation is usually possible with contact lens, and surgery may be required in selected cases.
Anyone you share the following link with will be able to read this content:
