Biochemical and cellular properties of insulin receptor signalling
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:

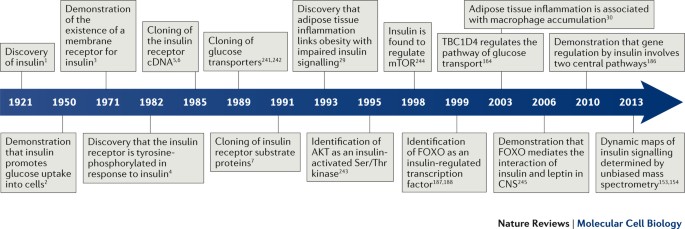
KEY POINTS * Formally started in 1971 with the discovery of the insulin receptor, the field of insulin signalling has by now resolved many questions related to the cellular, biochemical
foundation of the hormone's biological effects. * The three major biochemical steps in insulin signalling are: tyrosine phosphorylation of the receptor and its direct substrates;
activation of the lipid kinase, PI3K; and activation of multiple serine/threonine kinases, the most important of which is AKT. * Through various combinations of these signalling modules in
different cell types, with different time and dose dependence after insulin binding, innumerable combinations of signalling complexes can be obtained. This diversity likely underpins the
pleiotropism of insulin action, as well as the pathogenesis of insulin resistance. * Key recent discoveries in the field include the delineation of a pathway to insulin-dependent glucose
transport, the emergence of two central pathways for regulation of gene expression, the interaction of insulin and leptin signalling in the CNS to facilitate energy homeostasis, and the role
of inflammation as a regulator of insulin signalling. ABSTRACT The mechanism of insulin action is a central theme in biology and medicine. In addition to the rather rare condition of
insulin deficiency caused by autoimmune destruction of pancreatic β-cells, genetic and acquired abnormalities of insulin action underlie the far more common conditions of type 2 diabetes,
obesity and insulin resistance. The latter predisposes to diseases ranging from hypertension to Alzheimer disease and cancer. Hence, understanding the biochemical and cellular properties of
insulin receptor signalling is arguably a priority in biomedical research. In the past decade, major progress has led to the delineation of mechanisms of glucose transport, lipid synthesis,
storage and mobilization. In addition to direct effects of insulin on signalling kinases and metabolic enzymes, the discovery of mechanisms of insulin-regulated gene transcription has led to
a reassessment of the general principles of insulin action. These advances will accelerate the discovery of new treatment modalities for diabetes. Access through your institution Buy or
subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Access Nature and 54 other Nature Portfolio journals Get
Nature+, our best-value online-access subscription $29.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12 print issues and online access $209.00 per year only
$17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which are calculated during checkout
ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS REGULATION AND FUNCTION OF
INSULIN AND INSULIN-LIKE GROWTH FACTOR RECEPTOR SIGNALLING Article 10 February 2025 INSULIN RESISTANCE IN TYPE 2 DIABETES MELLITUS Article 17 April 2025 ACTIVATION OF THE HUMAN INSULIN
RECEPTOR BY NON-INSULIN-RELATED PEPTIDES Article Open access 28 September 2022 REFERENCES * Banting, F. G., Best, C. H., Collip, J. B., Campbell, W. R. & Fletcher, A. A. Pancreatic
extracts in the treatment of diabetes mellitus. _Can. Med. Assoc. J._ 12, 141–146 (1922). CAS PubMed PubMed Central Google Scholar * Levine, R., Goldstein, M. S., Huddlestun, B. &
Klein, S. P. Action of insulin on the 'permeability' of cells to free hexoses, as studied by its effect on the distribution of galactose. _Am. J. Physiol._ 163, 70–76 (1950).
Article CAS PubMed Google Scholar * Freychet, P., Roth, J. & Neville, D. M. Jr. Insulin receptors in the liver: specific binding of (125 I)insulin to the plasma membrane and its
relation to insulin bioactivity. _Proc. Natl Acad. Sci. USA_ 68, 1833–1837 (1971). Article CAS PubMed Google Scholar * Kasuga, M., Zick, Y., Blithe, D. L., Crettaz, M. & Kahn, C. R.
Insulin stimulates tyrosine phosphorylation of the insulin receptor in a cell-free system. _Nature_ 298, 667–669 (1982). Article CAS PubMed Google Scholar * Ebina, Y. et al. The human
insulin receptor cDNA: the structural basis for hormone-activated transmembrane signalling. _Cell_ 40, 747–758 (1985). Article CAS PubMed Google Scholar * Ullrich, A. et al. Human
insulin receptor and its relationship to the tyrosine kinase family of oncogenes. _Nature_ 313, 756–761 (1985). Article CAS PubMed Google Scholar * Sun, X. J. et al. Structure of the
insulin receptor substrate IRS-1 defines a unique signal transduction protein. _Nature_ 352, 73–77 (1991). Article CAS PubMed Google Scholar * Kohn, A. D., Kovacina, K. S. & Roth, R.
A. Insulin stimulates the kinase activity of RAC-PK, a pleckstrin homology domain containing ser/thr kinase. _EMBO J._ 14, 4288–4295 (1995). Article CAS PubMed PubMed Central Google
Scholar * Gehart, H., Kumpf, S., Ittner, A. & Ricci, R. MAPK signalling in cellular metabolism: stress or wellness? _EMBO Rep._ 11, 834–840 (2010). Article CAS PubMed PubMed Central
Google Scholar * Taniguchi, C. M., Emanuelli, B. & Kahn, C. R. Critical nodes in signalling pathways: insights into insulin action. _Nat. Rev. Mol. Cell Biol._ 7, 85–96 (2006).
Article CAS PubMed Google Scholar * Kim, Y.-B., Nikoulina, S. E., Ciaraldi, T. P., Henry, R. R. & Kahn, B. B. Normal insulin-dependent activation of Akt/protein kinase B, with
diminished activation of phosphoinositide 3-kinase, in muscle in type 2 diabetes. _J. Clin. Invest._ 104, 733–741 (1999). Article CAS PubMed PubMed Central Google Scholar * Nadler, S.
T. et al. Normal Akt/PKB with reduced PI3K activation in insulin-resistant mice. _Am. J. Physiol. Endocrinol. Metab._ 281, E1249–E1254 (2001). Article CAS PubMed Google Scholar *
Cleasby, M. E., Reinten, T. A., Cooney, G. J., James, D. E. & Kraegen, E. W. Functional studies of Akt isoform specificity in skeletal muscle _in vivo_; maintained insulin sensitivity
despite reduced insulin receptor substrate-1 expression. _Mol. Endocrinol._ 21, 215–228 (2007). Article CAS PubMed Google Scholar * Hoehn, K. L. et al. IRS1-independent defects define
major nodes of insulin resistance. _Cell Metab._ 7, 421–433 (2008). Article CAS PubMed PubMed Central Google Scholar * Kang, S. et al. Identification of nuclear hormone receptor
pathways causing insulin resistance by transcriptional and epigenomic analysis. _Nat. Cell Biol._ 17, 44–56 (2015). Article CAS PubMed Google Scholar * Odegaard, J. I. & Chawla, A.
Pleiotropic actions of insulin resistance and inflammation in metabolic homeostasis. _Science_ 339, 172–177 (2013). Article CAS PubMed PubMed Central Google Scholar * Ortega-Molina, A.
et al. Pharmacological inhibition of PI3K reduces adiposity and metabolic syndrome in obese mice and rhesus monkeys. _Cell Metab._ 21, 558–570 (2015). Article CAS PubMed PubMed Central
Google Scholar * Boucher, J., Kleinridders, A. & Kahn, C. R. Insulin receptor signaling in normal and insulin-resistant states. _Cold Spring Harb. Perspect. Biol._ 6, a009191 (2014).
Article CAS PubMed PubMed Central Google Scholar * Könner, A. C. & Brüning, Jens, C. Selective insulin and leptin resistance in metabolic disorders. _Cell Metab._ 16, 144–152 *
Czech, M. P. Insulin action and resistance in obesity and type 2 diabetes. _Nat. Med._ 23, 804–814 (2017). THIS PERSPECTIVE HIGHLIGHTS RECENT CONTROVERSIES AND CHALLENGES IN UNDERSTANDING
THE EFFECTS OF OBESITY ON INSULIN SIGNALLING. Article CAS PubMed PubMed Central Google Scholar * Gavin, J. R. et al. Insulin-dependent regulation of insulin receptor concentrations: a
direct demonstration in cell culture. _Proc. Natl Acad. Sci. USA_ 71, 84–88 (1974). Article CAS PubMed Google Scholar * Backer, J. M., Kahn, C. R., Cahill, D. A., Ullrich, A. &
White, M. F. Receptor-mediated internalization of insulin requires a 12-amino acid sequence in the juxtamembrane region of the insulin receptor β-subunit. _J. Biol. Chem._ 265, 16450–16454
(1990). CAS PubMed Google Scholar * Kolterman, O. G., Saekow, M. & Olefsky, J. M. The effects of acute and chronic starvation on insulin binding to isolated human adipocytes. _J.
Clin. Endocrinol. Metabolism_ 48, 836–842 (1979). Article CAS Google Scholar * Copps, K. D. & White, M. F. Regulation of insulin sensitivity by serine/threonine phosphorylation of
insulin receptor substrate proteins IRS1 and IRS2. _Diabetologia_ 55, 2565–2582 (2012). Article CAS PubMed PubMed Central Google Scholar * Shah, O. J., Wang, Z. & Hunter, T.
Inappropriate activation of the TSC/Rheb/mTOR/S6K cassette induces IRS1/2 depletion, insulin resistance, and cell survival deficiencies. _Curr. Biol._ 14, 1650–1656 (2004). Article CAS
PubMed Google Scholar * Harrington, L. S. et al. The TSC1-2 tumor suppressor controls insulin-PI3K signaling via regulation of IRS proteins. _J. Cell Biol._ 166, 213–223 (2004). Article
CAS PubMed PubMed Central Google Scholar * Um, S. H. et al. Absence of S6K1 protects against age- and diet-induced obesity while enhancing insulin sensitivity. _Nature_ 431, 200–205
(2004). Article CAS PubMed Google Scholar * Copps, K. D., Hançer, N. J., Qiu, W. & White, M. F. Serine 302 phosphorylation of mouse insulin receptor substrate 1 (IRS1) is dispensable
for normal insulin signaling and feedback regulation by hepatic S6 kinase. _J. Biol. Chem._ 291, 8602–8617 (2016). Article CAS PubMed PubMed Central Google Scholar * Hotamisligil, G.
S., Shargill, N. S. & Spiegelman, B. M. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. _Science_ 259, 87–91 (1993). Article CAS
PubMed Google Scholar * Weisberg, S. P. et al. Obesity is associated with macrophage accumulation in adipose tissue. _J. Clin. Invest._ 112, 1796–1808 (2003). Article CAS PubMed PubMed
Central Google Scholar * Xu, H. et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. _J. Clin. Invest._ 112, 1821–1830 (2003).
Article CAS PubMed PubMed Central Google Scholar * Osborn, O. & Olefsky, J. M. The cellular and signaling networks linking the immune system and metabolism in disease. _Nat. Med._
18, 363–374 (2012). Article CAS PubMed Google Scholar * Olefsky, J. M. & Glass, C. K. Macrophages, inflammation, and insulin resistance. _Annu. Rev. Physiol._ 72, 219–246 (2010).
Article CAS PubMed Google Scholar * Copps, K. D. et al. Irs1 Serine 307 promotes insulin sensitivity in mice. _Cell. Metab._ 11, 84–92 (2010). Article CAS PubMed PubMed Central
Google Scholar * Petersen, M. C. et al. Insulin receptor Thr1160 phosphorylation mediates lipid-induced hepatic insulin resistance. _J. Clin. Invest._ 126, 4361–4371 (2016). Article PubMed
PubMed Central Google Scholar * Samuel, Varman, T. & Shulman, Gerald, I. Mechanisms for insulin resistance: common threads and missing links. _Cell_ 148, 852–871 (2012). Article CAS
Google Scholar * Samuel, V. T. et al. Inhibition of protein kinase Cɛ prevents hepatic insulin resistance in nonalcoholic fatty liver disease. _J. Clin. Invest._ 117, 739–745 (2007).
Article CAS PubMed PubMed Central Google Scholar * Chaurasia, B. & Summers, S. A. Ceramides — lipotoxic inducers of metabolic disorders. _Trends Endocrinol. Metab._ 26, 538–550
(2015). Article CAS PubMed Google Scholar * Xia, J. Y., Morley, T. S. & Scherer, P. E. The adipokine/ceramide axis: key aspects of insulin sensitization. _Biochimie_ 96, 130–139
(2014). Article CAS PubMed Google Scholar * Lazar, D. F. & Saltiel, A. R. Lipid phosphatases as drug discovery targets for type 2 diabetes. _Nat. Rev. Drug Discov._ 5, 333–342
(2006). Article CAS PubMed Google Scholar * Ogg, S. & Ruvkun, G. The _C. elegans_ PTEN homolog, DAF-18, acts in the insulin receptor-like metabolic signaling pathway. _Mol. Cell_ 2,
887–893 (1998). Article CAS PubMed Google Scholar * Song, M. S., Salmena, L. & Pandolfi, P. P. The functions and regulation of the PTEN tumour suppressor. _Nat. Rev. Mol. Cell Biol._
13, 283–296 (2012). Article CAS PubMed Google Scholar * Leslie, N. R. & Downes, C. P. PTEN function: how normal cells control it and tumour cells lose it. _Biochem. J._ 382, 1–11
(2004). Article CAS PubMed PubMed Central Google Scholar * Butler, M. et al. Specific inhibition of PTEN expression reverses hyperglycemia in diabetic mice. _Diabetes_ 51, 1028–1034
(2002). Article CAS PubMed Google Scholar * Horie, Y. et al. Hepatocyte-specific Pten deficiency results in steatohepatitis and hepatocellular carcinomas. _J. Clin. Invest._ 113,
1774–1783 (2004). Article CAS PubMed PubMed Central Google Scholar * Stiles, B. et al. Liver-specific deletion of negative regulator Pten results in fatty liver and insulin
hypersensitivity [corrected]. _Proc. Natl Acad. Sci. USA_ 101, 2082–2087 (2004). Article CAS PubMed Google Scholar * Kurlawalla-Martinez, C. et al. Insulin hypersensitivity and
resistance to streptozotocin-induced diabetes in mice lacking PTEN in adipose tissue. _Mol. Cell. Biol._ 25, 2498–2510 (2005). Article CAS PubMed PubMed Central Google Scholar * Morley,
T. S., Xia, J. Y. & Scherer, P. E. Selective enhancement of insulin sensitivity in the mature adipocyte is sufficient for systemic metabolic improvements. _Nat. Commun._ 6, 7906 (2015).
Article CAS PubMed PubMed Central Google Scholar * Wijesekara, N. et al. Muscle-specific Pten deletion protects against insulin resistance and diabetes. _Mol. Cell. Biol._ 25,
1135–1145 (2005). Article CAS PubMed PubMed Central Google Scholar * Wong, J. T. et al. Pten (phosphatase and tensin homologue gene) haploinsufficiency promotes insulin
hypersensitivity. _Diabetologia_ 50, 395–403 (2007). Article CAS PubMed Google Scholar * Pal, A. et al. PTEN mutations as a cause of constitutive insulin sensitivity and obesity. _N.
Engl. J. Med._ 367, 1002–1011 (2012). Article CAS PubMed PubMed Central Google Scholar * Ishihara, H. et al. Molecular cloning of rat SH2-containing inositol phosphatase 2 (SHIP2) and
its role in the regulation of insulin signaling. _Biochem. Biophys. Res. Commun._ 260, 265–272 (1999). Article CAS PubMed Google Scholar * Sleeman, M. W. et al. Absence of the lipid
phosphatase SHIP2 confers resistance to dietary obesity. _Nat. Med._ 11, 199–205 (2005). Article CAS PubMed Google Scholar * Clement, S. et al. The lipid phosphatase SHIP2 controls
insulin sensitivity. _Nature_ 409, 92–97 (2001). Article CAS PubMed Google Scholar * Clement, S. et al. Corrigendum: the lipid phosphatase SHIP2 controls insulin sensitivity. _Nature_
431, 878–878 (2004). Article CAS Google Scholar * Fukui, K. et al. Impact of the liver-specific expression of SHIP2 (SH2-containing inositol 5′-phosphatase 2) on insulin signaling and
glucose metabolism in mice. _Diabetes_ 54, 1958–1967 (2005). Article CAS PubMed Google Scholar * Grempler, R. et al. Normalization of prandial blood glucose and improvement of glucose
tolerance by liver-specific inhibition of SH2 domain containing inositol phosphatase 2 (SHIP2) in diabetic KKAy mice: SHIP2 inhibition causes insulin-mimetic effects on glycogen metabolism,
gluconeogenesis, and glycolysis. _Diabetes_ 56, 2235–2241 (2007). Article CAS PubMed Google Scholar * Buettner, R. et al. Antisense oligonucleotides against the lipid phosphatase SHIP2
improve muscle insulin sensitivity in a dietary rat model of the metabolic syndrome. _Am. J. Physiol. Endocrinol. Metab._ 292, E1871–E1878 (2007). Article CAS PubMed Google Scholar *
Suwa, A. et al. Discovery and functional characterization of a novel small molecule inhibitor of the intracellular phosphatase, SHIP2. _Br. J. Pharmacol._ 158, 879–887 (2009). Article CAS
PubMed PubMed Central Google Scholar * Johnson, T. O., Ermolieff, J. & Jirousek, M. R. Protein tyrosine phosphatase 1B inhibitors for diabetes. _Nat. Rev. Drug Discov._ 1, 696–709
(2002). Article CAS PubMed Google Scholar * Ukkola, O. & Santaniemi, M. Protein tyrosine phosphatase 1B: a new target for the treatment of obesity and associated co-morbidities. _J.
Internal Med._ 251, 467–475 (2002). Article CAS PubMed Google Scholar * Feldhammer, M., Uetani, N., Miranda-Saavedra, D. & Tremblay, M. L. PTP1B: a simple enzyme for a complex world.
_Crit. Rev. Biochem. Mol. Biol._ 48, 430–445 (2013). Article CAS PubMed Google Scholar * Elchebly, M. et al. Increased insulin sensitivity and obesity resistance in mice lacking the
protein tyrosine phosphatase-1B gene. _Science_ 283, 1544–1548 (1999). Article CAS PubMed Google Scholar * Klaman, L. D. et al. Increased energy expenditure, decreased adiposity, and
tissue-specific insulin sensitivity in protein-tyrosine phosphatase 1B-deficient mice. _Mol. Cell. Biol._ 20, 5479–5489 (2000). Article CAS PubMed PubMed Central Google Scholar * Bence,
K. K. et al. Neuronal PTP1B regulates body weight, adiposity and leptin action. _Nat. Med._ 12, 917–924 (2006). Article CAS PubMed Google Scholar * Banno, R. et al. PTP1B and SHP2 in
POMC neurons reciprocally regulate energy balance in mice. _J. Clin. Invest._ 120, 720–734 (2010). Article CAS PubMed PubMed Central Google Scholar * Delibegovic, M. et al.
Liver-specific deletion of protein-tyrosine phosphatase 1B (PTP1B) improves metabolic syndrome and attenuates diet-induced endoplasmic reticulum stress. _Diabetes_ 58, 590–599 (2009).
Article CAS PubMed PubMed Central Google Scholar * Delibegovic, M. et al. Improved glucose homeostasis in mice with muscle-specific deletion of protein-tyrosine phosphatase 1B. _Mol.
Cell. Biol._ 27, 7727–7734 (2007). Article CAS PubMed PubMed Central Google Scholar * Zinker, B. A. et al. PTP1B antisense oligonucleotide lowers PTP1B protein, normalizes blood
glucose, and improves insulin sensitivity in diabetic mice. _Proc. Natl Acad. Sci. USA_ 99, 11357–11362 (2002). Article CAS PubMed Google Scholar * Brognard, J. & Newton, A. C.
PHLiPPing the switch on Akt and protein kinase C signaling. _Trends Endocrinol. Metab._ 19, 223–230 (2008). Article CAS PubMed PubMed Central Google Scholar * Newton, A. C. &
Trotman, L. C. Turning off AKT: PHLPP as a drug target. _Annu. Rev. Pharmacol. Toxicol._ 54, 537–558 (2014). Article CAS PubMed PubMed Central Google Scholar * Gao, T., Furnari, F.
& Newton, A. C. PHLPP: a phosphatase that directly dephosphorylates Akt, promotes apoptosis, and suppresses tumor growth. _Mol. Cell_ 18, 13–24 (2005). Article CAS PubMed Google
Scholar * Brognard, J., Sierecki, E., Gao, T. & Newton, A. C. PHLPP and a second isoform, PHLPP2, differentially attenuate the amplitude of Akt signaling by regulating distinct Akt
isoforms. _Mol. Cell_ 25, 917–931 (2007). Article CAS PubMed Google Scholar * Gao, T., Brognard, J. & Newton, A. C. The phosphatase PHLPP controls the cellular levels of protein
kinase C. _J. Biol. Chem._ 283, 6300–6311 (2008). Article CAS PubMed Google Scholar * Liu, J., Stevens, P. D., Li, X., Schmidt, M. D. & Gao, T. PHLPP-mediated dephosphorylation of
S6K1 inhibits protein translation and cell growth. _Mol. Cell. Biol._ 31, 4917–4927 (2011). Article CAS PubMed PubMed Central Google Scholar * Liu, J., Stevens, P. D. & Gao, T.
mTOR-dependent regulation of PHLPP expression controls the rapamycin sensitivity in cancer cells. _J. Biol. Chem._ 286, 6510–6520 (2011). Article CAS PubMed Google Scholar * Li, X., Liu,
J. & Gao, T. β-TrCP-mediated ubiquitination and degradation of PHLPP1 are negatively regulated by Akt. _Mol. Cell. Biol._ 29, 6192–6205 (2009). Article CAS PubMed PubMed Central
Google Scholar * Ugi, S. et al. Protein phosphatase 2A negatively regulates insulin's metabolic signaling pathway by inhibiting Akt (protein kinase B) activity in 3T3-L1 adipocytes.
_Mol. Cell. Biol._ 24, 8778–8789 (2004). Article CAS PubMed PubMed Central Google Scholar * Gotz, J. & Schild, A. Transgenic and knockout models of PP2A. _Methods Enzymol._ 366,
390–403 (2003). Article PubMed Google Scholar * Rodgers, J. T., Vogel, R. O. & Puigserver, P. Clk2 and B56β mediate insulin-regulated assembly of the PP2A phosphatase holoenzyme
complex on Akt. _Mol. Cell_ 41, 471–479 (2011). Article CAS PubMed PubMed Central Google Scholar * Xian, L. et al. Liver-specific deletion of Ppp2cα enhances glucose metabolism and
insulin sensitivity. _Aging_ 7, 223–232 (2015). Article CAS PubMed PubMed Central Google Scholar * Galbo, T. et al. PP2A inhibition results in hepatic insulin resistance despite Akt2
activation. _Aging_ 5, 770–781 (2013). Article CAS PubMed PubMed Central Google Scholar * Desbuquois, B., Carre, N. & Burnol, A. F. Regulation of insulin and type 1 insulin-like
growth factor signaling and action by the Grb10/14 and SH2B1/B2 adaptor proteins. _FEBS J._ 280, 794–816 (2013). CAS PubMed Google Scholar * Depetris, R. S. et al. Structural basis for
inhibition of the insulin receptor by the adaptor protein Grb14. _Mol. Cell_ 20, 325–333 (2005). Article CAS PubMed PubMed Central Google Scholar * Stein, E. G., Ghirlando, R. &
Hubbard, S. R. Structural basis for dimerization of the Grb10 Src homology 2 domain. Implications for ligand specificity. _J. Biol. Chem._ 278, 13257–13264 (2003). Article CAS PubMed
Google Scholar * Bereziat, V. et al. Inhibition of insulin receptor catalytic activity by the molecular adapter Grb14. _J. Biol. Chem._ 277, 4845–4852 (2002). Article CAS PubMed Google
Scholar * Cooney, G. J. et al. Improved glucose homeostasis and enhanced insulin signalling in Grb14-deficient mice. _EMBO J._ 23, 582–593 (2004). Article CAS PubMed PubMed Central
Google Scholar * Smith, F. M. et al. Mice with a disruption of the imprinted Grb10 gene exhibit altered body composition, glucose homeostasis, and insulin signaling during postnatal life.
_Mol. Cell. Biol._ 27, 5871–5886 (2007). Article CAS PubMed PubMed Central Google Scholar * Yu, Y. et al. Phosphoproteomic analysis identifies Grb10 as an mTORC1 substrate that
negatively regulates insulin signaling. _Science_ 332, 1322–1326 (2011). Article CAS PubMed PubMed Central Google Scholar * Hsu, P. P. et al. The mTOR-regulated phosphoproteome reveals
a mechanism of mTORC1-mediated inhibition of growth factor signaling. _Science_ 332, 1317–1322 (2011). Article CAS PubMed PubMed Central Google Scholar * Wang, L. et al. Peripheral
disruption of the Grb10 gene enhances insulin signaling and sensitivity _in vivo_. _Mol. Cell. Biol._ 27, 6497–6505 (2007). Article CAS PubMed PubMed Central Google Scholar * Holt, L.
J. et al. Dual ablation of Grb10 and Grb14 in mice reveals their combined role in regulation of insulin signaling and glucose homeostasis. _Mol. Endocrinol._ 23, 1406–1414 (2009). Article
CAS PubMed PubMed Central Google Scholar * Manning, A. K. et al. A genome-wide approach accounting for body mass index identifies genetic variants influencing fasting glycemic traits and
insulin resistance. _Nat. Genet._ 44, 659–669 (2012). Article CAS PubMed PubMed Central Google Scholar * Sohani, Z. N. et al. Risk alleles in/near ADCY5, ADRA2A, CDKAL1, CDKN2A/B,
GRB10, and TCF7L2 elevate plasma glucose levels at birth and in early childhood: results from the FAMILY study. _PLoS ONE_ 11, e0152107 (2016). Article CAS PubMed PubMed Central Google
Scholar * Rampersaud, E. et al. Identification of novel candidate genes for type 2 diabetes from a genome-wide association scan in the Old Order Amish: evidence for replication from
diabetes-related quantitative traits and from independent populations. _Diabetes_ 56, 3053–3062 (2007). Article CAS PubMed Google Scholar * Prokopenko, I. et al. A central role for GRB10
in regulation of islet function in man. _PLoS Genet._ 10, e1004235 (2014). Article CAS PubMed PubMed Central Google Scholar * Scott, R. A. et al. Large-scale association analyses
identify new loci influencing glycemic traits and provide insight into the underlying biological pathways. _Nat. Genet._ 44, 991–1005 (2012). Article CAS PubMed PubMed Central Google
Scholar * Kooner, J. S. et al. Genome-wide association study in individuals of South Asian ancestry identifies six new type 2 diabetes susceptibility loci. _Nat. Genet._ 43, 984–989 (2011).
Article CAS PubMed PubMed Central Google Scholar * Harder, M. N. et al. Type 2 diabetes risk alleles near BCAR1 and in ANK1 associate with decreased β-cell function whereas risk
alleles near ANKRD55 and GRB14 associate with decreased insulin sensitivity in the Danish Inter99 cohort. _J. Clin. Endocrinol. Metabolism_ 98, E801–E806 (2013). Article CAS Google Scholar
* Lu, Y. et al. New loci for body fat percentage reveal link between adiposity and cardiometabolic disease risk. _Nat. Commun._ 7, 10495 (2016). Article CAS PubMed PubMed Central
Google Scholar * Heid, I. M. et al. Meta-analysis identifies 13 new loci associated with waist-hip ratio and reveals sexual dimorphism in the genetic basis of fat distribution. _Nat.
Genet._ 42, 949–960 (2010). Article CAS PubMed PubMed Central Google Scholar * Liu, C. T. et al. Genome-wide association of body fat distribution in African ancestry populations
suggests new loci. _PLoS Genet._ 9, e1003681 (2013). Article CAS PubMed PubMed Central Google Scholar * Randall, J. C. et al. Sex-stratified genome-wide association studies including
270,000 individuals show sexual dimorphism in genetic loci for anthropometric traits. _PLoS Genet._ 9, e1003500 (2013). Article CAS PubMed PubMed Central Google Scholar * Shungin, D. et
al. New genetic loci link adipose and insulin biology to body fat distribution. _Nature_ 518, 187–196 (2015). Article CAS PubMed PubMed Central Google Scholar * Morris, A. P. et al.
Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. _Nat. Genet._ 44, 981–990 (2012). Article CAS PubMed PubMed
Central Google Scholar * Howard, J. K. & Flier, J. S. Attenuation of leptin and insulin signaling by SOCS proteins. _Trends Endocrinol. Metab._ 17, 365–371 (2006). Article CAS PubMed
Google Scholar * Jorgensen, S. B. et al. Deletion of skeletal muscle SOCS3 prevents insulin resistance in obesity. _Diabetes_ 62, 56–64 (2013). Article CAS PubMed Google Scholar *
Emanuelli, B., Macotela, Y., Boucher, J. & Ronald Kahn, C. SOCS-1 deficiency does not prevent diet-induced insulin resistance. _Biochem. Biophys. Res. Commun._ 377, 447–452 (2008).
Article CAS PubMed PubMed Central Google Scholar * Marine, J.-C. et al. SOCS1 deficiency causes a lymphocyte-dependent perinatal lethality. _Cell_ 98, 609–616 (1999). Article CAS
PubMed Google Scholar * Rui, L. SH2B1 regulation of energy balance, body weight, and glucose metabolism. _World J. Diabetes_ 5, 511–526 (2014). Article PubMed PubMed Central Google
Scholar * Song, W. et al. SH2B regulation of growth, metabolism, and longevity in both insects and mammals. _Cell Metab._ 11, 427–437 (2010). Article CAS PubMed PubMed Central Google
Scholar * Morris, D. L., Cho, K. W., Zhou, Y. & Rui, L. SH2B1 enhances insulin sensitivity by both stimulating the insulin receptor and inhibiting tyrosine dephosphorylation of insulin
receptor substrate proteins. _Diabetes_ 58, 2039–2047 (2009). Article CAS PubMed PubMed Central Google Scholar * Bauer, F. et al. Obesity genes identified in genome-wide association
studies are associated with adiposity measures and potentially with nutrient-specific food preference. _Am. J. Clin. Nutr._ 90, 951–959 (2009). Article CAS PubMed Google Scholar *
Jamshidi, Y., Snieder, H., Ge, D., Spector, T. D. & O'Dell, S. D. The SH2B gene is associated with serum leptin and body fat in normal female twins. _Obesity (Silver Spring)_ 15,
5–9 (2007). Article CAS Google Scholar * Renstrom, F. et al. Replication and extension of genome-wide association study results for obesity in 4923 adults from northern Sweden. _Hum. Mol.
Genet._ 18, 1489–1496 (2009). Article CAS PubMed PubMed Central Google Scholar * Thorleifsson, G. et al. Genome-wide association yields new sequence variants at seven loci that
associate with measures of obesity. _Nat. Genet._ 41, 18–24 (2009). Article CAS PubMed Google Scholar * Willer, C. J. et al. Six new loci associated with body mass index highlight a
neuronal influence on body weight regulation. _Nat. Genet._ 41, 25–34 (2009). Article CAS PubMed Google Scholar * Hotta, K. et al. Association between type 2 diabetes genetic
susceptibility loci and visceral and subcutaneous fat area as determined by computed tomography. _J. Hum. Genet._ 57, 305–310 (2012). Article CAS PubMed Google Scholar * Bochukova, E. G.
et al. Large, rare chromosomal deletions associated with severe early-onset obesity. _Nature_ 463, 666–670 (2010). Article CAS PubMed Google Scholar * Walters, R. G. et al. A new highly
penetrant form of obesity due to deletions on chromosome 16p11.2. _Nature_ 463, 671–675 (2010). Article CAS PubMed PubMed Central Google Scholar * Prudente, S. et al. The SH2B1 obesity
locus and abnormal glucose homeostasis: lack of evidence for association from a meta-analysis in individuals of European ancestry. _Nutr. Metab. Cardiovasc. Dis._ 23, 1043–1049 (2013).
Article CAS PubMed Google Scholar * Belfiore, A. & Malaguarnera, R. The insulin receptor: a new target for cancer therapy. _Front. Endocrinol._
http://dx.doi.org/10.3389/fendo.2011.00093 (2011). * Diaz-Castroverde, S. et al. Insulin receptor isoform A ameliorates long-term glucose intolerance in diabetic mice. _Dis. Model. Mech._ 9,
1271–1281 (2016). Article CAS PubMed PubMed Central Google Scholar * Diaz-Castroverde, S. et al. Prevalent role of the insulin receptor isoform A in the regulation of hepatic glycogen
metabolism in hepatocytes and in mice. _Diabetologia_ 59, 2702–2710 (2016). Article CAS PubMed Google Scholar * Moller, D. E., Yokota, A., Caro, J. F. & Flier, J. S. Tissue-specific
expression of two alternatively spliced insulin receptor mRNAs in man. _Mol. Endocrinol._ 3, 1263–1269 (1989). Article CAS PubMed Google Scholar * Bjornholm, M. et al. Absence of
functional insulin receptor substrate-3 (IRS-3) gene in humans. _Diabetologia_ 45, 1697–1702 (2002). Article CAS PubMed Google Scholar * Dong, X. C. et al. Inactivation of hepatic Foxo1
by insulin signaling is required for adaptive nutrient homeostasis and endocrine growth regulation. _Cell Metab._ 8, 65–76 (2008). Article CAS PubMed PubMed Central Google Scholar *
Kubota, N. et al. Dynamic functional relay between insulin receptor substrate 1 and 2 in hepatic insulin signaling during fasting and feeding. _Cell Metab._ 8, 49–64 (2008). Article CAS
PubMed Google Scholar * Michael, M. D. et al. Loss of insulin signaling in hepatocytes leads to severe insulin resistance and progressive hepatic dysfunction. _Mol. Cell_ 6, 87–97 (2000).
Article CAS PubMed Google Scholar * Long, Y. C., Cheng, Z., Copps, K. D. & White, M. F. Insulin receptor substrates Irs1 and Irs2 coordinate skeletal muscle growth and metabolism via
the Akt and AMPK pathways. _Mol. Cell. Biol._ 31, 430–441 (2011). Article CAS PubMed Google Scholar * Laustsen, P. G. et al. Essential role of insulin and insulin-like growth factor 1
receptor signaling in cardiac development and function. _Mol. Cell. Biol._ 27, 1649–1664 (2007). Article CAS PubMed Google Scholar * Dong, X. et al. Irs1 and Irs2 signaling is essential
for hepatic glucose homeostasis and systemic growth. _J. Clin. Invest._ 116, 101–114 (2006). Article CAS PubMed Google Scholar * Guo, S. et al. The Irs1 branch of the insulin signaling
cascade plays a dominant role in hepatic nutrient homeostasis. _Mol. Cell. Biol._ 29, 5070–5083 (2009). Article CAS PubMed PubMed Central Google Scholar * Kubota, N. et al. Differential
hepatic distribution of insulin receptor substrates causes selective insulin resistance in diabetes and obesity. _Nat. Commun._ 7, 12977 (2016). Article CAS PubMed PubMed Central Google
Scholar * Manning, B. D. & Cantley, L. C. AKT/PKB signaling: navigating downstream. _Cell_ 129, 1261–1274 (2007). Article CAS PubMed PubMed Central Google Scholar * Dummler, B.
& Hemmings, B. A. Physiological roles of PKB/Akt isoforms in development and disease. _Biochem. Soc. Trans._ 35, 231 (2007). Article CAS PubMed Google Scholar * Gonzalez, E. &
McGraw, T. E. The Akt kinases: isoform specificity in metabolism and cancer. _Cell Cycle_ 8, 2502–2508 (2009). Article CAS PubMed PubMed Central Google Scholar * Manning, B. D. &
Toker, A. AKT/PKB Signaling: navigating the network. _Cell_ 169, 381–405 (2017). Article CAS PubMed PubMed Central Google Scholar * Zheng, X. & Cartee, G. D. Insulin-induced effects
on the subcellular localization of AKT1, AKT2 and AS160 in rat skeletal muscle. _Sci. Rep._ 6, 39230 (2016). Article CAS PubMed PubMed Central Google Scholar * Gonzalez, E. &
McGraw, T. E. Insulin-modulated Akt subcellular localization determines Akt isoform-specific signaling. _Proc. Natl Acad. Sci. USA_ 106, 7004–7009 (2009). Article CAS PubMed Google
Scholar * Osorio-Fuentealba, C. & Klip, A. Dissecting signalling by individual Akt/PKB isoforms, three steps at once. _Biochem. J._ 470, e13–e16 (2015). Article CAS PubMed Google
Scholar * Kajno, E., McGraw, T. E. & Gonzalez, E. Development of a new model system to dissect isoform specific Akt signalling in adipocytes. _Biochem. J._ 468, 425–434 (2015). Article
CAS PubMed PubMed Central Google Scholar * Kubota, H. et al. Temporal coding of insulin action through multiplexing of the AKT pathway. _Mol. Cell_ 46, 820–832 (2012). Article CAS
PubMed Google Scholar * Lefebvre, P. J., Paolisso, G., Scheen, A. J. & Henquin, J. C. Pulsatility of insulin and glucagon release: physiological significance and pharmacological
implications. _Diabetologia_ 30, 443–452 (1987). Article CAS PubMed Google Scholar * Kim, S. P. et al. Nocturnal free fatty acids are uniquely elevated in the longitudinal development of
diet-induced insulin resistance and hyperinsulinemia. _Am. J. Physiol. Endocrinol. Metab._ 292, E1590–E1598 (2007). Article CAS PubMed Google Scholar * Zhang, J. et al. Insulin inhibits
transcription of IRS-2 gene in rat liver through an insulin response element (IRE) that resembles IREs of other insulin-repressed genes. _Proc. Natl Acad. Sci._ 98, 3756–3761 (2001).
Article CAS PubMed Google Scholar * Hirashima, Y. et al. Insulin down-regulates insulin receptor substrate-2 expression through the phosphatidylinositol 3-kinase/Akt pathway. _J.
Endocrinol._ 179, 253–266 (2003). Article CAS PubMed Google Scholar * Ide, T. et al. SREBPs suppress IRS-2-mediated insulin signalling in the liver. _Nat. Cell Biol._ 6, 351–357 (2004).
Article CAS PubMed Google Scholar * Hanke, S. & Mann, M. The phosphotyrosine interactome of the insulin receptor family and its substrates IRS-1 and IRS-2. _Mol. Cell Proteomics_ 8,
519–534 (2009). Article CAS PubMed PubMed Central Google Scholar * Vinayagam, A. et al. An integrative analysis of the InR/PI3K/Akt network identifies the dynamic response to insulin
signaling. _Cell Rep._ 16, 3062–3074 (2016). Article CAS PubMed PubMed Central Google Scholar * Schmelzle, K., Kane, S., Gridley, S., Lienhard, G. E. & White, F. M. Temporal
dynamics of tyrosine phosphorylation in insulin signaling. _Diabetes_ 55, 2171–2179 (2006). Article CAS PubMed Google Scholar * Kruger, M. et al. Dissection of the insulin signaling
pathway via quantitative phosphoproteomics. _Proc. Natl Acad. Sci. USA_ 105, 2451–2456 (2008). Article PubMed Google Scholar * Humphrey, S. J. et al. Dynamic adipocyte phosphoproteome
reveals that Akt directly regulates mTORC2. _Cell Metab._ 17, 1009–1020 (2013). Article CAS PubMed PubMed Central Google Scholar * Humphrey, S. J., Azimifar, S. B. & Mann, M.
High-throughput phosphoproteomics reveals _in vivo_ insulin signaling dynamics. _Nat. Biotechnol._ 33, 990–995 (2015). REFERENCES 153 AND 154 USED MASS SPECTROMETRY TO IDENTIFY THE PROTEIN
RESIDUES THAT ARE PHOSPHORYLATED IN RESPONSE TO INSULIN, AS WELL AS THE TIMING OF THESE PHOSPHORYLATION EVENTS. Article CAS PubMed Google Scholar * Lauro, D. et al. Impaired glucose
tolerance in mice with a targeted impairment of insulin action in muscle and adipose tissue. _Nat. Genet._ 20, 294–298 (1998). Article CAS PubMed Google Scholar * Cushman, S. W. &
Wardzala, L. J. Potential mechanism of insulin action on glucose transport in the isolated rat adipose cell. Apparent translocation of intracellular transport systems to the plasma membrane.
_J. Biol. Chem._ 255, 4758–4762 (1980). CAS PubMed Google Scholar * Suzuki, K. & Kono, T. Evidence that insulin causes translocation of glucose transport activity to the plasma
membrane from an intracellular storage site. _Proc. Natl Acad. Sci. USA_ 77, 2542–2545 (1980). Article CAS PubMed Google Scholar * Foley, K., Boguslavsky, S. & Klip, A. Endocytosis,
recycling, and regulated exocytosis of glucose transporter 4. _Biochemistry_ 50, 3048–3061 (2011). Article CAS PubMed Google Scholar * Huang, S. & Czech, M. P. The GLUT4 glucose
transporter. _Cell Metab._ 5, 237–252 (2007). Article CAS PubMed Google Scholar * Klip, A., Sun, Y., Chiu, T. T. & Foley, K. P. Signal transduction meets vesicle traffic: the
software and hardware of GLUT4 translocation. _Am J. Cell Physiol._ 306, C879–C886 (2014). Article CAS Google Scholar * Leto, D. & Saltiel, A. R. Regulation of glucose transport by
insulin: traffic control of GLUT4. _Nat. Rev. Mol. Cell Biol._ 13, 383–396 (2012). Article CAS PubMed Google Scholar * Eguez, L. et al. Full intracellular retention of GLUT4 requires
AS160 Rab GTPase activating protein. _Cell Metab._ 2, 263–272 (2005). Article CAS PubMed Google Scholar * Miinea, C. P. et al. AS160, the Akt substrate regulating GLUT4 translocation,
has a functional Rab GTPase-activating protein domain. _Biochem. J._ 391, 87–93 (2005). Article CAS PubMed PubMed Central Google Scholar * Sano, H. et al. Insulin-stimulated
phosphorylation of a Rab GTPase-activating protein regulates GLUT4 translocation. _J. Biol. Chem._ 278, 14599–14602 (2003). Article CAS PubMed Google Scholar * Ramm, G., Larance, M.,
Guilhaus, M. & James, D. E. A role for 14-3-3 in insulin-stimulated GLUT4 translocation through its interaction with the RabGAP AS160. _J. Biol. Chem._ 281, 29174–29180 (2006). Article
CAS PubMed Google Scholar * Ishikura, S., Bilan, P. J. & Klip, A. Rabs 8A and 14 are targets of the insulin-regulated Rab-GAP AS160 regulating GLUT4 traffic in muscle cells. _Biochem.
Biophys. Res. Commun._ 353, 1074–1079 (2007). Article CAS PubMed Google Scholar * Sano, H. et al. Rab10, a target of the AS160 Rab GAP, is required for insulin-stimulated translocation
of GLUT4 to the adipocyte plasma membrane. _Cell Metab._ 5, 293–303 (2007). Article CAS PubMed Google Scholar * Vazirani, R. P. et al. Disruption of adipose Rab10-dependent insulin
signaling causes hepatic insulin resistance. _Diabetes_ 65, 1577–1589 (2016). Article CAS PubMed PubMed Central Google Scholar * Bruno, J., Brumfield, A., Chaudhary, N., Iaea, D. &
McGraw, T. E. SEC16A is a RAB10 effector required for insulin-stimulated GLUT4 trafficking in adipocytes. _J. Cell Biol._ 214, 61–76 (2016). Article CAS PubMed PubMed Central Google
Scholar * Uhm, M. et al. Phosphorylation of the exocyst protein Exo84 by TBK1 promotes insulin-stimulated GLUT4 trafficking. _Sci. Signal._ 10, eaah5085 (2017). Article CAS PubMed Google
Scholar * Lin, H. V. & Accili, D. Hormonal regulation of hepatic glucose production in health and disease. _Cell Metab._ 14, 9–19 (2011). Article CAS PubMed PubMed Central Google
Scholar * Matsumoto, M., Pocai, A., Rossetti, L., Depinho, R. A. & Accili, D. Impaired regulation of hepatic glucose production in mice lacking the forkhead transcription factor Foxo1
in liver. _Cell Metab._ 6, 208–216 (2007). Article CAS PubMed Google Scholar * Nakae, J., Kitamura, T., Silver, D. L. & Accili, D. The forkhead transcription factor Foxo1 (Fkhr)
confers insulin sensitivity onto glucose-6-phosphatase expression. _J. Clin. Invest._ 108, 1359–1367 (2001). Article CAS PubMed PubMed Central Google Scholar * Haeusler, R. A. et al.
Integrated control of hepatic lipogenesis versus glucose production requires FoxO transcription factors. _Nat. Commun._ 5, 5190 (2014). Article CAS PubMed PubMed Central Google Scholar
* Nakae, J. et al. The forkhead transcription factor Foxo1 regulates adipocyte differentiation. _Dev. Cell_ 4, 119–129 (2003). Article CAS PubMed Google Scholar * Plum, L. et al. The
obesity susceptibility gene Cpe links FoxO1 signaling in hypothalamic pro-opiomelanocortin neurons with regulation of food intake. _Nat. Med._ 15, 1195–1201 (2009). Article CAS PubMed
PubMed Central Google Scholar * Ren, H. et al. FoxO1 target Gpr17 activates AgRP neurons to regulate food intake. _Cell_ 149, 1314–1326 (2012). Article CAS PubMed PubMed Central Google
Scholar * Kitamura, T. et al. The forkhead transcription factor Foxo1 links insulin signaling to Pdx1 regulation of pancreatic β cell growth. _J. Clin. Invest._ 110, 1839–1847 (2002).
Article CAS PubMed PubMed Central Google Scholar * Kitamura, Y. I. et al. FoxO1 protects against pancreatic β cell failure through NeuroD and MafA induction. _Cell Metab._ 2, 153–163
(2005). Article CAS PubMed Google Scholar * Horton, J. D., Goldstein, J. L. & Brown, M. S. SREBPs: activators of the complete program of cholesterol and fatty acid synthesis in the
liver. _J. Clin. Invest._ 109, 1125–1131 (2002). Article CAS PubMed PubMed Central Google Scholar * Flier, J. S. & Hollenberg, A. N. ADD-1 provides major new insight into the
mechanism of insulin action. _Proc. Natl Acad. Sci. USA_ 96, 14191–14192 (1999). Article CAS PubMed Google Scholar * Owen, J. L. et al. Insulin stimulation of SREBP-1c processing in
transgenic rat hepatocytes requires p70 S6-kinase. _Proc. Natl Acad. Sci. USA_ 109, 16184–16189 (2012). Article CAS PubMed Google Scholar * Chen, G., Liang, G., Ou, J., Goldstein, J. L.
& Brown, M. S. Central role for liver X receptor in insulin-mediated activation of Srebp-1c transcription and stimulation of fatty acid synthesis in liver. _Proc. Natl Acad. Sci. USA_
101, 11245–11250 (2004). Article CAS PubMed Google Scholar * Hegarty, B. D. et al. Distinct roles of insulin and liver X receptor in the induction and cleavage of sterol regulatory
element binding protein-1c. _Proc. Natl Acad. Sci. USA_ 102, 791–796 (2005). Article CAS PubMed Google Scholar * Kim, J. B. et al. Nutritional and insulin regulation of fatty acid
synthetase and leptin gene expression through ADD1/SREBP1. _J. Clin. Invest._ 101, 1–9 (1998). Article CAS PubMed PubMed Central Google Scholar * Li, S., Brown, M. S. & Goldstein,
J. L. Bifurcation of insulin signaling pathway in rat liver: mTORC1 required for stimulation of lipogenesis, but not inhibition of gluconeogenesis. _Proc. Natl Acad. Sci. USA_ 107, 3441–3446
(2010). Article CAS PubMed Google Scholar * Nakae, J., Park, B. C. & Accili, D. Insulin stimulates phosphorylation of the forkhead transcription factor FKHR on serine 253 through a
Wortmannin-sensitive pathway. _J. Biol. Chem._ 274, 15982–15985 (1999). Article CAS PubMed Google Scholar * Brunet, A. et al. Akt promotes cell survival by phosphorylating and inhibiting
a Forkhead transcription factor. _Cell_ 96, 857–868 (1999). Article CAS PubMed Google Scholar * Biggs, W. H. III., Meisenhelder, J., Hunter, T., Cavenee, W. K. & Arden, K. C.
Protein kinase B/Akt-mediated phosphorylation promotes nuclear exclusion of the winged helix transcription factor FKHR1. _Proc. Natl Acad. Sci. USA_ 96, 7421–7426 (1999). Article CAS
PubMed Google Scholar * Haas, J. T. et al. Hepatic insulin signaling is required for obesity-dependent expression of SREBP-1c mRNA but not for feeding-dependent expression. _Cell Metab._
15, 873–884 (2012). Article CAS PubMed PubMed Central Google Scholar * Shimomura, I. et al. Decreased IRS-2 and increased SREBP-1c lead to mixed insulin resistance and sensitivity in
livers of lipodystrophic and ob/ob mice. _Mol. Cell_ 6, 77–86 (2000). Article CAS PubMed Google Scholar * Waters, K. M. & Ntambi, J. M. Insulin and dietary fructose induce
stearoyl-CoA desaturase 1 gene expression of diabetic mice. _J. Biol. Chem._ 269, 27773–27777 (1994). CAS PubMed Google Scholar * Paulauskis, J. D. & Sul, H. S. Hormonal regulation of
mouse fatty acid synthase gene transcription in liver. _J. Biol. Chem._ 264, 574–577 (1989). CAS PubMed Google Scholar * Peterson, T. R. et al. mTOR complex 1 regulates lipin 1
localization to control the SREBP pathway. _Cell_ 146, 408–420 (2011). Article CAS PubMed PubMed Central Google Scholar * Han, J. et al. The CREB coactivator CRTC2 controls hepatic
lipid metabolism by regulating SREBP1. _Nature_ 524, 243–246 (2015). REFERENCES 194 AND 195 OFFERED TWO MECHANISMS TO EXPLAIN THE POST-TRANSLATIONAL ACTIVATION OF SREBP1C BY INSULIN, A
PHENOMENON THAT HAD PREVIOUSLY BEEN POORLY UNDERSTOOD. Article CAS PubMed Google Scholar * Jensen, M. & De Meyts, P. Molecular mechanisms of differential intracellular signaling from
the insulin receptor. _Vitam. Horm._ 80, 51–75 (2009). Article CAS PubMed Google Scholar * Bergeron, J. J., Di Guglielmo, G. M., Dahan, S., Dominguez, M. & Posner, B. I. Spatial and
temporal regulation of receptor tyrosine kinase activation and intracellular signal transduction. _Annu. Rev. Biochem._ 85, 573–597 (2016). Article CAS PubMed Google Scholar * Nakae,
J., Kido, Y. & Accili, D. Distinct and overlapping functions of insulin and IGF-I receptors. _Endocr. Rev._ 22, 818–835 (2001). Article CAS PubMed Google Scholar * Schmidt, V. et al.
SORLA facilitates insulin receptor signaling in adipocytes and exacerbates obesity. _J. Clin. Invest._ 126, 2706–2720 (2016). Article PubMed PubMed Central Google Scholar * Smith, E. N.
et al. Longitudinal genome-wide association of cardiovascular disease risk factors in the Bogalusa heart study. _PLoS Genet._ 6, e1001094 (2010). Article CAS PubMed PubMed Central
Google Scholar * Parks, Brian, W. et al. Genetic control of obesity and gut microbiota composition in response to high-fat, high-sucrose diet in mice. _Cell Metab._ 17, 141–152 (2013).
Article CAS Google Scholar * Lampson, M. A., Racz, A., Cushman, S. W. & McGraw, T. E. Demonstration of insulin-responsive trafficking of GLUT4 and vpTR in fibroblasts. _J. Cell Sci._
113, 4065–4076 (2000). CAS PubMed Google Scholar * Ross, S. A., Herbst, J. J., Keller, S. R. & Lienhard, G. E. Trafficking kinetics of the insulin-regulated membrane aminopeptidase in
3T3-L1 adipocytes. _Biochem. Biophys. Res. Commun._ 239, 247–251 (1997). Article CAS PubMed Google Scholar * Keller, S. R., Davis, A. C. & Clairmont, K. B. Mice deficient in the
insulin-regulated membrane aminopeptidase show substantial decreases in glucose transporter GLUT4 levels but maintain normal glucose homeostasis. _J. Biol. Chem._ 277, 17677–17686 (2002).
Article CAS PubMed Google Scholar * Screaton, R. A. et al. The CREB coactivator TORC2 functions as a calcium- and cAMP-sensitive coincidence detector. _Cell_ 119, 61–74 (2004). Article
CAS PubMed Google Scholar * Dentin, R. et al. Insulin modulates gluconeogenesis by inhibition of the coactivator TORC2. _Nature_ 449, 366–369 (2007). Article CAS PubMed Google Scholar
* Ozcan, L. et al. Calcium signaling through CaMKII regulates hepatic glucose production in fasting and obesity. _Cell Metab._ 15, 739–751 (2012). Article CAS PubMed PubMed Central
Google Scholar * Kawamori, D. et al. The forkhead transcription factor Foxo1 bridges the JNK pathway and the transcription factor PDX-1 through its intracellular translocation. _J. Biol.
Chem._ 281, 1091–1098 (2006). Article CAS PubMed Google Scholar * Martinez, S. C. et al. Inhibition of Foxo1 protects pancreatic islet β-cells against fatty acid and endoplasmic
reticulum stress-induced apoptosis. _Diabetes_ 57, 846–859 (2008). Article CAS PubMed Google Scholar * Frescas, D., Valenti, L. & Accili, D. Nuclear trapping of the forkhead
transcription factor FoxO1 via Sirt-dependent deacetylation promotes expression of glucogenetic genes. _J. Biol. Chem._ 280, 20589–20595 (2005). Article CAS PubMed Google Scholar *
Qiang, L., Banks, A. S. & Accili, D. Uncoupling of acetylation from phosphorylation regulates FOXO1 function independent of its sub-cellular localization. _J. Biol. Chem._ 285,
27396–27401 (2010). Article CAS PubMed PubMed Central Google Scholar * Banks, A. S. et al. Dissociation of the glucose and lipid regulatory functions of FoxO1 by targeted knockin of
acetylation-defective alleles in mice. _Cell Metab._ 14, 587–597 (2011). Article CAS PubMed PubMed Central Google Scholar * Tsuchiya, K. et al. Homozygosity for an allele encoding
deacetylated FoxO1 protects macrophages from cholesterol-induced inflammation without increasing apoptosis. _Arterioscler. Thromb. Vasc. Biol._ 31, 2920–2928 (2011). Article CAS PubMed
PubMed Central Google Scholar * Qiang, L. et al. Increased atherosclerosis and endothelial dysfunction in mice bearing constitutively deacetylated alleles of Foxo1 gene. _J. Biol. Chem._
287, 13944–13951 (2012). Article CAS PubMed PubMed Central Google Scholar * Betz, C. & Hall, M. N. Where is mTOR and what is it doing there? _J. Cell Biol._ 203, 563–574 (2013).
Article CAS PubMed PubMed Central Google Scholar * Sancak, Y. et al. Ragulator-Rag complex targets mTORC1 to the lysosomal surface and is necessary for its activation by amino acids.
_Cell_ 141, 290–303 (2010). Article CAS PubMed PubMed Central Google Scholar * Inoki, K., Li, Y., Xu, T. & Guan, K.-L. Rheb GTPase is a direct target of TSC2 GAP activity and
regulates mTOR signaling. _Genes Dev._ 17, 1829–1834 (2003). Article CAS PubMed PubMed Central Google Scholar * Inoki, K., Li, Y., Zhu, T., Wu, J. & Guan, K.-L. TSC2 is
phosphorylated and inhibited by Akt and suppresses mTOR signalling. _Nat. Cell Biol._ 4, 648–657 (2002). Article CAS PubMed Google Scholar * Potter, C. J., Pedraza, L. G. & Xu, T.
Akt regulates growth by directly phosphorylating Tsc2. _Nat. Cell Biol._ 4, 658–665 (2002). Article CAS PubMed Google Scholar * Menon, S. et al. Spatial control of the TSC complex
integrates insulin and nutrient regulation of mTORC1 at the lysosome. _Cell_ 156, 771–785 (2014). THIS ARTICLE DEMONSTRATED THAT INSULIN REGULATES MTORC1 ACTIVITY BY CONTROLLING THE SPATIAL
DISTRIBUTION OF THE TSC COMPLEX. Article CAS PubMed PubMed Central Google Scholar * Phillips, M. J. & Voeltz, G. K. Structure and function of ER membrane contact sites with other
organelles. _Nat. Rev. Mol. Cell Biol._ 17, 69–82 (2016). Article CAS PubMed Google Scholar * Rutter, G. A. & Pinton, P. Mitochondria-associated endoplasmic reticulum membranes in
insulin signaling. _Diabetes_ 63, 3163–3165 (2014). Article CAS PubMed Google Scholar * Giorgi, C. et al. PML regulates apoptosis at endoplasmic reticulum by modulating calcium release.
_Science_ 330, 1247–1251 (2010). Article CAS PubMed PubMed Central Google Scholar * Betz, C. et al. mTOR complex 2-Akt signaling at mitochondria-associated endoplasmic reticulum
membranes (MAM) regulates mitochondrial physiology. _Proc. Natl Acad. Sci._ 110, 12526–12534 (2013). Article CAS PubMed Google Scholar * Tubbs, E. et al. Mitochondria-associated
endoplasmic reticulum membrane (MAM) integrity is required for insulin signaling and is implicated in hepatic insulin resistance. _Diabetes_ 63, 3279–3294 (2014). Article CAS PubMed
Google Scholar * Sarbassov, D. D., Guertin, D. A., Ali, S. M. & Sabatini, D. M. Phosphorylation and Regulation of Akt/PKB by the Rictor-mTOR Complex. _Science_ 307, 1098–1101 (2005).
Article CAS PubMed Google Scholar * Sebastian, D. et al. Mitofusin 2 (Mfn2) links mitochondrial and endoplasmic reticulum function with insulin signaling and is essential for normal
glucose homeostasis. _Proc. Natl Acad. Sci. USA_ 109, 5523–5528 (2012). Article CAS PubMed Google Scholar * Arruda, A. P. et al. Chronic enrichment of hepatic endoplasmic
reticulum-mitochondria contact leads to mitochondrial dysfunction in obesity. _Nat. Med._ 20, 1427–1435 (2014). Article CAS PubMed PubMed Central Google Scholar * Hijmans, B. S.,
Grefhorst, A., Oosterveer, M. H. & Groen, A. K. Zonation of glucose and fatty acid metabolism in the liver: mechanism and metabolic consequences. _Biochimie_ 96, 121–129 (2014). Article
CAS PubMed Google Scholar * Lee, W. L. & Klip, A. Endothelial transcytosis of insulin: does it contribute to insulin resistance? _Physiology (Bethesda)_ 31, 336–345 (2016). CAS
Google Scholar * Rask-Madsen, C. & Kahn, C. R. Tissue-specific insulin signaling, metabolic syndrome, and cardiovascular disease. _Arterioscler. Thromb. Vasc. Biol._ 32, 2052–2059
(2012). Article CAS PubMed PubMed Central Google Scholar * King, G. & Johnson, S. Receptor-mediated transport of insulin across endothelial cells. _Science_ 227, 1583–1586 (1985).
Article CAS PubMed Google Scholar * Wang, H., Liu, Z., Li, G. & Barrett, E. J. The vascular endothelial cell mediates insulin transport into skeletal muscle. _Am. J. Physiol.
Endocrinol. Metab._ 291, E323–E332 (2006). Article CAS PubMed Google Scholar * Vicent, D. et al. The role of endothelial insulin signaling in the regulation of vascular tone and insulin
resistance. _J. Clin. Invest._ 111, 1373–1380 (2003). Article CAS PubMed PubMed Central Google Scholar * Kubota, T. et al. Impaired insulin signaling in endothelial cells reduces
insulin-induced glucose uptake by skeletal muscle. _Cell Metab._ 13, 294–307 (2011). Article CAS PubMed Google Scholar * Tsuchiya, K. & Accili, D. Liver sinusoidal endothelial cells
link hyperinsulinemia to hepatic insulin resistance. _Diabetes_ 62, 1478–1489 (2013). Article CAS PubMed PubMed Central Google Scholar * Pajvani, U. B. et al. Inhibition of Notch
signaling ameliorates insulin resistance in a FoxO1-dependent manner. _Nat. Med._ 17, 961–967 (2011). Article CAS PubMed PubMed Central Google Scholar * Pajvani, U. B. et al. Inhibition
of Notch uncouples Akt activation from hepatic lipid accumulation by decreasing mTorc1 stability. _Nat. Med._ (2013). * Bi, P. & Kuang, S. Notch signaling as a novel regulator of
metabolism. _Trends Endocrinol. Metab._ 26, 248–255 (2015). Article CAS PubMed PubMed Central Google Scholar * Titchenell, P. M., Lazar, M. A. & Birnbaum, M. J. Unraveling the
regulation of hepatic metabolism by insulin. _Trends Endocrinol. Metab._ (2017). * Mueckler, M. Family of glucose-transporter genes. Implications for glucose homeostasis and diabetes.
_Diabetes_ 39, 6–11 (1990). Article CAS PubMed Google Scholar * Thorens, B., Charron, M. J. & Lodish, H. F. Molecular physiology of glucose transporters. _Diabetes Care_ 13, 209–218
(1990). Article CAS PubMed Google Scholar * Cross, D. A., Alessi, D. R., Cohen, P., Andjelkovich, M. & Hemmings, B. A. Inhibition of glycogen synthase kinase-3 by insulin mediated by
protein kinase B. _Nature_ 378, 785–789 (1995). Article CAS PubMed Google Scholar * Scott, P. H., Brunn, G. J., Kohn, A. D., Roth, R. A. & Lawrence, J. C. Jr. Evidence of
insulin-stimulated phosphorylation and activation of the mammalian target of rapamycin mediated by a protein kinase B signaling pathway. _Proc. Natl Acad. Sci. USA_ 95, 7772–7777 (1998).
Article CAS PubMed Google Scholar * Kitamura, T. et al. Forkhead protein FoxO1 mediates Agrp-dependent effects of leptin on food intake. _Nat. Med._ 12, 534–540 (2006). Article CAS
PubMed Google Scholar Download references ACKNOWLEDGEMENTS The authors thank U. Pajvani and R. Leibel for stimulating discussions and helpful comments. Supported by NIH grants DK57539,
DK64819, DK58282, HL81723, DK52852 and HL125649. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Pathology and Cell Biology, Columbia University College of Physicians and
Surgeons, New York, 10032, New York, USA Rebecca A. Haeusler * Departments of Biochemistry and Cardiothoracic Surgery, Weill Cornell Medicine, New York, 10065, New York, USA Timothy E.
McGraw * Department of Medicine, Columbia University College of Physicians & Surgeons, New York, 10032, New York, USA Domenico Accili Authors * Rebecca A. Haeusler View author
publications You can also search for this author inPubMed Google Scholar * Timothy E. McGraw View author publications You can also search for this author inPubMed Google Scholar * Domenico
Accili View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS R.A.H., T.E.M. and D.A. researched data for the article, contributed to discussion
of the content, wrote the article and reviewed and/or edited the manuscript before submission. CORRESPONDING AUTHOR Correspondence to Domenico Accili. ETHICS DECLARATIONS COMPETING INTERESTS
The authors declare no competing financial interests. POWERPOINT SLIDES POWERPOINT SLIDE FOR FIG. 1 POWERPOINT SLIDE FOR FIG. 2 POWERPOINT SLIDE FOR FIG. 3 POWERPOINT SLIDE FOR FIG. 4
POWERPOINT SLIDE FOR FIG. 5 GLOSSARY * Anorexigenic Appetite-suppressant. * Paracrine A mechanism by which neighbouring cells influence each other by way of a secreted factor. *
Diacylglycerol A glycerol molecule with two fatty acid chains present in food or produced primarily in the liver, adipose tissue and intestine, diacylglycerol is best known for its
signalling properties to activate protein kinase C but also functions as a precursor molecule in the synthesis of triglycerides and prostaglandins. * Haploinsufficiency A phenotype caused by
a heterozygous loss-of-function mutation, or by a mutation partly affecting levels and/or activity of a gene product. * Post-absorptive state The state following food absorption by the gut,
hence the fasting state. * RABGAP A protein activating the GTPase activity of RAB, a component of secretory vesicles involved in intracellular transport. * Exocyst An octamer assembled to
promote intracellular vesicle transport. * COPII complex A complex of proteins assembled around coat protein II (COPII), required for anterograde transport from the endoplasmic reticulum to
the Golgi. * Transcytocis The transport of proteins across the interior of a cell. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Haeusler, R., McGraw,
T. & Accili, D. Biochemical and cellular properties of insulin receptor signalling. _Nat Rev Mol Cell Biol_ 19, 31–44 (2018). https://doi.org/10.1038/nrm.2017.89 Download citation *
Published: 04 October 2017 * Issue Date: January 2018 * DOI: https://doi.org/10.1038/nrm.2017.89 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this
content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
